Abstract
There is emerging but limited data assessing single-port (SP) robot-assisted surgery as an alternative to multi-port (MP) platforms. We compared perioperative outcomes between SP and MP robot-assisted approaches for excision of high and low complexity renal masses. Retrospective chart review was performed for patients undergoing robot-assisted partial or radical nephrectomy using the SP surgical system (n = 23) at our institution between November 2019 and November 2021. Renal masses were categorized as high complexity (7+) or low complexity (4–6) using the R.E.N.A.L. nephrometry scoring system. Adjusting for baseline characteristics, patients were matched using a prospectively maintained MP database in a 2:1 (MP:SP) ratio. For high complexity tumors (n = 12), SP surgery was associated with a significantly longer operative time compared to MP (248.4 vs 188.1 min, p = 0.02) but a significantly shorter length of stay (1.9 vs 2.8 days, p = 0.02). For low complexity tumors (n = 11), operative time (177.7 vs 161.4 min, p = 0.53), estimated blood loss (69.6.0 vs 142.0 mL, p = 0.62), and length of stay (1.6 vs 1.8 days, p = 0.528) were comparable between SP and MP approaches. Increasing nephrometry score was associated with a greater relative increase in operative time for SP compared to MP renal surgery (p = 0.07) using best of fit linear modeling. SP robot-assisted partial and radical nephrectomy is safe and feasible for low complexity renal masses. For high complexity renal masses, the SP system is associated with a significantly longer operative time compared to the MP technique. Careful consideration should be given when selecting patients for SP robot-assisted kidney surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robot-assisted partial nephrectomy (RAPN) is the standard approach for the extirpative treatment of small renal masses. Compared to radical nephrectomy, partial nephrectomy provides similar oncological outcomes while producing better functional outcomes [1,2,3]. Although RAPN is commonly performed with a conventional multi-port (MP) robot, the single-port (SP) system has been introduced with increasing adoption [4]. Recent reports have demonstrated similar perioperative outcomes for SP and MP systems for RAPN [5], including potential benefits such as shorter hospital stay [6, 7]. Beyond RAPN, higher rates of same-day discharge for SP systems have been observed in robot-assisted prostatectomy, pyeloplasty, nephrectomy, adrenalectomy, and partial cystectomy [6]. However, another study comparing SP versus MP robot-assisted prostatectomy found that despite shorter hospital stay and decreased hospitalization expenses for SP prostatectomy, overall costs for MP and SP procedures were comparable due to higher cost of consumable materials with the SP platform [8].
Despite increasing literature on SP-RAPN since the initial series report in 2019 [9], further study regarding the feasibility of the da Vinci Single Port® robotic surgical system (Intuitive Surgical, Sunnyvale, CA) as an alternative to conventional MP robotic platforms is needed. There remains a paucity of data regarding the safety and efficacy of SP systems as case complexity increases. RAPN case complexity and perioperative outcomes are known to be associated with anatomic complexity of the renal mass, as characterized by the R.E.N.A.L. nephrometry score system that accounts for tumor radius, endophytic/exophytic growth, nearness to collecting system or sinus, anterior/posterior aspect, and location relative to the polar line [10, 11]. Therefore, we sought to compare perioperative outcomes between SP and MP robot-assisted partial or radical nephrectomy for high versus low complexity renal masses as determined by the R.E.N.A.L. nephrometry score, using propensity score matching to account for patient- and tumor-related factors.
