Abstract
Purpose
This study aimed to compare energy, macronutrients (quantity and quality), the overall dietary quality, and eating behaviors of patients undergoing laparoscopic sleeve gastrectomy (LSG) at different times since surgery.
Materials and Methods
This cross-sectional study included 184 adults at least 1 year post-LSG. Dietary intakes were assessed by a 147-item food frequency questionnaire. Macronutrient quality was assessed by computing the macronutrient quality index (MQI), carbohydrate quality index, fat quality index, and healthy plate protein quality index (HPPQI). The Healthy Eating Index (HEI)-2015 was used to assess diet quality. The Dutch Eating Behavior Questionnaire was used to assess eating behaviors. Based on the time since LSG, the time at which eating data were also collected, participants were categorized into three groups: 1–2 years (group 1), 2–3 years (group 2), and 3–5 years (group 3).
Results
Group 3 consumed significantly more energy and absolute carbohydrates than group 1. The MQI and HPPQI scores of group 3 were significantly lower than those of group 1.
The HEI score was significantly lower in group 3 compared to group 1, with a mean difference of 8.1 points. Compared to patients with 1–2 years following LSG, those with 2–3 and 3–5 years consumed more refined grains. Eating behavior scores did not differ between groups.
Conclusion
Patients at 3–5 years post-LSG consumed more energy and carbohydrates than those at 1–2 years after the surgery. Protein quality, overall macronutrient quality, and overall diet quality decreased as time passed following surgery.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is the most efficacious treatment for clinically severe obesity because it induces substantial and long-lasting weight loss and reduces obesity-related disorders [1]. According to the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) survey, there were 696,191 bariatric operations performed worldwide in 2018, before the emergence of the COVID-19 epidemic. Sleeve gastrectomy (SG) accounts for 55.4% of procedures, indicating that it has been the most prevalent procedure since 2014 [2]. Despite the overall success of bariatric surgery, some patients may experience insufficient weight loss or weight recurrence after the surgery [3, 4]. The insufficient weight reduction following bariatric surgery may lead to failure to improve or relapse of obesity-related comorbidities and the need for surgical revision [5].
Dietary intake and eating behaviors have been identified as two factors influencing bariatric surgery outcomes [6, 7]. Studies that followed patients within the first 2 years after the bariatric surgery consistently reported a marked decrease in energy consumption in the first few months after the surgery, followed by a progressive increase in energy intake [8,9,10]. However, few studies have investigated energy and macronutrient consumption over time after 2 years of surgery, when the rate of weight loss may slow or even weight recurrence may occur [11]. In addition, since prior nutritional research on bariatric surgery patients focused mostly on energy and macronutrient intake, it is unclear how the quality of the diet changes over time after surgery.
Eating behaviors have been documented to change after bariatric surgery in some studies, with a decrease in emotional and external eating and an increase in restrained eating [12,13,14,15]. A systematic review and meta-analysis on emotional eating, a component that has been studied more, revealed a significant reduction in emotional eating scores 4–18 months after bariatric surgery by combining the results of research with various surgical methods [16]. Since the majority of previous research has studied eating behaviors before and after bariatric surgery, it is unclear how postoperative eating behaviors are over time. Therefore, this cross-sectional study was conducted to examine energy, the quantity and quality of macronutrients, the overall quality of the diet, and eating behaviors in different patients, based on time after laparoscopic SG (LSG).
