Abstract
Introduction
dHACM is a source of factors including cytokines that allow anti-inflammatory and proliferative elements to be utilized for wound and ulcer management. We present our experience of using dHACM in a cohort of patients undergoing nerve-sparing (NS) robot-assisted laparoscopic prostatectomy (RALP). Our objective is to investigate the functional and oncological outcomes of NS after placing amniotic or dehydrated human amnion/chorion membrane (dHACM) on preserved neurovascular bundles (NVBs). From 2013 to 2019, our institution performed transperitoneal multi-port da Vinci robotic prostatectomy. The NVBs are spared by releasing their fascial planes posteriorly, followed by an anterior release of the plane at a similar level. Once the retrograde release of the NVB is performed then 599 patients underwent placement of dHACM graft (AmnioFix by MiMedx, Marietta, GA, USA). The graft was cut into two 4 × 1 cm pieces and laid over the NVB as a wrap. In order to inform the urological community of oncological and functional outcomes, we excluded patients with less than 12 months follow up (n = 64), benign prostatic hyperplasia (n = 5), and unilateral NS (n = 1). 529 (88%) patients were included in this study who underwent a partial or full bilateral NS with dHACM. 529 patients were followed-up for a median (IQR) of 42 months (25–89). Demographics include median (IQR) age 57 years (52–62), median preoperative SHIM score of 24 (21–15), and AUASS of 5 (2–11). Full NS was performed in 74% (391/529). Pathological staging was pT2 = 399 (75%), pT3a = 107 (20%), pT3b = 19 (4%) and pT4 = 4 (1%) with N1 = 3 (0.6%). The number of patients with PSM was 86 (16%), and the overall BCR in the entire cohort was 10%. Postoperatively, 434 (82%) were sexually active. Median time to potency was 119 (37–420) days and time to continence was 42 (23–91) days. Regarding full vs partial NS: median post op SHIM score 18 (13–20) vs 15 (6–20), median time to potency 92 (35–365) days vs 184 (42–560) days, and median time to continence 42 (23–91) days vs 44 (30–92) days. Age > 55 vs ≤ 55 years: median post op SHIM score 18 (12–20) vs 15 (10–20), median time to potency 167 days (42–549) vs 80 (35–288) days, and median time to continence 42 (25–116) days vs 42 (29–76) days. In our series the application of amniotic membrane/dHACM has led to acceptable post RALP outcomes. The BCR rate of 10% in addition to the recovery of potency at a median time of 3 months and continence at 6 weeks is an encouraging result of dHACM. Our findings indicate that dHACM allowed for an even faster period for continence recovery which was independent of grade of NS. Future comparative studies may further assess the impact of new amniotic membrane types on the functional and oncological outcomes after RALP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the second most commonly diagnosed tumor among men in the United States, with 250,000 new cases estimated for 2021 according to the American Cancer Society. Environmental factors along with genetics can predispose patients to prostate cancer, and those undergoing definitive surgical management of prostatectomy may have potency and urinary continence impacted [1]. To mitigate this, meticulous surgical technique along with adjuncts should be investigated and employed.
For more than 50 years, amniotic membranes have been used in managing chronic wounds, corneal surfaces, orthopedic and neurosurgical clinical settings [2]. Challenges in storage and preservation of fresh human amnion were overcome by processing through dehydration and cleansing, to retain regulatory molecules. Therefore, dehydrated human amnion/chorion membrane (dHACM) has shown benefit in treating diabetic ulcers, burns and dermal injuries by reducing pain, inflammation and scar formation [3]. Functioning as a source of growth factors and cytokines [2], the ability of these grafts to improve post prostatectomy recovery was hypothesised. The complex role of biological activity from studies on this product in vitro and in vivo, involve angiogenesis and extracellular matrix deposition among others.
After the discovery of the neurovascular bundle (NVB) by Walsh and Donker in 1981 [4] radical prostate surgery outcomes improved. Patients undergoing degrees of nerve-sparing (NS) prostatectomy rather than wide local excision resulted in recovery of erectile function. In order to preserve the function of these nerve structures, high volume expertise in dissection with rigorous postoperative penile rehabilitation is crucial but finite [5]. Forty years after Walsh’s discovery, our Unit has utilised dHACM in a cohort of patients undergoing NS robot-assisted laparoscopic prostatectomies (RALP), in order to be a comparison with other surgical approaches [6].
The utility of dHACM was previously examined in NS RALPs as proof of concept in functional recovery, when compared to matched cohorts [7,8,9]. This study provides the descriptive analysis of our experience since we commenced using dHACM, to aid urology community when similar adjuncts are used in the future.
