Abstract
A 76-year-old female with a history of high-grade transitional cell carcinoma (TCC) of the bladder presented with persistent nocturia and urge incontinence and was diagnosed with a necrotic bladder lesion. Cystoscopy revealed a 4 cm area of necrosis, ulceration, calcification, and fat. Transurethral biopsy confirmed the lesion to be benign, and two attempts to re-epithelialize the area of necrosis with cold scraping of exudate failed. Decision was then made to proceed with removal of necrotic lesion with bladder preservation. With the aid of concomitant cystoscopic visualization of the necrotic lesion, a robotic partial cystectomy with bladder reconstruction was performed. The patient tolerated the procedure, had an uneventful post-operative course, and remains asymptomatic and disease-free at last follow-up of 6 months. To our knowledge, this case represents the first report of a necrotic lesion as a complication of transurethral resection of a bladder tumor (TURBT) and the first description of a robotic partial cystectomy for the management of either benign or malignant bladder disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A 76-year-old female was diagnosed with a necrotic bladder lesion on surveillance cystoscopy for her history of bladder TCC. After failed conservative management, a robotic partial cystectomy was performed to excise this necrotic lesion and to reconstruct and preserve the remaining bladder.
Case report
A 76-year-old female initially presented with gross hematuria and was found on cystoscopy to have a 3-cm bladder mass involving the dome and posterior wall. Her medical history included emphysema, prior deep venous thrombosis, hyperlipidemia, and osteoporosis. Past surgical history was significant for bilateral hip replacements and spinal fusion. The patient underwent an uncomplicated transurethral resection of the bladder tumor (TURBT). Pathology revealed a high-grade TCC with invasion only into the lamina propria; however, only a small amount of muscularis propria was identified in the specimen. A repeat TURBT one month later revealed no residual carcinoma, with ample amount of muscularis propria in the sample. The patient was offered Bacillus Calmette–Guérin bladder instillation, but failed to receive treatment for unknown reasons. The patient returned six months later with urinary frequency, urgency, and dysuria, but no gross hematuria or urinary tract infection. A repeat cystoscopy revealed a necrotic-appearing bladder wall at the previous site of resection. This necrotic lesion was biopsied, and the patient was placed on antibiotics and anticholinergic medication for six weeks. Pathologic analysis revealed necrotic bladder wall, granulation tissue, and inflammation (Fig. 1). A follow-up cystoscopy in two months demonstrated a persistently large, necrotic, and devitalized ulceration with exposed fat and fibrinous exudate. Repeat cold transurethral scraping with a resectoscope confirmed the benign necrosis, granulation tissue, and inflammation seen previously.
After discussing treatment options, which included continued observation with surveillance and partial or radical cystectomy, the decision was made to proceed with robotic partial cystectomy of the necrotic bladder wall.
Robotic partial cystectomy technique
The patient is placed in a steep Trendelenberg position, the urethra is prepped into the field, and a carbon dioxide pneumoperitoneum is established with a Hassan cannula. Trocar placement is similar to that described for robotic prostatectomy: one periumbilical trocar, two lower quadrant 8 mm robotic trocars (each one slightly lateral to the mid-clavicular line), and two additional trocars, 10 and 12 mm, in the right lower quadrant [1]. The da Vinci Robot (Intuitive Surgical, Sunnyvale, CA, USA) is then docked to the patient, and the bladder filled with 250 cc of normal saline via a catheter.