Methods
Participant recruitment and data collection for this cross-sectional study were performed between April and August 2022. Participants were recruited among the patients of a surgeon who underwent LSG between September 18, 2017, and March 16, 2021. The inclusion criteria for participants were being over the age of 18 and having undergone LSG (primary) for at least 1 year. Of the patients who underwent LSG during this time, 495 individuals were invited, of whom 200 individuals consented to participate in this study. After excluding those with mental or musculoskeletal disorders, cancer, or poor cooperation in answering questions, 184 patients were included in this study. Dietary intake and eating behavior were assessed in 181 and 182 participants, respectively. The bariatric surgery criteria were body mass index (BMI) levels ≥40 kg/m2 or 30<BMI<35 kg/m2 with a medical comorbidity/failure to respond to intensive medical treatment for at least 1 year. Before surgery, each participant was evaluated by a multidisciplinary team consisting of a bariatric surgeon, psychologist, and dietitian. In addition, the patricians were instructed to attend the clinics at 1, 3, 6, 9, 12, and 18 months post-surgery, followed by annual visits to receive dietary and physical activity recommendations. This study was approved by the Research Ethics Committees of National Nutrition and Food Technology Research Institute of Iran (No. IR.SBMU.NNFTRI.REC.1401.004), and each participant provided informed consent at the beginning of the study.
Dietary Assessment
A 147-item food frequency questionnaire (FFQ) was used to collect dietary data [17]. During the in-person interview, two trained nutritionists used the questionnaire to inquire about the frequency of consumption of each food item based on predefined portion sizes or household metrics. The intake of each food was then computed as g/d based on its reported frequency and quantity of consumption over the previous year. The daily intake of energy and nutrients was established using the food composition table of the US Department of Agriculture and the food composition table of Iran for traditional foods [17]. The absolute amount of macronutrients (g/d) and their intake relative to total energy intake (percentage of energy) were determined.
To evaluate the quality of macronutrients, the carbohydrate quality index (CQI), fat quality index (FQI), healthy plate protein quality index (HPPQI), and overall macronutrient quality index (MQI) were computed [18]. The CQI was calculated using four carbohydrate quality criteria: glycemic index, dietary fiber, whole-grain to total-grain carbohydrate ratio, and solid carbohydrate to solid + liquid carbohydrate ratio. The dietary glycemic index was determined using the international table of GI and a list of the GI of Iranian foods as follows [19, 20]:
Whole grains included bread produced with whole flour, rye, and bulgur (four food items), while refined grains included white rice, pasta, bread, and other bakery products made from refined flour (fourteen food items). Liquid carbohydrates were defined as carbohydrate intakes from sugar-sweetened beverages and fruit juices, while solid carbohydrates included carbohydrate intakes from non-liquid sources. These four criteria were categorized as quintiles, and scores 1–5 were given to the first through fifth quintiles, except for GI, which was scored in reverse; these scores were then added. Consequently, the CQI ranged between 4 and 20.
The FQI was a continuous score calculated as follows:
The HPPQI, a recently proposed index of protein quality in the diet, was calculated as follows:
The CQI, the PQI, and the HPPQI were categorized into quintiles to create the MQI, and then scored from 1 (first quintile) to 5 (fifth quintile), and then summed. The higher scores of the CQI and MQI represent better quality.
The overall quality of the diet was assessed using the Healthy Eating Index-2015 (HEI-2015) [21, 22]. The HEI-2015 consists of thirteen components, nine of which are referred to as adequacy components and four as moderation components. Adequacy components are dietary components that suggest consuming enough to assure nutrient adequacy for health, which include total fruits, total vegetables, greens and beans, dairy, total protein foods, seafood and plant proteins, and a fatty acid ratio. The moderation components include refined grains, added sugars, sodium, and saturated fats that should be consumed in moderation or in small quantities. The HEI-2015 score ranged between 0 and 100; the higher the score, the better the quality.
Eating Behavior
The Dutch Eating Behavior Questionnaire (DEBQ) was used to evaluate eating behaviors [23]. This 33-item questionnaire addresses three common dimensions of eating behavior: emotional eating (13 items), external eating (10 items), and restrained eating (10 items). Emotional eating was also divided into two subgroups: diffuse emotions (4 items; items 3, 8, 10, and 28) and clearly labeled emotions (9 items; the remaining items of emotional eating).
To obtain the raw score for each dimension, values from 1 (never) to 5 (very often) on a 5-point Likert scale were assigned, and then the values were added. The raw score was then divided by the number of items in each dimension to provide a score with equal weight for each dimension [24].