Methodology
Study population and technique
Institutional review board approval was granted for this study between 2013 and 2019, to perform a transperitoneal multi-port RALP utilizing a da Vinci surgical system. dHACM was guided into the operative field and implanted in 635 patients. The NS approach is performed by retrogradely releasing the NVB from their fascial plane during the posterior dissection. Following this, an athermal anterior release of the plane at a similar level connects the two dissection points, followed by a complete retrograde release of the NVB with limited traction [10]. This series is from a single surgeon (V.P.), with dHACM graft placed over each NVB after the posterior musculofascial ‘Rocco’ reconstruction and before the vesico-urethral anastomosis.
Definitions
Potency was defined as the ability to achieve and maintain erections for penetrative intercourse, with or without the use of PDE-5 inhibitors. Continence was defined as the absence of uncontrolled leakage of urine. Biochemical recurrence (BCR) is a post RALP PSA of > 0.2 ng/mL.
Adjuvant treatment refers to initiation of therapeutics before a post RALP PSA threshold of 0.2 ng/mL; salvage treatment refers to initiation of therapeutics after BCR occurs.
Inclusion/exclusion criteria
Patients who underwent surgery more than 1 year ago were included in the study. Patients aged 40–75 years who were pre-operatively potent with Sexual Health Inventory for Men (SHIM) scores of 20 or above and underwent full or partial bilateral NS RALPs were also included. Patients with preoperative erectile dysfunction (ED) or SHIM less than 20 did meet inclusion criteria to have dHACM. Patients with locally advanced disease on staging investigations (MRI or CT) and/or previous bladder outflow obstruction surgery were excluded from the study.
To inform the urological community of oncological and functional outcomes, we excluded 64 patients with less than 12 months follow-up recorded, 5 individuals who had benign prostatic hyperplasia, and 1 individual who underwent unilateral NS with accompanying allograft. Taking into account these exclusions, 529 patients (88% or 529/599) underwent a partial or full bilateral NS and were included in this study.
Statistical analysis
Continuous variables are reported as median and interquartile range (IQR), and categorical as absolute and percentage frequencies.
Patients were analysed based on full or partial degree of NS, and age > or ≤ 55. These groups were compared using Wilcoxon rank-sum test for continuous and Fisher’s exact test for categorical variables. Cumulative incidence functions (CIFs) for functional outcomes were estimated using the Kaplan–Meier method and were compared between groups using the log rank-test. Unadjusted and adjusted hazard ratios (HRs) were estimated using uni- and multi-variable Cox regression models. The hypothesis of statistically significant HRs was investigated using the Wald test. Statistical significance was set at p < 0.05 for a two-tailed test. The statistical analyses were performed using Stata version 16 (Stata Corp., College Station, TX, USA) and R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria).
Results
In this study, 529 patients were followed-up for a median period of 42 months. Table 1 shows a median PSA of 5.1 ng/mL and age of 57 years old. The median preoperative SHIM score was 24 and median American Urological Association Symptom Score (AUASS) was 5. Full NS was performed in 74% (391/529), no patient had a non NS procedure.
Histopathological & oncology outcomes
Table 2 demonstrates the most common pathological stage was pT2 in 75%. Overall, 55% (292/529) of patients underwent pelvic lymph node dissection of which the pathology revealed N0 in 289 and N1 = 3 patients. Positive surgical margins (PSM) were seen in 16%, and BCR in 10% of the entire cohort. Of the patients with PSM, 19% (16/86) had BCR; and those with adverse tumor pathological staging (> T3a) 18% (24/130) had BCR. Rates of adjuvant and salvage therapy are shown in Table 2.
Functional outcomes
Table 3 demonstrates overall functional outcomes for this cohort, with 434 (82%) patients being sexually active. Mechanical support in the form of vacuum erection device was 19% and PDE5-i use of sildenafil or tadalafil was 47%. Continence data by the number of pads used per day was 0 pad usage in 507 patients (96%), 1 pad usage for 9 patients (1.7%) and 2 pads for 5 patients (1%).
A subgroup analysis by age (below/above 55 years) and NS degree (full vs partial). Statistically significant differences between groups were noted in SHIM score, erection score and sexually activity or not.
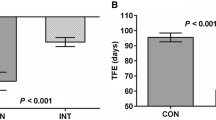
Table 4 is the result of median time to regain continence and potency for the total cohort, by age and by NS degree with adjusted HR. The comparison was also performed by estimating cumulative incidence functions for age group, seen in Figs. 1 and 2.
