Abstract
Robot-assisted radical prostatectomy (RARP) is the most adopted treatment for localized prostate cancer. The aim of this study was to explore the learning curves (LC) for overall and site-specific positive surgical margins (PSM) occurrence after RARP of multiple surgeons within a step-structured mentor-initiated training program. The study included consecutive patients undergoing RARP between January 2013 and March 2020, by three surgeons: a mentor and his two trainees. Prospectively collected patients’ data were retrospectively analyzed. The cumulative summation (CUSUM) method was used to generate the LCs, with turning points indicating the number of cases to reach proficiency levels. Furthermore, the association between PSM and surgical experience was evaluated, adjusting for case mix. A total of 761 consecutive patients were included, 370 treated by the Mentor surgeon, 247 and 144 treated, respectively, by the two Trainees. Mentor and Trainees had similar PSM rates (31.6% vs 28.0% vs 31.3%, p = 0.6). CUSUM charts showed different LC shapes for different PSM locations (postero-lateral, bladder neck, apex, and multifocal/> 3 mm). Surgical experience was significantly associated with overall, postero-lateral, and multifocal/> 3 mm PSMs, in the Mentor series only. Trainees reached their turning points after far fewer cases then the Mentor, both for overall (12 and 31 vs 153), postero-lateral (24 and 30 vs 120), and multifocal/> 3 mm PSMs (9 and 31 vs 153). The achievement of stable SM proficiency takes involved different LCs depending on the prostatic location being considered. Monitoring site-specific LC can indicate the surgical steps for which there may be still room for further technical refinements, even when an apparent proficiency status seems achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robot-assisted radical prostatectomy (RARP) is the most adopted treatment of localized prostate cancer [1, 2]. The main goal of oncological surgery is cancer control, which, during radical prostatectomy (RP) for prostate cancer, means the control of surgical margins (SM). Positive SM (PSM) after RP are associated with a greater risk of biochemical recurrence (BCR) and patient anxiety [3, 4]. Furthermore, there are increasing evidences on the impact of location, number, and length of PSM after RP in predicting BCR [5, 6]. As a result, the achievement of proficiency in SM control should be the most important goal in RARP training. A thorough knowledge of surgeons’ learning curve (LC) may be useful for the development of effective and standardized training programs that guarantee the achievement of a baseline expertise, without jeopardizing the patient's safety during the learning phase [7]. Several LC studies have shown the impact of surgical experience on the outcomes of RARP, focusing more often on functional outcomes, operative time, and estimated blood loss [8,9,10]. Few studies have shown the existence of an LC for PSM occurrence after RARP [11,12,13,14], and no studies have shown the existence of different LC for different locations, number, and length of PSM.
The aim of this study was to explore, using the cumulative summation (CUSUM) method, the learning curves for overall and site-specific PSM occurrence after RARP of three surgeons within a step-structured mentor-initiated training program with a dual console system, in a second-generation robotic tertiary referral center.
Materials and methods
Patient population, study design, and data assessment
All consecutive patients undergoing RARP, between January 2013 and March 2020, at our institution were included in this IRB-approved study after signing an informed consent. Prospectively collected patients’ data were retrospectively analyzed. PSM locations have been classified into apex, right (RPL), and left (LPL) postero-lateral, bladder neck (BN), according to a multi-institutional study by Patel et al. [15]. Multifocal PSM or PSM longer than 3 mm (MF/> 3 mm) were also recorded [16]. The surgeon performing each surgical step was recorded in the operation report. Overall 42 (5.5%) procedures involved two surgeons (the Mentor and one of the Trainees). Recorded PSMs were attributed to the surgeon responsible for the surgical step that was crucial for the specific PSM location.
Surgical technique and training program
All procedures were performed following a standardized four-arms RARP procedure (Montsouris technique [17], using a transperitoneal six-port approach, 0° lens, da Vinci SI® (from 2013 to December 2015) or da Vinci XI® (from January 2016) robotic surgical system (Intuitive Surgical Inc.). Briefly, an initial posterior approach to the seminal vesicles from Douglas’ pouch was used; BN preservation was attained whenever technically possible; planned, intrafascial, or interfascial nerve-sparing technique (NS) was performed selectively based on side-specific risk assessment, including multiparametric MRI findings available for most patients in our series; apical dissection was carried out using an anterior approach, after controlling with resorbable stiches and cutting the dorsal venous complex (DVC), and circularly freeing and cutting the urethra a few millimeters away from the apex. Vesico-urethral anastomosis was performed using the Van Velthoven technique.