Any large or small bowel adhesions to the bladder are lysed, mobilized, and retracted superiorly. The bladder is then released from the side wall and surrounding structures to ensure all margins of necrosis are exposed extravesically. Next, the robot is undocked, and the side surgeon, using the three-dimensional laparoscope to view the bladder extravesically, uses a grasper to stabilize the bladder on traction. A resectoscope is placed transurethrally into the bladder to locate the necrotic lesion, and the remainder of the bladder is inspected to ensure there are no other suspicious lesions. The margins of the 4 cm necrotic bladder mass are demarcated cystoscopically with a Collings hot knife (Cook Medical, Bloomington, IN, USA); in this case, a 1-cm margin from the anterior bladder neck was obtained. The Collings incision is deepened through the serosa circumferentially around the lesion, achieving full thickness. Again, these maneuvers are viewed in real time with the robotic laparoscope to confirm there is no inadvertent injury to surrounding structures or tissues (Fig 2). Once the cystotomy is made, allowing fluid to flow into the extraperitoneal space, the resectoscope is removed, a 20- french Foley catheter is passed into the bladder, and the robot is redocked to complete the bladder excision extravesically with the da Vinci system. To accomplish this, we prefer the Maryland bipolar forceps in the left hand, and the hot shears in the right (Intuitive Surgical, Sunnyvale, CA, USA) (Fig 2b). Thus, accurate identification and excision of the posterior margin is performed, allowing for easier excision of the remaining necrotic bladder wall, which is performed extravesically using robotic endoshears (Fig. 2b).
Once the necrotic bladder mass is completely excised, a running two-layer closure is performed, using 2-0 chromic suture for the internal layer and 2-0 vicryl suture for the seromuscular layer (Fig. 3). The anastomosis is tested with gentle irrigation through the catheter, and a self-suction bulb drain is placed extravesically.
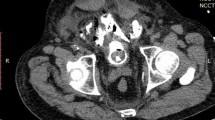
The operative time was 252 min. The patient tolerated surgery without complication, progressed well post-operatively, and was discharged home on postoperative-day 3. Final pathologic examination of the specimen revealed necrosis with extensive dystrophic calcification, fibrosis, chronic inflammation, and eosinophilic infiltration, without residual carcinoma (Figs. 4a, b).
Post-operative cystogram at 3 weeks with 200 cc demonstrated no extravasation, and the Foley catheter was removed (Fig. 5). Aside from occasional nocturia, the patient reported doing well, denying hematuria or dysuria, and remains free of disease on last surveillance, 6 months after surgery.
Discussion
Transurethral resection of bladder tumors is the treatment of choice for low-stage disease and is also utilized in the diagnostic evaluation of bladder tumors with higher stages. While TURBT is generally considered to have minimal morbidity, there are several well-recognized complications. The overall incidence of complications from TURBT has been reported to be anywhere from 5.1 to 43.3% [2–8]. The most common complication following TURBT is bleeding, with a reported incidence in the literature ranging from 2 to 13%, followed by bladder perforation with an incidence of 0.9–5% [2–8]. Hemorrhage requiring transfusion has been reported to occur between 2.3 and 13% of the time [2–4]. Other reported complications of TURBT include urinary tract infection (2–39%), medical complications, such as pulmonary embolism and myocardial infarction, reabsorption syndrome, urethral false passage creation, sepsis, ureteral orifice damage resulting in vesicoureteral reflux, tumor cell implanation following perforation, and intravesical explosions [2–9]. Published 30-day mortality rates for TURBT are low, all less than 1.3% [2, 6].
To our knowledge, the complication of bladder wall necrosis following TURBT has not been previously reported in the literature. Bladder necrosis has previously been described after hydrodistension in patients with interstitial cystitis, following pelvic artery embolization, after bilateral internal iliac artery ligation during surgery for rectal cancer, and secondary to clean intermittent catheterization [10–13]. Other known causes include intravesical irrigation/instillation solutions, radiation, indwelling catheters, calculi, infection, prostatic electrocoagulation, carcinoma, urinary retention, trauma, thromboembilism, and diabetes [14]. Options available for the treatment of a benign necrotic bladder mass include hyperbaric oxygen treatment, repeat TURBT, radical cystectomy with enterocystoplasty, partial cystectomy, and observation [15, 16]. We chose to proceed with a robotic partial cystectomy for this benign lesion.
Partial cystectomy is employed to treat bladder cancer in selected patients and can also be utilized for benign entities such as bladder diverticula, cavernous hemangiomas, cystic hytadid disease, ulcerative interstitial cystitis, colovesical fistula, vesicovaginal fistula, and localized endometriosis of the bladder [17, 18]. Over the last decade, there have been many reports in the literature of minimally invasive surgical techniques to treat various bladder pathologies. Laparoscopic radical cystectomy, laparoscopic partial cystectomy, and robotic radical cystectomy have all been described [19–23].