Discussion
This study updates the urological community on the functional and oncological outcomes of a large series of patients undergoing placement of amniotic membrane/dHACM at the time of RALP. The use of this adjunct was previously investigated by the senior author and other Institutions with regard to its early outcomes in prostate cancer surgery [9]. Studies of lower limb wound care and the role of amniotic membranes have concluded that it accelerates healing; a process of regulated haemostasis, inflammation, remodelling and recruitment of leukocytes, platelets, fibroblasts, vascular smooth muscle cells among others. dHACM is made up of preserved human placenta with an extracellular matrix protein that provides growth factors, cytokines and chemokines [11]. dHACM is also being investigated in renal cancer surgery, with current trials assessing its impact post partial nephrectomy (ClinicalTrials.gov Identifier: NCT03323021). In vitro biocompatibility with endothelial, cardiac myocytes and cord blood mesenchymal cells showed in vivo application when neovascularization in a porcine model was feasible, after a multi-layered sheet of amniotic membrane was applied [12]. Surgical scientists are challenged to investigate how these molecular frameworks impact the recovery from oncologic surgery and tumor biology.
Historical concerns of amniotic allografts’ retrieval, preparation, and storage before surgery, with tissue-borne disease transmission is addressed by sterile preparation and dehydration. The product storage and transportability means that amniotic membranes has received renewed interest in its effectiveness in a range of clinical practises [13]. In regards to RALP, the dissection of NVBs off of the prostate requires precision and correlation of biopsy histopathology to gross anatomy for optimising degrees of NS [14]. Traction and diathermy of the NVB can delay recovery of potency, where optimised techniques can be beneficial [15]. To enhance recovery further, adjuncts such as human amniotic membrane have reduced recurrence of perineural tissue adhesions and associated fibrosis in previous trials. This accelerates nerve function post trauma or surgery and could likely prevent neuroma formation, in respect to peripheral nerve injuries [16]. Furthermore, when the NVB is laid open on the prostate bed, the dHACM sheet can be applied as a wrap directly so that it is secured in place by the small volume of residual blood.
In regards to our patient demographics in Table 1, the majority of dHACM products were utilised in those that met criteria from our previous study such as SHIM > 20, bilateral NS and age 40–75 [7]. Our median BMI of the cohort, did challenge obesity being an independent factor in prolonging the healing period with dHACM in wounds [17].
The overall PSM rate of 16% (for a 95% cohort with ≤ pT3a), is in keeping with a study[18] correlating PSM rates to pT2 and pT3a, of 8.6% and 26.6% rate, respectively. Patients with pathological staging of > T3a had BCR in 18%; while studies on extracapsular extension (ECE) and seminal vesicle invasion (SVI) predict BCR [19], this requires further investigation with dHACM. Alvim et al. [20] investigated immunodeficient mice injected with human cell lines for prostate (LNCaP) and bladder cancer (UM-UC-3) concluding that utilization of dHACM in incomplete excision of tumors resulted in comparatively faster relapse and regrowth. The undefined heterogeneity of interaction with a human amniotic derived product in mice, have unmeasured variables and may not substantiate a contra-indication of dHACM in human clinical practise. Nonetheless, a long-term cancer investigation of post RALP and amniotic membrane patients is warranted due to absence of published literature in this arena.
In regards to functional outcomes, days to return of potency was higher in the full NS group (p = 0.003). However, return to continence or AUA scores was independent of NS degree with dHACM, and reflects our technique of preserving apical structures and the endopelvic fascia [21]. Our unit routinely performs a modified posterior ‘Rocco’ reconstruction of the rhabdosphincter which has impacts the return of continence [22] with or without NS. We started modified posterior ‘rocco’’ reconstruction before dHACM was used in urologic oncology, and it is consistently used since 2011.
Data with and without dHACM for functional outcomes are not available, and so the next comparative step was in patients who were younger or older than 55 years. Younger patients had faster continence and potency recovery as represented by Figs. 1 and 2. This is substantiated by a statistically significant difference in parameters that represented sexual function in Table 3 (SHIM, PDE5i, erection score, mechanical support). However, AUASS showed no difference between age groups. AUSSS is considered an objective assessment of treatment outcomes of prostate cancer in the literature [23].
