Abstract
Background
Bariatric surgery is an effective intervention for the management of severe obesity and its associated comorbidities, including metabolic abnormalities. This meta-analysis aimed to evaluate the impact of bariatric surgery on the triglyceride-glucose (TyG) index, a novel marker of insulin resistance and metabolic syndrome.
Methods
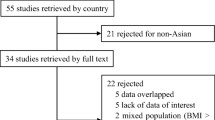
A systematic search was conducted in Embase, PubMed, Web of Science, and Scopus. The meta-analysis was performed using Comprehensive Meta-Analysis (CMA) V4 software. The overall effect size was determined by a random-effects meta-analysis and the leave-one-out approach.
Results
A total of 9 trials including 1620 individuals confirmed a significant reduction in TyG following bariatric surgery (weighted mean difference (WMD) − 0.770, 95% CI − 1.006, − 0.534, p < 0.001). In a sub-analysis according to the type of bariatric surgery there was a significant reduction in TyG index for Roux-en-Y gastric bypass (WMD − 0.775, 95% CI − 1.000, − 0.550, p < 0.001), and sleeve gastrectomy (WMD − 0.920, 95% CI − 1.368, − 0.473, p < 0.001). In a sub-analysis according to the follow-up duration there was similarly a significant reduction in TyG index for both < 12 months (WMD − 1.645, 95% CI − 2.123, − 1.167, p < 0.001), and ≥ 12 months follow-up (WMD − 0.954, 95% CI − 1.606, − 0.303, p < 0.001).
Conclusion
The results of this meta-analysis demonstrated a significant reduction in the TyG index following bariatric surgery, indicating improved insulin sensitivity and metabolic health. These findings highlight the potential of bariatric surgery as a valuable therapeutic option for individuals with obesity and its metabolic consequences.
Graphical Abstract






Similar content being viewed by others
Data Availability
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Khan SS, Ning H, Wilkins JT, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018;3(4):280–7.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Jamialahmadi T, Abbasifard M, Reiner Ž, et al. The effect of bariatric surgery on circulating levels of monocyte chemoattractant protein-1: a systematic review and meta-analysis. J Clin Med. 2022;11(23).
Jamialahmadi T, Alidadi M, Atkin SL, et al. Effect of bariatric surgery on flow-mediated vasodilation as a measure of endothelial function: a systematic review and meta-analysis. J Clin Med. 2022;11(14).
Jamialahmadi T, Banach M, Almahmeed W, et al. Impact of bariatric surgery on circulating PCSK9 levels as a marker of cardiovascular disease risk: a meta-analysis. Arch Med Sci. 2022;18(5):1372–7.
Jamialahmadi T, Reiner Ž, Alidadi M, et al. Effect of bariatric surgery on intima media thickness: a systematic review and meta-analysis. J Clin Med. 2022;11(20).
Jamialahmadi T, Reiner Ž, Alidadi M, et al. The effect of bariatric surgery on circulating levels of oxidized low-density lipoproteins is apparently independent of changes in body mass index: a systematic review and meta-analysis. Oxidative Med Cell Longev. 2021;2021.
Jamialahmadi T, Reiner Ž, Alidadi M, et al. Impact of bariatric surgery on pulse wave velocity as a measure of arterial stiffness: a systematic review and meta-analysis. Obes Surg. 2021;31(10):4461–9.
Nabavi N, Ghodsi A, Rostami R, et al. Impact of bariatric surgery on carotid intima-media thickness in patients with morbid obesity: a prospective study and review of the literature. Obes Surg. 2022;32(5):1563–9.
Norouzian Ostad A, Rajabzadeh F, Jamialahmadi T, et al. Impact of gastric bypass surgery on the liver fibrosis of patients with extreme obesity and nonalcoholic fatty liver disease in 30-month follow-up. Updat Surg. 2023;75(3):659–69.
Jamialahamdi T, Mirhadi E, Atkin SL, et al. Effect of bariatric surgery on serum amyloid a protein: a systematic review and meta-analysis. Obes Surg. 2023;33(11):3602–10.
Brzozowska MM, Isaacs M, Bliuc D, et al. Effects of bariatric surgery and dietary intervention on insulin resistance and appetite hormones over a 3 year period. Sci Rep. 2023;13(1):6032.
Cho YK, Kim HS, Jung CH, et al. Triglyceride-glucose index is a useful marker for predicting future cardiovascular disease and mortality in young Korean adults: a nationwide population-based cohort study. J Lipid Atheroscler. 2022;11(2):178.
Lopez-Jaramillo P, Gomez-Arbelaez D, Martinez-Bello D, et al. Association of the triglyceride glucose index as a measure of insulin resistance with mortality and cardiovascular disease in populations from five continents (PURE study): a prospective cohort study. Lancet Healthy Longev. 2023;4(1):e23–33.
Sendur SN, Isgin Atici K, Turan Demirci B, et al. The triglycerides–glucose index shows a stronger correlation with serum adiponectin levels than homeostasis model assessment of insulin resistance and quantitative insulin sensitivity check index. Metab Syndr Relat Disord. 2023.
Higgins JP. Cochrane handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration. http://www.cochrane-handbook.org. 2008.
Wells GA, Shea B, O’Connell Da, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
Borenstein M. Comprehensive meta‐analysis software. Systematic reviews in health research: meta‐analysis in context. 2022:535–48.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):1–10.