Physical Activity
The Persian-translated short form of the International Physical Activity Questionnaire (IPAQ) was used to assess physical activity [25]. Physical activity was determined as metabolic equivalent task (MET) minutes per week. The participants’ physical activity was divided into three levels: low (<600 MET-min/week), medium (600–3000 MET-min/week), and high (>3000 MET-min/week) according to the continuous IPAQ score.
Demographic and Anthropometric Data
Demographic characteristics of the participants, including age, smoking, education, occupation, marital status, and the prevalence of chronic diseases including diabetes, hypertension, and dyslipidemia, were collected using a questionnaire.
Weight, fat mass, and fat-free mass were measured by a bio-impedancemetry body composition analyzer (InBody 370S, BioSpace America, Inc.). The BMI was calculated as a ratio of weight (kg) to height (m2). Pre-operative BMI were extracted from their medical records. The percentage of total weight loss at the time of data collection was defined as [(preoperative weight – current weight) / preoperative weight] ×100. The percentage of excessive weight loss at the time of data collection was also defined as [(preoperative weight – current weight) / (preoperative weight- ideal body weight)] ×100. Ideal body weight was weight at the BMI of 25 kg/m2.
Statistical Analysis
For analyses, participants were divided into three groups based on time since surgery: 1–2 years (group 1), 2–3 years (group 2), and 3–5 years (group 3). The characteristics of the participants across the three groups were compared using analysis of variance (ANOVA) for continuous variables and Chi-squared for categorical variables. The analysis of covariance (ANCOVA) method was used to compare the quantity and quality of diet and eating behaviors across the three study groups, with age and sex adjustments. Data were presented as least-squared means (95% confidence interval (CI)) for normally distributed variables and geometric least-squared means (95% CI) for non-normally distributed variables. Post hoc comparisons were made using the LSD test. To optimize the study’s power, we decided not to include the other demographic covariates in the model, as the variables were comparable between groups. The SPSS statistical software (version 20; IBM Corp, Armonk, NY, USA) was used to perform the statistical analysis. Statistical significance was defined as p values ≤ 0.05.
Results
The mean age ± standard deviation of the participants was 43.4 ± 12.1, and 78.3% were women. The median time since surgery was 18.4, 29.8, and 44.8 months, respectively, in groups 1–3. Table 1 presents the characteristics of the participants according to their postoperative duration. The participants in groups 1 and 2 were significantly younger on average than those in group 3. Demographics and physical activity did not significantly differ between groups. Preoperative BMI and body composition were not significantly different across the groups, though weight and BMI at the time of the dietary assessment were highest in group 3.
Table 2 shows the dietary energy and macronutrient consumption based on postoperative time after adjusting for age and sex. Participants in group 3 consumed more energy than those in group 1 (p = 0.05). Intakes of macronutrients did not differ significantly between groups except for carbohydrate intake, which was higher in group 3 compared to group 1 (geometric means (95% CI) = 329 (281, 384) vs. 243 (195, 304); P = 0.032). The overall quality of macronutrient intake, as measured by MQI, decreased from group 1 to group 3, and it was significantly lower in group 3 compared to group 1 (means (95% CI) = 7.78 (6.75, 8.82) vs. 9.85 (8.37, 11.3); p = 0.026). Among the indices of macronutrient quality, the HPPQI was significantly different between the groups (p = 0.003). Despite the decrease in protein quality index in groups 2 and 3, the difference between group 1 and group 3 was statistically significant (p = 0.002). In addition, among the components of CQI, the ratio of solid to total carbohydrates was significantly higher in group 2 compared to group 1 (p = 0.037).