Surgical procedures have been performed by three right-handed surgeons. The Mentor had a large previous open RP experience and started performing RARP after a 6-month training period, including simulation and observership in qualified robotic surgery centers. Trainee 1 and Trainee 2 had no previous RP experience before starting to perform RARP at our institution through a step-structured mentor-initiated training program.
The training program included a period of didactic sessions regarding robotic mechanics and instrumentations, dry and wet lab. The next step of the program consisted in becoming proficient as bedside assistant of the Mentor, thus learning the steps of the RARP procedure. The program culminated in the trainees performing specific parts of the procedure under supervision of the Mentor, ready to take over thanks to a dual console system. Console training was divided into five steps: (1) dissection of seminal vesicles and posterior prostate, bladder detachment, incision of endopelvic fascia, and dorsal venous complex (DVC) ligation; (2) BN incision, control of prostatic pedicles and NS; (3) DVC transection, apex dissection and transection of the urethra; (4) suturing the vesicourethral anastomosis; (5) pelvic lymphadenectomy. A trainee could move on to the next step when judged proficient by the Mentor.
Pathological evaluation
RARP specimens were evaluated by two academic uro-pathologists (PF and MM). Each radical prostatectomy specimen was totally embedded and processed with the whole-mount method. Each specimen was weighed, measured, inked, and fixed in 10% neutral formalin. After fixation, the apex and base were amputated and serially sectioned at 4 mm intervals in the vertical para-sagittal plane. The seminal vesicles were sectioned parallel to their junction with the prostate and entirely submitted for evaluation. The remaining specimen was serially sectioned perpendicular to the long axis of the gland from the apex to the base. Whole-mount sections were prepared at 5 mm sections and stained with hematoxylin and eosin for histological evaluation. When immunohistochemical studies were necessary, the paraffin block with the whole-mount section was divided in four microblocks (anterior-lateral left and right quadrants, posterior-lateral left and right quadrants). A PSM was defined as cancer cells seen at the inked margin [18, 19].
Cumulative sum (CUSUM) method
The CUSUM method was used to generate retrospectively the learning curves for overall and site-specific PSM occurrence. Overall PSM learning curve was also stratified by pathological stage. We chose the most intuitive CUSUM technique, that is the cumulative “observed minus expected failure” method which plots the procedures chronological sequence number on the horizontal axis against the cumulative sum of observed minus expected failure rate on the vertical axis [20, 21].
While there is a plenty of literature regarding the acceptable range of overall PSM rate after RARP [22], there are no such consistent reporting for different PSM locations, number, and length. Because of this gap in the literature, as expected minimum proficiency levels (expected failure rate) for overall and site-specific PSM rate, we chose the PSM rates reached by the Mentor in the last part of his case series, when his PSM rates stabilized at a plateau level, according to the methodology described by Rogers et al. [23]. For each CUSUM curve, we defined a turning point as a peak point after which the PSM rate begins to decrease and then reaches the proficiency level without increasing significantly again.
Statistical analysis
Mean and standard deviation or median and 95% confidence interval (CI) were used to report continuous variables, as appropriate. Chi-squared test was used to compare categorical variables and ANOVA to compare continuous variables. Univariate and multivariate logistic regression analyses were used to evaluate the association between PSMs and potential predictors for the whole patient population. To evaluate the association between PSM and surgical experience, adjusting for case mix, we built, for each surgeon, a multivariate model regressing the overall and site-specific SM status on surgical experience and the independent predictors of PSM in our series. Surgical experience was defined splitting equally each surgeon’s case series into three groups of consecutive patients according to the chronological order based on procedure date [11].
A two-sided p < 0.05 was deemed to indicate statistical significance. Statistical analyses were performed using MedCalc software for Windows v.12.3.0 (MedCalc Software, Mariakerke, Belgium).
Results
Patients and PSM characteristics
Table 1 displays peri-operative, intra-operative, and post-operative characteristics of the 761 consecutive included patients. Overall PSM rate was 30.3% (231/761). No significant differences in patient characteristics emerged between the surgeons.