In 2004, Mariano and Tefilli presented their initial experience of laparoscopic partial cystectomy and lymphadenectomy for TCC in six carefully selected patients [21]. Mean surgical time was 205 min, mean estimated blood loss 200 mL, there were no significant perioperative complications, and all surgical margins were free of tumor. At a mean follow up of 30 months (range 12–50), there was one patient who developed local and metastatic disease. Wadwha and associates performed laparoscopic partial cystectomy with bilateral pelvic lymphadenectomy for three patients with urachal adenocarcinoma, with a mean operative time of 180 min, and a mean estimated blood loss of 150 cc [24]. No patient developed local or distant recurrence at a mean follow-up of 6.5 months (range 4.5–9). Laparoscopic partial cystectomy has also been described for urachal cysts, vesical endometriosis, bladder pheochromocytoma, bladder leiomyoma, post-traumatic splenic pseudocyst, bladder schwannoma, and endometrioid adenocarcinoma [25–31].
Recently, Sener et al. [32] reported performing a combined transurethral and laparoscopic partial cystectomy with robot-assisted bladder repair for the treatment of a deeply infiltrating 4-cm bladder endometrioma. Patient positioning and trocar placement were similar to those described in our case; however, we perform our exposure, extravesical excision, and reconstruction entirely robotically.
We have previously described the advantages of robotic surgery for reconstruction of the upper urinary tract [33]. Our growing experience with robotic reconstruction of lower urinary tract disease leads us to believe that the same advantages hold: increased instrument control, magnified, three-dimensional view, more working ports for the assistant, and increased surgeon comfort. This particular case involves a patient with a history of bladder TCC who developed a benign necrotic bladder lesion from TURBT. A robotic partial cystectomy was performed, based on the principles of open surgery, to excise the necrotic tissue and reconstruct the remaining healthy bladder. The patient will continue to receive appropriate surveillance for her history of bladder cancer. This communication represents the first report of a completely robotic partial cystectomy for either benign or malignant bladder disease, as well as the first report of bladder wall necrosis as a complication of TURBT.
Conclusion
Robotic surgery continues to find new utility in urologic surgery. While the use of laparoscopy for the management of bladder cancer has been reported, robotic surgery in this arena has not been described, and awaits further evaluation. Prospective multi-institutional studies and outcome analyses with comparisons to the gold standard of open surgery as well as laparoscopy are warranted to determine the exact role of robotic surgery in partial cystectomy for either benign or malignant disease.
References
Menon M, Shrivastava A, Kaul S, et al (2007) Vattikuti institute prostatectomy: contemporary technique and analysis of results. Eur Urol 51(3): 27–44
Dick A, Barnes R, Hadley H, et al (1980) Complications of transurethral resection of bladder tumors: prevention, recognition, and treatment. J Urol 124:810
Nieder AM, Meinbach DS, Kim SS, et al (2005) Transurethral bladder tumor resection: intraoperative and postoperative complications in a residency setting. J Urol 174:2307–2309
Collado A, Chechile GE, Salvador J, et al (2000) Early complications of endoscopic treatment for superficial bladder tumors. J Urol 164:1529–1531
Pycha A, Lodde M, Lusuardi L, et al (2003) Teaching transurethral resection of the bladder: still a challenge? Urology 62:46–48
Kondas J, Szentgyorgyi E (1992) Transurethral resection of 1250 bladder tumours. Int Urol Nephrol 24:35–42
Hollenbeck BK, Miller DC, Taub D, et al (2006) Risk factors for adverse outcomes after transurethral resection of bladder tumors. Cancer 106(7):1527–1535
Traxer O, Pasqui F, Gettegno B, et al (2004) Technique and complications of transurethral surgery for bladder tumors. BJU Int 94:492–496