Patients and methods
Patient selection
With Institutional Review Board approval, we performed a retrospective chart review of all patients receiving SP robot-assisted partial or radical nephrectomy by three surgeons from November 2019—at time of adoption of SP system at our institution—until November 2021. Informed consent was obtained from all patients including discussion of risks regarding SP robot-assisted surgery and the possible need for conversion to conventional robotic, laparoscopic, or open approaches. Qualifying patients were then matched in a 2:1 (MP:SP) fashion to patients from our prospectively maintained MP robot-assisted nephrectomy database (which includes robot-assisted partial and radical nephrectomy) using propensity score matching. Both datasets allowed extraction of patient demographics, preoperative imaging, operative approaches, and perioperative outcomes. Propensity score matching was performed based on clinical factors, including patient body mass index (BMI), renal mass size, and partial versus radical nephrectomy. Most importantly, patients were matched for renal mass complexity based on their R.E.N.A.L. nephrometry score group (low or high complexity). Our final study cohort consisted of 69 patients (SP = 23 and MP = 46).
Surgical technique
For all approaches the patient was placed in the lateral decubitus position with the table flexed.
SP transperitoneal approach was performed by first obtaining access to the peritoneal cavity using a Hasson technique in the paramedian area of the lower quadrant abdomen. Once access was obtained, the 25 mm multichannel SP robotic port was docked through a GelPOINT® access system (Applied Medical, Rancho Santa Margarita, CA), and a 12 mm AirSeal® access port (ConMed, Largo, FL) was used as an assistant port in a “plus-one” fashion. Typically, the assistant port was placed medial and superior to the SP robotic port.
SP retroperitoneal approach was performed by making an incision off the tip of the 12th rib and entering the retroperitoneal cavity similar to our initial entry for retroperitoneal MP robot-assisted surgery [12]. Once the retroperitoneal space was dissected using a balloon dilator, the 25 mm multichannel SP robotic port was docked through a GelPOINT® access system, and a 12 mm AirSeal® access port was used as an assistant port in a “plus-one” fashion. Typically, the assistant port was placed inferior and medial to the SP robotic port, over the iliac crest.
Our technique for transperitoneal and retroperitoneal MP-RAPN has been described previously [13]. Briefly, MP transperitoneal approach was performed with initial Veress needle access and the placement of four robotic trocars trocars along the paramedian line, starting one fingerbreadth below the costal margin with each a minimum of 8 cm apart. A 12 mm AirSeal® access port was used as an assistant port and placed in the midline. MP retroperitoneal approach was performed with an initial incision off of the tip of the 12th rib and entering the retroperitoneal cavity digitally. The retroperitoneal space was dissected using a balloon dilator and an additional robotic trocar was placed at the costovertebral angle. The peritoneum was mobilized bluntly, and two additional robotic trocars were placed medially collinear with the previously placed robotic trocars. A 12 mm AirSeal® access port was used as an assistant port and placed above the iliac crest in the mid-axillary line.
Statistical analysis
All patients were stratified by their R.E.N.A.L. nephrometry score. We defined scores 4–6 as “low complexity” and scores 7–12 as “high complexity” for the purpose of this study. Primary outcome variables included operative time, estimated blood loss (EBL), positive surgical margins, length of hospital stay (LOS), warm ischemia time, postoperative estimated glomerular filtration rate (eGFR), and postoperative complications.
Mean values for perioperative outcomes were stratified to low or high complexity groups prior to comparison between SP and MP systems. Best of fit linear modeling was used to evaluate operative time at each nephrometry score. Mann–Whitney U tests and Chi-square tests were used to determine significant associations between SP and MP systems and variables of interest for continuous and categorical variables, respectively. All analysis was completed using R version 4.1.0. Statistical significance was set at p < 0.05.
Results
Baseline study population characteristics were not significantly different between SP and MP groups and are summarized in Table 1. Retroperitoneal approach was utilized in 34.7% (8/23) of SP and 19.6% (9/46) of MP cases. There were zero radical nephrectomies in the low complexity groups, and in the high complexity groups 3/12 (25%) SP and 6/24 (25%) MP patients underwent radical nephrectomy. There were no operative conversions from partial to radical nephrectomy or from robot-assisted to pure laparoscopic or open surgery in any group.