Table 2 shows SM status by location/extension and surgeon. The apex was the most common site of PSM (108/761, 14.3%), followed by the postero-lateral location (82/761, 10.8%) and the bladder neck (69/761, 9.1%). Within the postero-lateral location, a significantly higher PSM rate was observed for the left side (RPL/LPL: 4.5%/7.0%, p = 0.04).
The PSM rate for pT2 and pT3 cases was 23.3% (133/570) and 50.8% (97/191), respectively (p < 0.0001). The pT3 PSM rate was significantly higher than pT2 PSM rate even for each specific PSM location (see the table in Online Resource 1). No statistically significant differences were found between the surgeons for the incidence of PSM stratified by location/extension.
CUSUM analysis
Figure 1 shows CUSUM charts with learning curves for PSM occurrence in the whole population (Fig. 1A) and in the pT2 population (Fig. 1B) of each surgeon. A prominent reduction in the PSM rate, indicating improving performance, was evident for all surgeons and in both patient populations. For each surgeon, it was possible to identify a three-phase learning curve: an initial upward trend (phase 1), a phase of decline culminating with a turning point (phase 2) after which the PSM rate decreases to or below the proficiency level, reaching the plateau (phase 3) in the overall population. Mentor's turning point (case 153) was set much further in his overall case series than that of Trainee 1 (case 12) and Trainee 2 (case 31). The same trend, for each surgeon, was noted in the pT2 population chart (Mentor’s turning point at 118 cases; Trainee 1 at 14 cases; Trainee 2 at 21 cases).
Figure 2 shows CUSUM charts of the three surgeons for the different PSM locations and for multifocal or > 3 mm PSM in the whole patient population.
The CUSUMPOSTEROLATERAL chart (Fig. 2A) showed a clear learning curve effect for all the three surgeons, with the recognizable three phases: again, the decline phase was longer and more gradual for the Mentor (turning point at case 120), shorter for Trainee 1 and Trainee 2 (turning points at case 24 and case 30, respectively); the final plateau phase set around a common 10% rate.
The CUSUMBLADDER-NECK curves (Fig. 2B) identified, for all three surgeons, the achievement of a plateau at a 10% rate after about 100 cases. The very early phase of the curve was characterized by inhomogeneous trends: while for Trainee 1, there was a learning curve effect characterized by a progressive reduction in the PSM rate as the surgeon’s experience increased, for Mentor and Trainee 2, we registered a progressive stabilization after a fluctuating trend in a narrow range (5–15%).
Looking at the CUSUMAPEX chart (Fig. 2C), a learning curve effect cannot be identified for any of the surgeons, with the PSM rate fluctuating in a wide range around 15%, without an identifiable trend toward a plateau.
The three-phase learning curve can also be identified in the CUSUMMF or >3 mm chart (Fig. 2D), with a trend that imitates, for each surgeon, that of the general PSM learning curve: even in this case, the turning points of Trainee 1 (case 9) and Trainee 2 (case 31) occurred earlier than that of the Mentor (case 153).
Multivariate analysis
Univariate and multivariate logistic regressions for PSM predictors performed for the whole patient population are displayed in Table 3. Prostate volume, preoperative PSA, nerve-sparing technique, pathological stage, perineural invasion, and percentage of cancer in the surgical specimen were statistically significant independent predictors for PSM occurrence.
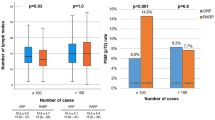
Table 4 shows the multivariate models assessing the association between surgical experience and overall and site-specific PSM occurrences adjusted for statistically significant independent predictors of PSM, for each of the surgeons. The Mentor’s model revealed a significant association between surgical experience and overall, PL and MF or > 3 mm PSM, while Trainees’ models revealed not such associations.
Discussion
As far as we know, this is the first study to show the existence of different learning curves for different PSM locations in RARP. Two previous studies have shown that the CUSUM method is a useful tool for evaluating PSM learning curve of RARP, but they did not evaluate the site-specific PSM occurrence [12, 13]. Williams et al. monitored PSM rate during a single surgeon transition from open to robotic RP in a series of 158 patients with pT2 disease: using CUSUM method, they found a turning point at procedure 50 (PSM rate 22%) with a subsequent flattening trend (PSM rate 13%) after 110 procedures [12]. Sivaraman et al. used CUSUM method to analyze their institutional RARP series (initiated after 250 laparoscopic RP) as a whole (9 surgeons), finding a turning point after 100 procedures (PSM rate 20%) [13].