Sutton AJ, Abrams KR, Jones DR, et al. Methods for meta-analysis in medical research: Wiley Chichester; 2000.
Banach M, Serban C, Sahebkar A, et al. Impact of statin therapy on coronary plaque composition: a systematic review and meta-analysis of virtual histology intravascular ultrasound studies. BMC Med. 2015;13(1):1–21.
Banach M, Serban C, Ursoniu S, et al. Statin therapy and plasma coenzyme Q10 concentrations—a systematic review and meta-analysis of placebo-controlled trials. Pharmacol Res. 2015;99:329–36.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Shadnoush M, Rajabian Tabesh M, Asadzadeh-Aghdaei H, et al. Effect of bariatric surgery on atherogenicity and insulin resistance in patients with obesity class II: a prospective study. BMJ Open. 2023;13(6).
Frühbeck G, Catalán V, Ramírez B, et al. Serum levels of IL-1 RA increase with obesity and type 2 diabetes in relation to adipose tissue dysfunction and are reduced after bariatric surgery in parallel to adiposity. J Inflamm Res. 2022:1331–45.
Cheraghpour M, Alipour M, Tabesh MR, et al. Effects gastric bypass vs. sleeve gastrectomy on lipid indices in obese adults: a retrospective cohort. J Nutr, Fasting Health. 2022;10.
Cheng XY, Fu ZB, Xie W, et al. Preoperative circulating peroxiredoxin 1 levels as a predictor of non-alcoholic fatty liver disease remission after laparoscopic bariatric surgery. Front Endocrinol. 2022;13.
Wei R, Gao Z, Xu H, et al. Body fat indices as effective predictors of insulin resistance in obstructive sleep apnea: evidence from a cross-sectional and longitudinal study: BFI as predictors of IR in OSA. Obes Surg. 2021;31(5):2219–30.
Luo P, Cao YQ, Li PZ, et al. Insulin resistance remission following laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy in Chinese type 2 diabetes mellitus patients with a body mass index of 27.5–32.5 kg/m(2). Front Physiol. 2021;12.
Fonnegra CB, Valera RJ, Sarmiento-Cobos M, et al. The impact of rapid weight loss after bariatric surgery on insulin resistance measured by the triglyceride/HDL-cholesterol ratio and the triglyceride-glucose index. J Am Coll Surg. 2020;231(4):S32-S.
Pinto SL, Juvanhol LL, de Oliveira LL, et al. Changes in oxidative stress markers and cardiometabolic risk factors among Roux-en-Y gastric bypass patients after 3- and 12-months postsurgery follow-up. Surg Obes Relat Dis. 2019;15(10):1738–45.
Cazzo E, Callejas-Neto F, Pareja JC, et al. Correlation between post over preoperative surrogate insulin resistance indexes’ ratios and reversal of metabolic syndrome after Roux-en-Y gastric bypass. Obes Surg. 2014;24(6):971–3.
Liu H, Hu C, Zhang X, et al. Role of gut microbiota, bile acids and their cross-talk in the effects of bariatric surgery on obesity and type 2 diabetes. J Diabetes Investig. 2018;9(1):13–20.
Juárez-Fernández M, Román-Sagüillo S, Porras D, et al. Long-term effects of bariatric surgery on gut microbiota composition and faecal metabolome related to obesity remission. Nutrients. 2021;13(8):2519 (Note: MDPI stays neutral with regard to jurisdictional claims in published …; 2021).
Kuipers F, Bloks VW, Groen AK. Beyond intestinal soap—bile acids in metabolic control. Nat Rev Endocrinol. 2014;10(8):488–98.
Ryan KK, Tremaroli V, Clemmensen C, et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014;509(7499):183–8.
Palomäki VA, Lehenkari P, Meriläinen S, et al. Dynamics of adipose tissue macrophage populations after gastric bypass surgery. Obesity. 2023;31(1):184–91.
Osorio-Conles Ó, Vidal J, de Hollanda A. Impact of bariatric surgery on adipose tissue biology. J Clin Med. 2021;10(23):5516.
Chen MZ, Hudson CA, Vincent EE, et al. Bariatric surgery in morbidly obese insulin resistant humans normalises insulin signalling but not insulin-stimulated glucose disposal. PLoS One. 2015;10(4):e0120084.
Salehi M, D’Alessio DA. Mechanisms of surgical control of type 2 diabetes: GLP-1 is the key factor—maybe. Surg Obes Relat Dis. 2016;12(6):1230–5.
Funding
This work was supported by the Russian Science Foundation (Grant # 23–65-10014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Bariatric surgery is an effective for the management of severe obesity and its associated comorbidities.
• The results of this meta-analysis demonstrated a significant reduction in the TyG index following bariatric surgery.
• The results indicated improved insulin sensitivity and metabolic health.
• These findings highlight the potential of bariatric surgery as a valuable therapeutic option for individuals with obesity and its metabolic consequences.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jamialahamdi, T., Gadde, K.M., Nguyen, N.T. et al. Improvement of Triglyceride–Glucose Index Following Bariatric Surgery: a Systematic Review and Meta-analysis. OBES SURG 34, 741–750 (2024). https://doi.org/10.1007/s11695-023-06992-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06992-7