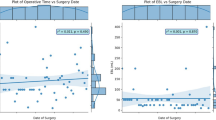
Table 2 summarizes perioperative outcomes of the SP and MP groups. For high complexity tumors, the SP approach was associated with a significantly longer average operative time compared to MP (248.4 ± 75.0 min vs 188.1 ± 61.0 min, p = 0.02). While not statistically significant, increasing nephrometry score trended toward a greater relative increase in operative time for SP compared to MP renal surgery (p = 0.07) using best of fit linear modeling (Fig. 1). Warm ischemia time was also significantly greater in the high complexity SP group compared to MP (50.0 ± 14.1 min vs 23.7 ± 7.5 min, p = 0.04). Conversely, SP patients had a significantly shorter LOS (1.9 ± 1.4 days vs 2.8 ± 1.9 days, p = 0.02). SP cases trended towards higher average EBL (410.0 ± 669.9 mL vs 171.2 ± 136.0 mL, p = 0.62), and a higher percentage of SP procedures utilized an off-clamp excisional technique compared to MP (77.8% vs 38.9%, p = 0.10). The SP group trended towards a higher positive surgical margin rate (25.0% vs 12.5%, p = 0.38) compared to MP. The final pathologic stage distribution between SP and MP was comparable (p = 0.71). There was no significant difference in eGFR percent change between SP and MP groups (− 18.1% ± 14.8% vs − 14.2% ± 28.8%, p = 0.92).
For low complexity tumors, there was no significant difference in operative time (177.7 ± 53.9 min vs 161.4 ± 41.9 min, p = 0.53), average EBL (69.6.0 ± 33.0 mL vs 142.0 ± 168.6 mL, p = 0.62), positive margins (9.1% vs 4.5%, p = 1.00), final pathologic stage distribution, or LOS (1.6 ± 1.0 days vs 1.8 ± 1.0 days, p = 0.53) between SP and MP techniques. There was one clamped procedure in the SP group (warm ischemia time of 49 min), while a significantly higher percentage of MP procedures utilized a clamped excisional technique (50% vs 9.1%, p = 0.03). Mean warm ischemia time for the MP group was 16.1 ± 6.7 min. There was a significantly smaller percent change in eGFR in the SP group compared to the MP group (− 0.7% ± 25.3% vs − 17.2% ± 21.3%, p = 0.017).
Clavien-Dindo II or greater complications occurred in 13.0% (3/23) of SP and 15.2% (7/46) of MP cases.
Discussion
In this study, we present a comparison between SP and MP robot-assisted renal surgery stratified by renal mass complexity. SP renal surgery in high complexity tumors (R.E.N.A.L. nephrometry score ≥ 7) was associated with a significantly longer average operative time compared to MP surgery; however, there was no significant difference for low complexity tumors (nephrometry score = 4–6). Although a trend was noted, best-of-fit linear modeling of operative time was not statistically different between SP and MP as nephrometry score increased. We also evaluated EBL, positive surgical margin rates, and perioperative complication rates and found no statistically significant differences between SP and MP platforms for both low and high complexity masses. There was no difference in LOS between SP and MP for low complexity masses; however, we found LOS to be nearly a full day shorter for SP patients with high complexity masses, a statistically significant reduction. There were no significant differences in baseline comorbidities between SP and MP patients to suggest a compelling influence on the significant reduction in LOS for high complexity SP patients. Collectively, these findings suggest that SP robot-assisted extirpative surgery provides comparable perioperative outcomes to the MP approach for low complexity renal masses. For the treatment of high complexity renal masses, the SP system may be associated with longer operative time but shorter post-operative hospital stay.