Within our multi-surgeon learning curve analysis, we documented a statistically significant association between surgical experience and overall, PL and MF/> 3 mm PSM occurrences, but only for the Mentor surgeon and not for the Trainees. We interpreted these results based on the analysis of the CUSUM charts, which showed Trainees reaching proficiency in SM control much earlier than their Mentor. Reaching their turning points after far fewer cases than their Mentor, Trainees proved to benefit significantly from institutional experience built by the Mentor who imported the surgical technique and standardized it within the hospital. In line with our results, Schroeck et al. (2008) showed how the trainees of an experienced mentor had, in the early phase of a mentor-initiated RARP training program, lower PSM rates than their mentor in the same phase [24], although site-specific PSM rates were not assessed.
In our study, we identified different CUSUM curve shapes for different PSM locations, with implications for the different steps of RARP training.
The CUSUMPOSTEROLATERAL curves showed a clear learning curve effect, shaping predominantly the early phase of the overall PSM learning curve, with Trainees reaching their turning points earlier than their Mentor. In our series, NS technique proved to be an independent risk factor for PSM; therefore, a faster mastery of NS technique by the Trainees may be an explanation for the anticipation of their turning points. Other authors reported an association between NS and increased risk of PSMs [25,26,27], even though the issue remains controversial [28].
For the postero-lateral location, we also documented a statistically significant difference in the PSM rate between the right and left side, with the left postero-lateral being associated with a higher risk of PSMs. The left-sided dominance of PSM has been previously described by other authors, both in robotic [29] and laparoscopic RP [30]. An explanation may be the asymmetry in the mutual position of robotic instruments (scissors and forceps) and the different prostatic side, introducing inherent technical limits during the left postero-lateral dissection for right-handed surgeons. More conflicts between bipolar and Prograsp forceps, limitations in the range of motion of the fourth arm, and right robotic instruments reaching the left postero-lateral aspect of the gland in a somewhat uncomfortable way, make more technically challenging the left postero-lateral dissection. In terms of training, we believe that PL dissection, even with NS intent, can be safely introduced in the early steps of learning if under the supervision of a skilled mentor, paying greater attention to the dissection of the side opposite the surgeon's dominant hand.
The CUSUMBLADDER-NECK chart showed inhomogeneous trends between the three surgeons in the very early phase of the experience (first 20 cases), and then a phase of transition with fluctuating PSM rates in a narrow range (5–15%) before reaching a common plateau phase at 10% rate (after about 100 cases, for all the surgeon). A possible interpretation for the fluctuation phase may be the progressive acquisition of mastery of the bladder neck sparing technique (BNS), but we had not enough data on the BN dissection technique applied for all the patients, to test this hypothesis. BNS can be problematic due to the junction’s anatomical variability and lack of natural visual land-marks [31]. However, there is no consensus in the literature on BNS as a risk factor for PSM, as highlighted in a recent review on the topic by Bellangino et al. [32]. The same lack of consensus concerns the association between BNS and BCR: in a large RARP series of > 1000 patients, Friedlander et al. reported no difference in BCR-free survival for BNS and non-sparing groups [33]. According to our experience BNS can be safely introduced in the early phases of a mentor-initiated training, avoiding, at the beginning, cases with large prostate, prominent median lobes and known disease at the base of the gland.
The apex was the most common PSM location in agreement with several robotic [15, 29, 34], laparoscopic [29, 35], and open [29, 34] radical prostatectomy series. CUSUMAPEX chart did not show a peculiar curve for this site, nor a significant reduction in the PSM rate associated with improving surgical experience, not even for the Mentor with the most extensive series. This reflects the challenging nature of apex dissection, where maximizing urethral length and sparing neurovascular bundles can jeopardize complete tumor resection balancing [36]. Other reasons for the high apex PSM rate are its variable configuration and the poor representation of capsule and peri-prostatic tissues in this location, which determine more frequent iatrogenic intra-prostatic incisions and a more difficult distinction between intra-prostatic and extra-prostatic tissue for the pathologist, all leading to artifacts or "false" PSMs [3, 37]. A study by Marcq et al. found that only extensive apical PSMs, but not focal apical PSMs, were independently associated with biochemical recurrence (BCR) in their series; as an explanation of their results, they cited the greater presence of artifacts among the focal PSMs [38]. For all these reasons, we think that apex dissection, for its demand of precision, still must be part of the advanced steps of training programs, but always keeping in mind that surgeon experience is only one of the many variables determining apex PSMs.