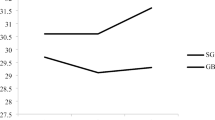
Table 3 presents the HEI-2015 and its dietary components based on postoperative time since surgery after adjustment for age and sex. The total HEI score decreased according to the time of surgery, the score was significantly lower in group 3 compared to group 1 (mean (95% CI) = 57.8 (53.9, 61.7) vs. 65.9 (60.3, 71.5); p = 0.021). Comparisons of the HEI dietary components between the groups showed that the intake of refined grains was significantly different between the groups. Pairwise comparison showed that participants in group 1 had a significantly lower intake of refined grains per 1000 kcal than those in group 2 (p = 0.021) and group 3 (p = 0.005). Furthermore, participants in group 3 consumed more sodium than those in group 2 (p = 0.041). On the other HEI components, there were no significant differences between the groups.
Table 4 shows the eating behavior scores of the patients based on postoperative time since LSG. None of the components of eating behaviors differed significantly between groups.
Discussion
Participants in this cross-sectional study at 3–5 years since LSG consumed more daily energy and carbohydrate than those with 1–2 years since surgery. In addition, the HPPQI, the MQI, and the HEI scores were significantly lower in groups of 3–5 years post-operation than those with 1–2 years. When the HEI dietary components were compared, those with time since surgery of 2–3 and 3–5 years consumed more refined grains than those at 1–2 years after the LSG. Eating behaviors were not significantly different between the groups.
Previous studies with short-term follow-up of patients undergoing bariatric surgery (up to 2 years) indicated a dramatic reduction in energy intake in the first few months after the surgery, followed by a gradual increase [8,9,10]. Consistent with our findings, a cross-sectional study comparing the energy and macronutrients intake between the three groups of RYGB patients based on time after surgery showed a significantly lower energy intake in patients with time passed surgery of up to 2 years than those 2–5 and over 5 years [26]. Energy intake in a prospective study of 61 SG patients progressively increased from 12 months to 5 years after the surgery but the increase was not statistically significant from 2 to 5 years after surgery. Comparing the macronutrient composition, an increase in % of energy from protein was observed for up to 12 months, followed by a reduction. Unlike protein, the percentage of energy derived from carbohydrates decreases until 12 months and then increases. The study did not report p values for different time points but the highest difference was observed between 6–12 months and 60 months [11].
This study is the first to compare the quality of the diet by time since surgery. The quality was assessed in two aspects: macronutrient quality and overall diet quality. The MQI is a multi-component index representing the overall quality of macronutrients [18]. In this study, the quality of all macronutrients was highest in those with a time since surgery of 1–2 years, although the differences reached statistical significance between groups with a time at the surgery of 3–5 compared to 1–2 for HPPQI. In addition, the MQI score was significantly lower in the 3–5 years post-surgery than in the 1–2 years. These findings imply that the overall quality of macronutrients and particularly protein quality reduce over time since surgery. Furthermore, the a priori dietary index of the HEI-2015 revealed a lower score for patients 3–5 years after surgery compared to those 1–2 years after surgery, with a mean difference of 8.1 points. The difference was clinically important according to the previous study, which defined a minimum clinically important difference of 3 [27]. Despite being statistically non-significant, the HEI mean variations between 2–3 years and 3–5 years following surgery were also clinically significant (6.4 points). When the dietary components of the HEI were compared, participants at 1–2 years after surgery consumed the least refined grains compared to those at 2–3 and 3–5 years after surgery. A study that followed the food ability consumption of LSG patients for 36 months found that rice and bread are better tolerated after 6 and 12 months of surgery, respectively [28]. The improvement in food tolerance may lead to increased consumption of refined grains in this study.