Our findings add to a collection of recent studies on RAPN that have shown increased operative time for high complexity cases, as indicated by an increasing nephrometry score [14]. Okhawere et al. reported shorter operative times in an SP cohort compared to an MP cohort for high complexity (nephrometry score = 10–12) renal masses, as well as shorter operative times in a high complexity SP group compared to low and intermediate complexity SP groups [15]. We, on the other hand, observed a trend toward increased operative times as complexity increased for both SP and MP approaches, as well as a statistically significant increase in operative time with the SP platform for high complexity masses. Besides utilizing different nephrometry score cut-offs, Okhawere and colleagues also collected data from nine centers with some centers contributing only SP or only MP cases. This may be cofounded by varying degrees of experience with the SP platform at different centers. At our institution, during the early stages of SP system implementation, trainees invariably had less SP experience compared to MP, which may have led to the observed higher operative times in complex SP cases. Similarly, high-volume MP surgeons were early in the SP learning curve during our study timeframe, and the need to learn an intricate SP system may have factored into longer operative times for complex cases compared to the MP system.
Other observed outcomes in the present study are consistent with those reported in the literature. In a single-institution retrospective chart review comparing SP-RAPN to MP-RAPN, Palacios et al. found no statistically significant differences in EBL, positive margin rate, and postoperative complication rate. We observed similar findings. They reported a mean LOS of 2.5 days with a 1-day shorter stay for SP-RAPN patients compared to MP-RAPN patients [16]. Our LOS findings for SP versus MP in high complexity masses support these results. While fewer incisions may be a factor in shorter LOS for high complexity SP cases, (1) we did not observe a similar difference in low complexity cases, and (2) our study timeline overlapped the COVID-19 pandemic, which has been associated with significantly higher rates of same-day discharge after robot-assisted urologic surgery [17, 18]. Other recent studies have noted decreased operative time and EBL for retroperitoneal MP-RAPN compared to the transperitoneal approach [19, 20]. Our cohort featured a higher percentage of retroperitoneal approaches for both SP groups compared to MP groups, but we did not observe decreased operative time nor EBL.
Generally, RAPN has been shown to have lower morbidity and achieve similar short-term functional outcomes compared to open surgery [21]. Therefore, if SP systems can preserve the low morbidity and short-term outcomes demonstrated by RAPN, it may be offered as a potentially less invasive option for patients. Previous investigators have noted their initial clinical experiences implementing this new system, reporting its safety in a variety of urological procedures, feasibility in managing cortical renal masses, and ideally a continued minimization of invasiveness of robot-assisted surgery [9, 22,23,24,25]. More recently, reassuring data has suggested similar perioperative outcomes for SP and MP systems for partial nephrectomy, among other procedures [5, 6]. Our study was consistent regarding feasibility, safety, and perioperative outcomes of SP surgical systems. Specifically, we report similar EBL and surgical margin positivity rates, and operative time was comparable for low complexity renal masses. These findings suggest that SP surgical systems are safe for robot-assisted kidney surgery and careful selection should be performed when planning an operative approach early in the learning curve. When deciding to utilize the SP platform for complicated masses, surgeons should consider these factors, being mindful that increased time in the operating room may adversely impact costs of the procedure, lead to higher blood loss or complications, and negate any potential decrease in LOS. Including these metrics in future study may further aid in developing guidelines for how to build an SP robotic practice in a stepwise approach.
Our study is not without limitations. The retrospective design is susceptible to selection bias since it is inherently difficult to capture why certain patients underwent SP-RAPN as opposed to MP-RAPN. We attempted to minimize selection bias with propensity score matching. The number of differences between each surgical case such as partial vs radical nephrectomy, surgeon/trainee involvement, and transperitoneal vs retroperitoneal approach are difficult to minimize due to the retrospective nature of the study. For example, it is difficult to compare mean ischemia time as most SP procedures were performed off-clamp. Trends that were noted, but did not reach statistical significance, might be better evaluated with a larger study population to strengthen the power of the relationships we examined. While our study compares SP and MP data from a single institution, thereby limiting study size and population heterogeneity, it allows comparison of SP and MP procedures performed by the same surgeons, limiting the impact of surgeon- and site-specific factors. Nonetheless, multi-institutional data will be critical to validate the results of this study. Furthermore, as SP usage continues to evolve, many surgeons have modified techniques not utilized at our institution during the study timeframe, including eliminating “plus-one” and the usage of a balloon dilator. These and future modifications to the SP approach have the potential to improve both operative time and cost, which could positively impact outcomes. Lastly, we do not routinely track trainee console time or docking time—doing so may reveal factors associated with our higher operative times for high complexity SP cases. The strength of our study lies in the nephrometry score stratification used to compare perioperative outcomes of SP and MP partial and radical nephrectomy.