Avoiding multifocal PSM and PSM length > 3 mm is an outcome to be achieved as important as avoiding the presence of PSM itself, for its recognized impact on the risk of BCR [4, 5, 15]. In our study, the learning curves identified in the CUSUMMF or >3 mm chart showed trends imitating, for each surgeon, that of the general PSM learning curve, confirming the great advantage of the trainees who reached the institutional plateau threshold after much less cases of the Mentor who set that threshold.
This study has its strength in the large contemporary series of consecutive patients in a high-volume center, in the multiple surgeons evaluation based on two effective tools for learning curve assessment (CUSUM analysis and multivariate logistic regression to adjust for case mix) [20] and in the standardized protocol for assessing the prostatectomy specimens by two experienced uro-pathologists. However, we acknowledge several limitations, including the retrospective nature, the lack of data on BCR to evaluate its association with PSMs, and the lack of enough data on BNS technique to test it as a PSM predictor. Another limitation could be the single-center design, though it is difficult and unreliable to compare different surgeons from different institutions in terms of PSM rate, considering that institutions differ, from each other, in many aspects such as patient characteristics, surgical technique, and post-operative pathological evaluation. Moreover, even though CUSUM curves are recognized effective tools for the continuous assessment of surgeons’ progress, it is difficult to compare curves of different surgeons, because LC must be appraised as an individual entity, depending on several factors that may influence the characteristics of an individual learning curve, such as surgeon experience, skills, and innate characteristics, and continuous refinements in personal surgical technique. We also acknowledge that our overall and pT2 PSM rates fell close to the upper limit of the range in the literature (6.5–32% and 4–23% [38]), although several factors may explain differences in PSM occurrence between different institutions.
Conclusions
The achievement of stable SM proficiency takes different caseloads with distinct learning curves depending not only on cancer features but also on the institutional experience and the prostatic location being considered. A step-structured mentor-initiated RARP training program can reduce trainees’ PSM rate and extension within acceptable limits in the early phase of training, thus without jeopardizing patient's oncological safety. This study supports the CUSUM method as an effective tool for surgeon self-appraisal to prompt continuous quality improvement. Monitoring site-specific learning curves can indicate the surgical steps for which there may be still room for further technical refinements, even when an apparent proficiency status seems to have been achieved.
Availability of data and materials
Data related to patients and surgical procedures can be found at the Department of Urology, Fondazione Policlinico Universitario A. Gemelli IRCCS-Università Cattolica del Sacro Cuore, Largo Agostino Gemelli 8, 00168 Rome, Italy. The results of histopathologic exams are available at the Department of Anatomic Pathology and Histology, Fondazione Policlinico Universitario A. Gemelli IRCCS-Università Cattolica del Sacro Cuore, Largo Agostino Gemelli 8, 00168 Rome, Italy.