Instances of slow recruitment and COVID-19’s impact on additional centres having the opportunity to study this product on a single or multi-institutional level is noted. This study has several limitations, specifically pertaining to its nature as an observational study with retrospective data and no control group. However, this is the largest series with an accompanying long follow up. As new departments begin to investigate the utility of new allograft products [24], this mature dataset will be a necessary reference. Surgical use of novel amniotic membrane products will comparatively suggest the benefits of a similar allograft from our cohort’s experience. The exclusion criteria for patients receiving dHACM in our institution included conditions that could exacerbate erectile dysfunction such as diabetes or vascular disease. Furthermore, a medical history of drug/alcohol abuse, autoimmune disease or prior hormonal therapy would make patients ineligible. Therefore, variables that could allow for a poor baseline SHIM and erectile function were not available in our cohort, to assess the wider impact of dHACM. Notwithstanding, diversity in demographic data, multiple institutions, and risk factors for poor erections pre RALP, should be compared in future trials.
Conclusion
Amniotic membranes offer capabilities of wound healing and nerve regeneration in medical practise. In this study, we demonstrated how the employment of the dHACM graft in robotic prostatectomy for prostate cancer is safe. Our findings indicate that the application of amniotic membrane/dHACM allowed for the return of potency at an average time of 3 months, with an overall shorter period for continence recovery. This experience confirms previously published studies, that amniotic membrane aids in functional outcome recovery, while future studies should focus on the long term impact of tumor biology post RALP. New amniotic membrane products can enhance our understanding of this adjuncts role in managing future uro-oncological patients.
References
Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS, Hoffman RM, Potosky AL, Stanford JL, Stroup AM, Van Horn RL, Penson DF (2013) Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med 368(5):436–445. https://doi.org/10.1056/NEJMoa1209978.PMID:23363497;PMCID:PMC3742365
Koob TJ, Rennert R, Zabek N et al (2013) Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J 10(5):493–500. https://doi.org/10.1111/iwj.12140
Lakmal K, Basnayake O, Hettiarachchi D (2021) Systematic review on the rational use of amniotic membrane allografts in diabetic foot ulcer treatment. BMC Surg 21(1):87. https://doi.org/10.1186/s12893-021-01084-8
Walsh PC, Donker PJ (1982) Impotence following radical prostatectomy: insight into etiology and prevention. J Urol 128(3):492–497. https://doi.org/10.1016/s0022-5347(17)53012-8
Basal S, Wambi C, Acikel C, Gupta M, Badani K (2013) Optimal strategy for penile rehabilitation after robot-assisted radical prostatectomy based on preoperative erectile function. BJU Int 111(4):658–665. https://doi.org/10.1111/j.1464-410X.2012.11487.x
Berryhill R Jr, Jhaveri J, Yadav R et al (2008) Robotic prostatectomy: a review of outcomes compared with laparoscopic and open approaches. Urology 72:15–23
Patel VR, Samavedi S, Bates AS, Kumar A, Coelho R, Rocco B, Palmer K (2015) Dehydrated human amnion/chorion membrane allograft nerve wrap around the prostatic neurovascular bundle accelerates early return to continence and potency following robot-assisted radical prostatectomy: propensity score-matched analysis. Eur Urol 67(6):977–980. https://doi.org/10.1016/j.eururo.2015.01.012
Ogaya-Pinies G, Palayapalam-Ganapathi H, Rogers T, Hernandez-Cardona E, Rocco B, Coelho RF, Jenson C, Patel VR (2018) Can dehydrated human amnion/chorion membrane accelerate the return to potency after a nerve-sparing robotic-assisted radical prostatectomy? Propensity score-matched analysis. J Robot Surg 12(2):235–243. https://doi.org/10.1007/s11701-017-0719-8
Razdan S, Bajpai RR, Razdan S, Sanchez MA (2019) A matched and controlled longitudinal cohort study of dehydrated human amniotic membrane allograft sheet used as a wraparound nerve bundles in robotic-assisted laparoscopic radical prostatectomy: a puissant adjunct for enhanced potency outcomes. J Robot Surg 13(3):475–481. https://doi.org/10.1007/s11701-018-0873-7
Coughlin G, Dangle PP, Palmer KJ, Samevedi S, Patel VR (2009) Athermal early retrograde release of the neurovascular bundle during nerve-sparing robotic-assisted laparoscopic radical prostatectomy. J Robot Surg 3(1):13–17. https://doi.org/10.1007/s11701-009-0127-9