Conclusion
In patients undergoing partial or radical nephrectomy utilizing the SP surgical system with high complexity renal tumors, we found a significant increase in operative time but a significant decrease in hospital LOS. As this study represents the early stages of implementation of this new technology, our experience and analysis suggest that others seeking to initiate SP approaches may benefit from focusing on low complexity tumors initially. We hope that our findings can aid in the decision-making process for urologic surgeons in determining the optimal surgical candidates for the SP platform during their learning curve.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Washington University School of Medicine in St. Louis.
References
Campbell SC, Clark PE, Chang SS, Karam JA, Souter L, Uzzo RG (2021) Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: part I. J Urol 206(2):199–208
Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A et al (2011) A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol 59(4):543–552
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H (2014) Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol 65(2):372–377
Dobbs RW, Halgrimson WR, Talamini S, Vigneswaran HT, Wilson JO, Crivellaro S (2020) Single-port robotic surgery: the next generation of minimally invasive urology. World J Urol 38(4):897–905
Glaser ZA, Burns ZR, Fang AM, Saidian A, Magi-Galluzzi C, Nix JW et al (2022) Single- versus multi-port robotic partial nephrectomy: a comparative analysis of perioperative outcomes and analgesic requirements. J Robot Surg 16(3):695–703
Abaza R, Murphy C, Bsatee A, Brown DH Jr, Martinez O (2021) Single-port robotic surgery allows same-day discharge in majority of cases. Urology 148:159–165
Francavilla S, Abern MR, Dobbs RW, Vigneswaran HT, Talamini S, Antonelli A et al (2022) Single-Port robot assisted partial nephrectomy: initial experience and technique with the da Vinci Single-Port platform (IDEAL Phase 1). Minerva Urol Nephrol 74(2):216–224
Lenfant L, Sawczyn G, Kim S, Aminsharifi A, Kaouk J (2021) Single-institution cost comparison: single-port versus multiport robotic prostatectomy. Eur Urol Focus 7(3):532–536
Kaouk J, Garisto J, Eltemamy M, Bertolo R (2019) Pure single-site robot-assisted partial nephrectomy using the sp surgical system: initial clinical experience. Urology 124:282–285
Kutikov A, Uzzo RG (2009) The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 182(3):844–53
Schiavina R, Novara G, Borghesi M, Ficarra V, Ahlawat R, Moon DA et al (2017) PADUA and R.E.N.A.L. nephrometry scores correlate with perioperative outcomes of robot-assisted partial nephrectomy: analysis of the Vattikuti Global Quality Initiative in Robotic Urologic Surgery (GQI-RUS) database. BJU Int. 119(3):456–63
Johnson MH, Mobley JM, Figenshau RS (2013) Retroperitoneal access for robot-assisted renal surgery. Videourology 27(4)
Kim EH, Larson JA, Potretzke AM, Hulsey NK, Bhayani SB, Figenshau RS (2015) Retroperitoneal robot-assisted partial nephrectomy for posterior renal masses is associated with earlier hospital discharge: a single-institution retrospective comparison. J Endourol 29(10):1137–1142
Krishnan NK, Zappia J, Calaway AC, Nagle RT, Sundaram CP, Boris RS (2022) Identifying preoperative predictors of operative time and their impact on outcomes in robot-assisted partial nephrectomy. J Endourol 36(1):71–76
Okhawere KE, Beksac AT, Wilson MP, Korn TG, Meilika KN, Harrison R et al (2022) A propensity-matched comparison of the perioperative outcomes between single-port and multi-port robotic assisted partial nephrectomy: a report from the single port advanced research consortium (SPARC). J Endourol 36(12):1526–1531