References
Trinh QD, Sammon J, Sun M (2012) Perioperative outcomes of robot-assisted radical prostatectomy compared with open radical prostatectomy: results from the nationwide in patient sample. Eur Urol 61(4):679–685. https://doi.org/10.1016/j.eururo.2011.12.027
Sacco E, Bientinesi R, Bassi PF (2015) Current status of robotic urologic surgery in Italy. Urologia 82(Suppl 1):S8-10
Sooriakumaran P, Dev HS, Skarecky D (2016) The importance of surgical margins in prostate cancer. J Surg Oncol 113(3):310–315. https://doi.org/10.1002/jso.24109
Pinto F, Prayer-Galetti T, Gardiman M (2006) Clinical and pathological characteristics of patients presenting with biochemical progression after radical retropubic prostatectomy for pathologically organ-confined prostate cancer. Urol Int 76(3):202–208. https://doi.org/10.1159/000091619
Dev HS, Wiklund P, Patel V (2015) Surgical margin length and location affect recurrence rates after robotic prostatectomy. Urol Oncol 33(3):109.e7–13. https://doi.org/10.1016/j.urolonc.2014.11.005
Rajan P, Hagman A, Sooriakumaran P (2018) Oncologic outcomes after robot-assisted radical prostatectomy: a large european single-centre cohort with median 10-year follow-up. Eur Urol Focus 4(3):351–359. https://doi.org/10.1016/j.euf.2016.10.07
Ahmed K, Khan R, Mottrie A (2015) Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int 116(1):93–101. https://doi.org/10.1111/bju.12974
Sharma NL, Papadopoulos A, Lee D (2011) First 500 cases of robotic-assisted laparoscopic radical prostatectomy from a single UK centre: learning curves of two surgeons. BJU Int 108(5):739–747. https://doi.org/10.1111/j.1464-410X.2010.09941.x
Jaffe J, Castellucci S, Cathelineau X (2009) Robot-assisted laparoscopic prostatectomy: a single-institutions learning curve. Urology 73(1):127–133. https://doi.org/10.1016/j.urology.2008.08.482
Sacco E, Prayer-Galetti T, Pinto F (2006) Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int 97(6):1234–1241. https://doi.org/10.1111/j.1464-410X.2006.06185.x
Atug F, Castle EP, Srivastav SK (2006) Positive surgical margins in robotic-assisted radical prostatectomy: impact of learning curve on oncological outcomes. Eur Urol 49(5):866–871. https://doi.org/10.1016/j.eururo.2006.02.054
Williams AK, Chalasani V, Martínez CH (2011) Cumulative summation graphs are a useful tool for monitoring positive surgical margin rates in robot-assisted radical prostatectomy. BJU Int 107(10):1648–1652. https://doi.org/10.1111/j.1464-410X.2010.09634.x
Sivaraman A, Sanchez-Salas R, Prapotnich D (2017) Learning curve of minimally invasive radical prostatectomy: comprehensive evaluation and cumulative summation analysis of oncological outcomes. Urol Oncol 35(4):149.e1-149.e6. https://doi.org/10.1016/j.urolonc.2016.10.015
Bravi CA, Tin A, Vertosick E (2019) The impact of experience on the risk of surgical margins and biochemical recurrence after robot-assisted radical prostatectomy: a learning curve study. J Urol 202(1):108–113. https://doi.org/10.1097/JU.0000000000000147
Patel VR, Coelho RF, Rocco B (2011) Positive surgical margins after robotic assisted radical prostatectomy: a multi-institutional study. J Urol 186(2):511–516. https://doi.org/10.1016/j.juro.2011.03.112
Sooriakumaran P, Ploumidis A, Nyberg T (2015) The impact of length and location of positive margins in predicting biochemical recurrence after robot-assisted radical prostatectomy with a minimum follow-up of 5 years. BJU Int 115(1):106–113. https://doi.org/10.1111/bju.12483
Guillonneau B, Vallancien G (2000) Laparoscopic radical prostatectomy: the Montsouris technique. J Urol 163(6):1643–1649. https://doi.org/10.1016/s0022-5347(05)67512-x
Tan PH, Cheng L, Srigley JR (2011) International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. working group 5: surgical margins. Mod Pathol 24(1):48–57. https://doi.org/10.1038/modpathol.2010.155
Pierconti F, Rossi ED, Martini M (2019) 34BetaE12 and Alfa-methylacyl coenzyme A racemase (AMACR) antibodies better than p63 antibody distinguish normal and neoplastic glands in prostatic tissue with thermal artifacts. Appl Immunohistochem Mol Morphol 27(4):306–310. https://doi.org/10.1097/PAI.0000000000000599
Maguire T, Mayne CJ, Terry T (2013) Analysis of the surgical learning curve using the cumulative sum (CUSUM) method. Neurourol Urodyn 32(7):964–967. https://doi.org/10.1002/nau.22375
Ramsay CR, Grant AM, Wallace SA (2001) Statistical assessment of the learning curves of health technologies. Health Technol Assess 5(12):1–79. https://doi.org/10.3310/hta5120