Khan A, Masood J, Ghei M, et al (2007) Intravesical explosions during transurethral endoscopic procedures. Int Urol Nephrol 39(1):179–183
Zabihi N, Allee T, Maher MG, et al (2007) Bladder necrosis following hydrodistention in patients with interstitial cystitis. J Urol 177(1):149–152
Sieber PR (1994) Bladder necrosis secondary to pelvic artery embolization: case report and literature review. J Urol 151(2):422
Andriole GL, Sugarbaker PH (1985) Perineal and bladder necrosis following bilateral internal iliac artery ligation. Report of a case. Dis Colon Rectum 28(3):183–184
Reisman EM, Preminger GM (1989) Bladder perforation secondary to clean intermittent catheterization. J Urol 142(5):1316–1317
Grossklaus DJ, Franke JJ (2000) Vesical necrosis after hydrodistension of the urinary bladder in a patient with interstitial cystitis. BJU Int 86(1):140–141
Schulman CC, Pereira C (1970) Bladder regeneration: a case of total bladder necrosis followed by spontaneous regeneration. Acta Urol Belg 38(3):348–356
Bui QC, Lieber M, Withers HR, et al (2004) The efficacy of hyperbaric oxygen therapy in the treatment of radiation-induced late side effects. Int J Radiat Oncol Biol Phys 60(3):871–878
Sweeney P, Kursh ED, Resnick MI (1992) Partial cystectomy. Urol Clin North Am 19:701–711
Brannan W, Oschrer MG, Fuselier HA Jr, et al (1978) Partial cystectomy in the treatment of transitional cell carcinoma of the bladder. J Urol 119:213–215
Menon M, Hemal AK, Tewari A, et al (2003) Nerve-sparing robot-assisted radical cystoprostatectomy and urinary diversion. BJU Int 92(3):232–236
Turk I, Deger S, Winkelmann B, et al (2001) Laparoscopic radical cystectomy with continent urinary diversion (rectal sigmoid pouch) performed completely intracorporeally: the initial 5 cases. J Urol 165:1863–1866
Mariano MB, Tefilli MV (2004) Laparoscopic partial cystectomy in bladder cancer—initial experience. Int Braz J Urol 30(3):192–198
Denewer A, Kotb S, Hussein MBB, et al (1999) Laparoscopic assisted cystectomy and lymphadenectomy for bladder cancer: initial experience. Worl J Surg 23:608–611
Gill IS, Fergany A, Klein EA (2000) Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology 56:26–29
Wadhwa P, Kolla SB, Hemal AK (2006) Laparoscopic en bloc partial cystectomy with bilateral pelvic lymphadenectomy for urachal adenocarcinoma. Urology 67(4):837–843
Cadeddu JA, Boyle KE, Fabrizio MD, et al (2000) Laparoscopic management of urachal cysts in adulthood. J Urol 164:1526–1528
Ferzli G, Wenof M, Giannakakos A, et al (1993) Laparoscopic partial cystectomy for vesical endometrioma. J Laparoendosc Surg 3:161–165
Kozlowski PM, Mihm F, Winfield HN (2001) Laparoscopic management of bladder pheochromocytoma. Urology 57:365–367
Jeschke K, Wakonig J, Winzely M, et al (2002) Laparoscopic partial cystectomy for leiomyoma of the bladder wall. J Urol 168:2115–2116
Souka H, Loosemore T, Taylor RS (1997) Laparoscopic partial cystectomy for post-traumatic splenic pseudocyst. Endoscopy 29(7):S41
Geol H, Kim DW, Kim TH, et al (2005) Laparoscopic partial cystectomy for schwannoma of urinary bladder: case report. J Endourol 19(3):303–306
Nezhat CH, Malik S, Osias J, et al (2002) Laparoscopic management of 15 patients with infiltrating endometriosis of the bladder and a case of primary intravesical endometrioid adenosarcoma. Fertil Steril 78(4):872–875
Sener A, Chew BH, Duvdevani M, et al (2006) Combined transurethral and laparoscopic partial cystectomy and robot-assisted bladder repair for the treatment of bladder endometrioma. J Min Inv Gyn 13:243–248
Mufarrij PW, Shah OD, Berger AD, et al (2007) Robotic reconstruction of the upper urinary tract. J Urol 178(5):2002–2005
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Mufarrij, P.W., Penna, F.J., Tareen, B.U. et al. Necrotic mass after transurethral resection of a bladder tumor: novel management with robotic partial cystectomy. J Robotic Surg 1, 257–261 (2008). https://doi.org/10.1007/s11701-007-0041-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-007-0041-y