Palacios AR, Morgantini L, Trippel R, Crivellaro S, Abern MR (2022) Comparison of perioperative outcomes between retroperitoneal single-port and multiport robot-assisted partial nephrectomies. J Endourol 36(12):1545–1550
Abaza R, Kogan P, Martinez O (2021) Impact of the COVID-19 crisis on same-day discharge after robotic urologic surgery. Urology 149:40–45
Balasubramanian S, Ronstrom C, Shiang A, Vetter JM, Sheets J, Palka J et al (2023) Feasibility and safety of same-day discharge following single-port robotic-assisted laparoscopic prostatectomy. World J Urol 41(1):35–41
Mittakanti HR, Heulitt G, Li HF, Porter JR (2020) Transperitoneal vs. retroperitoneal robotic partial nephrectomy: a matched-paired analysis. World J Urol. 38(5):1093–9
Sharma G, Shah M, Ahluwalia P, Dasgupta P, Challacombe BJ, Bhandari M et al (2022) Comparison of perioperative outcomes following transperitoneal versus retroperitoneal robot-assisted partial nephrectomy: a propensity-matched analysis of VCQI database. World J Urol 40(9):2283–2291
Xia L, Wang X, Xu T, Guzzo TJ (2017) Systematic review and meta-analysis of comparative studies reporting perioperative outcomes of robot-assisted partial nephrectomy versus open partial nephrectomy. J Endourol 31(9):893–909
Bertolo R, Garisto J, Gettman M, Kaouk J (2018) Novel system for robotic single-port surgery: feasibility and state of the art in urology. Eur Urol Focus 4(5):669–673
Fang AM, Saidian A, Magi-Galluzzi C, Nix JW, Rais-Bahrami S (2020) Single-port robotic partial and radical nephrectomies for renal cortical tumors: initial clinical experience. J Robot Surg 14(5):773–780
Kaouk J, Aminsharifi A, Sawczyn G, Kim S, Wilson CA, Garisto J et al (2020) Single-port robotic urological surgery using purpose-built single-port surgical system: single-institutional experience with the first 100 cases. Urology 140:77–84
Na JC, Lee HH, Yoon YE, Jang WS, Choi YD, Rha KH et al (2020) True single-site partial nephrectomy using the sp surgical system: feasibility, comparison with the Xi single-site platform, and step-by-step procedure guide. J Endourol 34(2):169–174
Acknowledgements
Preliminary findings of this study were presented as an abstract at the 2022 AUA Annual Meeting and are published in the Scientific Program of the 2022 AUA Annual Meeting in the Journal of Urology.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
JMB: conceptualization; methodology; data curation; visualization; writing—original draft; writing—review and editing. HH: conceptualization; investigation; data curation; writing—review and editing; supervision. JMV: methodology; formal analysis; data curation; writing—review and editing; resources. SBB: conceptualization; methodology; writing—review and editing; supervision. GMH: conceptualization; methodology; investigation; writing—original draft; writing—review and editing. NAP: conceptualization; methodology; investigation; data curation; writing—review and editing. AS: conceptualization; investigation; supervision; writing—review and editing. RSF: conceptualization; investigation; supervision; writing—review and editing. EHK: conceptualization; methodology; investigation; writing—original draft; writing—review and editing; supervision; project administration.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Berry, J.M., Hill, H., Vetter, J.M. et al. Single-port vs multi-port robot-assisted renal surgery: analysis of perioperative outcomes for excision of high and low complexity renal masses. J Robotic Surg 17, 2149–2155 (2023). https://doi.org/10.1007/s11701-023-01637-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01637-4