Novara G, Ficarra V, Mocellin S et al (2012) Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur Urol 62(3):382–404. https://doi.org/10.1016/j.eururo.2012.05.047
Rogers CA, Reeves BC, Caputo M (2004) Control chart methods for monitoring cardiac surgical performance and their interpretation. J Thorac Cardiovasc Surg 128(6):811–819. https://doi.org/10.1016/j.jtcvs.2004.03.011
Schroeck FR, de Sousa CAP, Kalman RA (2008) Trainees do not negatively impact the institutional learning curve for robotic prostatectomy as characterized by operative time, estimated blood loss, and positive surgical margin rate. Urology 71(4):597–601. https://doi.org/10.1016/j.urology.2007.12.023
Preston MA, Breau RH, Lantz AG (2015) The association between nerve sparing and a positive surgical margin during radical prostatectomy. Urol Oncol 33(1):18.e1-18.e6. https://doi.org/10.1016/j.urolonc.2014.09.006
Mortezavi A, Hermanns T, Seifert HH (2012) Intrafascial dissection significantly increases positive surgical margin and biochemical recurrence rates after robotic-assisted radical prostatectomy. Urol Int 89(1):17–24. https://doi.org/10.1159/000339254
Liss M, Osann K, Ornstein D (2008) Positive surgical margins during robotic radical prostatectomy: a contemporary analysis of risk factors. BJU Int 102(5):603–608. https://doi.org/10.1111/j.1464-410X.2008.07672.x
Nguyen LN, Head L, Witiuk K (2017) The risks and benefits of cavernous neurovascular bundle sparing during radical prostatectomy: a systematic review and meta-analysis. J Urol 198(4):760–769. https://doi.org/10.1016/j.juro.2017.02.3344
Albadine R, Hyndman ME, Chaux A (2012) Characteristics of positive surgical margins in robotic-assisted radical prostatectomy, open retropubic radical prostatectomy, and laparoscopic radical prostatectomy: a comparative histopathologic study from a single academic center. Hum Pathol 43(2):254–260. https://doi.org/10.1016/j.humpath.2011.04.029
Secin FP, Serio A, Bianco FJ (2007) Preoperative and intraoperative risk factors for side-specific positive surgical margins in laparoscopic radical prostatectomy for prostate cancer. Eur Urol 51(3):764–771. https://doi.org/10.1016/j.eururo.2006.10.058
Skarecky DW (2013) Robotic-assisted radical prostatectomy after the first decade: surgical evolution or new paradigm. ISRN Urol. https://doi.org/10.1155/2013/157379
Bellangino M, Verrill C, Leslie T (2017) Systematic review of studies reporting positive surgical margins after bladder neck sparing radical prostatectomy. Curr Urol Rep 18(12):99. https://doi.org/10.1007/s11934-017-0745-0
Friedlander DF, Alemozaffar M, Hevelone ND (2012) Stepwise description and outcomes of bladder neck sparing during robot-assisted laparoscopic radical prostatectomy. J Urol 188(5):1754–1760. https://doi.org/10.1016/j.juro.2012.07.045
Ahlering TE, Woo D, Eichel L (2004) Robot-assisted versus open radical prostatectomy: a comparison of one surgeon’s outcomes. Urology 63(5):819–822. https://doi.org/10.1016/j-.urology.2005.01.038
Guillonneau B, El-Fettouh H, Baumert H (2003) Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases at Montsouris Institute. J Urol 169(4):1261–1266. https://doi.org/10.1097/01.hu.0000055141.36916.be
Touijer K, Kuroiwa K, Saranchuk JW (2005) Quality improvement in laparoscopic radical prostatectomy for pT2 prostate cancer: impact of video documentation review on positive surgical margin. J Urol 173(3):765–768. https://doi.org/10.1097/01.ju.0000146574.52402.d5
Walz J, Burnett AL, Costello AJ (2010) A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol 57(2):179–192. https://doi.org/10.1016/j.eururo.2009.11.009
Marcq G, Michelet A, Hannink G (2019) Correction to: Risk of biochemical recurrence based on extent and location of positive surgical margins after robot-assisted laparoscopic radical prostatectomy. BMC Cancer 19(1):124
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Fondazione Policlinico A. Gemelli IRCCS, Rome, Italy (protocol code 0001853/21 and January 20, 2021).
Consent to participate
Informed consent was obtained from all subjects involved in the study that we were able to contact.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gandi, C., Totaro, A., Bientinesi, R. et al. A multi-surgeon learning curve analysis of overall and site-specific positive surgical margins after RARP and implications for training. J Robotic Surg 16, 1451–1461 (2022). https://doi.org/10.1007/s11701-022-01378-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01378-w