Raffetto JD, Ligi D, Maniscalco R, Khalil RA, Mannello F (2020) Why venous leg ulcers have difficulty healing: overview on pathophysiology, clinical consequences, and treatment. J Clin Med 10(1):29. https://doi.org/10.3390/jcm10010029
Swim MM, Albertario A, Iacobazzi D, Caputo M, Ghorbel MT (2018) Amnion-based scaffold with enhanced strength and biocompatibility for in vivo vascular repair. Tissue Eng. https://doi.org/10.1089/ten.tea.2018.0175
Tartaro R, Caporossi T, Virgili G et al (2020) Insights on the human amniotic membrane in clinical practice with a focus on the new applications in retinal surgery. Regen Eng Transl Med. https://doi.org/10.1007/s40883-020-00190-y
Schatloff O, Chauhan S, Sivaraman A, Kameh D, Palmer KJ, Patel VR (2012) Anatomic grading of nerve sparing during robot-assisted radical prostatectomy. Eur Urol 61(4):796–802. https://doi.org/10.1016/j.eururo.2011.12.048
Ahlering TE, Eichel L, Chou D, Skarecky DW (2005) Feasibility study for robotic radical prostatectomy cautery-free neurovascular bundle preservation. Urology 65:994–997
Bourgeois M, Loisel F, Obert L, Pluvy I, Gindraux F (2019) Can the amniotic membrane be used to treat peripheral nerve defects? A review of literature. Hand Surg Rehabil 38(4):223–232. https://doi.org/10.1016/j.hansur.2019.05.006
Tettelbach W, Cazzell S, Reyzelman AM, Sigal F, Caporusso JM, Agnew PS (2019) A confirmatory study on the efficacy of dehydrated human amnion/chorion membrane dHACM allograft in the management of diabetic foot ulcers: a prospective, multicentre, randomised, controlled study of 110 patients from 14 wound clinics. Int Wound J 16(1):19–29. https://doi.org/10.1111/iwj.12976
Kang SG, Schatloff O, Haidar AM et al (2016) Overall rate, location, and predictive factors for positive surgical margins after robot-assisted laparoscopic radical prostatectomy for high-risk prostate cancer. Asian J Androl 18(1):123–128. https://doi.org/10.4103/1008-682X.148723
Gandaglia G, Ploussard G, Valerio M, Marra G, Moschini M, Martini A, Briganti A (2020) Prognostic implications of multiparametric magnetic resonance imaging and concomitant systematic biopsy in predicting biochemical recurrence after radical prostatectomy in prostate cancer patients diagnosed with magnetic resonance imaging–targeted biopsy. Eur Urol. Onc. 3(6):739–747
Alvim RG, Hughes C, Somma A, Nagar KK, Wong NC, La Rosa S, Monette S, Kim K, Coleman JA (2019) The potential risk of tumor progression after use of dehydrated human amnion/chorion membrane allograft in a positive margin resection model. Ther Adv Urol 29(11):1756287219837771. https://doi.org/10.1177/1756287219837771
de Carvalho PA, Barbosa JABA, Guglielmetti GB, Cordeiro MD, Rocco B, Nahas WC, Patel V, Coelho RF (2020) Retrograde release of the neurovascular bundle with preservation of dorsal venous complex during robot-assisted radical prostatectomy: optimizing functional outcomes. Eur Urol 77(5):628–635. https://doi.org/10.1016/j.eururo.2018.07.003 (Epub 2018 Jul 21 PMID: 30041833)
Coelho RF, Chauhan S, Orvieto MA, Sivaraman A, Palmer KJ, Coughlin G, Patel VR (2011) Influence of modified posterior reconstruction of the rhabdosphincter on early recovery of continence and anastomotic leakage rates after robot-assisted radical prostatectomy. Eur Urol 59(1):72–80. https://doi.org/10.1016/j.eururo.2010.08.025
Katz G, Rodriguez R (2001) Use of a modified American urological association symptom score for the evaluation of the quality of life of patients with prostate cancer. Urology 57(1):112–116. https://doi.org/10.1016/s0090-4295(00)00855-4
Elliott PA, Hsiang S, Narayanan R, Bierylo J, Chang SC, Twardowski P, Wilson TG (2021) Cryopreserved placental tissue allograft accelerates time to continence following robot-assisted radical prostatectomy. J Robot Surg 15(6):877–883
Funding
The study was partially funded by MiMedx (Marietta, GA, USA) who provided the grafts. Author Patel was a medical consultant for MiMedx.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Jonathan Noël, Anya Mascarenhas, Ela Patel, Sunil Reddy, Marco Sandri, Seetharam Bhat, Marcio Moschovas, Travis Rogers, Subuhee Ahmed and Daniel Stirt declare that they have no conflicts of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Noël, J., Mascarenhas, A., Patel, E. et al. Nerve spare robot assisted laparoscopic prostatectomy with amniotic membranes: medium term outcomes. J Robotic Surg 16, 1219–1224 (2022). https://doi.org/10.1007/s11701-022-01370-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01370-4