Eating behavior scores in this study did not significantly differ between the three groups, demonstrating that there were no notable variations in eating behaviors from 1 to 5 years after LSG. Reductions in emotional eating and external eating scores, but not restrained eating, were reported in 17 patients with RYGB and 10 patients with laparoscopic adjustable gastric banding when they lost 20% of their body weight compared to pre-operative time [14]. Moreover, the external eating score decreased between 3 and 6 months after surgery in a prospective study following 57 bariatric surgery patients, compared to before the surgery. However, the emotional eating score and the restrained eating score did not significantly change over this period [15]. A systematic review and meta-analysis gathered all study data on emotional eating behavior after bariatric surgery, an eating behavior that had received the most attention, regardless of the questionnaire used to assess eating behavior and surgical procedure. The majority of the included investigations were conducted up to 12 months following surgery, but a few studies examined the association over a longer duration (up to 36 months). Combining the results of 17 observational studies, the study found a significant reduction in the emotional eating score 4–18 months after surgery compared to pre-operative time. However, there was a substantial level of heterogeneity (I2 = 93%) among the studies’ findings. According to the systematic review, studies comparing eating behaviors at more than one postoperative time point showed no significant differences between any two-time points within the first 12 months after the surgery, while results for time points after 12 months were inconsistent [16]. Overall, it has not been well established how post-operative eating behavior changes over time, particularly in the intermediate and long term after bariatric surgery.
Restriction of stomach capacity, alteration in gut hormones, food tolerance, and postprandial discomfort are among some physiological factors that may affect energy intake, food preference, and eating behavior after bariatric surgery [28,29,30]. Some dietary changes occur in the early stages after surgery in response to the “dumping syndrome,” which is a prevalent complication of bariatric surgery [31]. Patients are recommended to reduce their simple carbohydrates and fats and instead increase their high-fiber and high-protein foods to alleviate the dumping syndrome symptoms [32], which may improve the quality of their diet. Moreover, the multiple nutritional and psychological examinations before surgery and over the first postoperative years may also improve dietary intake and eating behaviors [16]. Variations in the patient’s social and psychological state can also affect food intake and eating behavior, and these factors are especially significant in the mid-to-long term after surgery [16, 30]. These two factors can weaken the early effects of bariatric surgery on food intake and behavior. Therefore, the favorable effects of bariatric surgery on dietary intake and eating behaviors may be transient unless patients are provided with ongoing lifestyle and behavioral modification strategies after the surgery.
To the best of our knowledge, the quality of the diet after bariatric surgery according to the time since surgery has been investigated for the first time in this study. Assessing the quality of the diet based on two aspects of macronutrients and food group consumption, using a reliable and valid questionnaire to collect dietary data, determining eating behaviors postoperatively based on time since LSG, reducing variability by filling out the questionnaires only by two dietitians, and comparing dietary intakes and eating behaviors across the groups after adjusting for age and sex are among the strengths of the study. There are certain limitations to this study, however. First, the study’s ability to identify differences between groups may be hampered by the small number of patients in group 1 with 1–2 years after surgery. Second, the selection bias is possible and the sample included in the current study may not be representative of all LSG patients. Third, dietary intakes and eating behaviors were self-reported, which may be subject to self-reporting bias due to social desirability bias or recall bias [33]. Fourth, because the study was cross-sectional, we did not have preoperative dietary and eating behavior data. However, the purpose of this study was to look at dietary intake and eating behaviors after the first year of LSG with no comparison to before the surgery.
Conclusion
The energy and carbohydrate intakes were significantly higher in LSG patients at 3–5 years since the surgery compared to those at 1–2 years. The overall quality of the macronutrients, protein quality, and overall quality of the diet was lower in those with 3–5 years compared with 1–2 years after the surgery. No significant differences were observed in eating behaviors between the groups from 1 to 5 years after surgery. The findings suggest that a lower-quality diet is associated with a longer time after LSG. More studies, particularly prospective studies, are required to clarify how the quantity and quality of the diet and eating behaviors change over time after bariatric surgery.
References
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324:879–87.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg. 2021;31:1937–48.
El Ansari W, Elhag W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps—a scoping review. Obes Surg. 2021;31:1755–66.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy—a systematic review. Obes Surg. 2016;26:1326–34.
Franken RJ, Sluiter NR, Franken J, et al. Treatment options for weight regain or insufficient weight loss after sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2022;32:2035–46.
Cornejo-Pareja I, Molina-Vega M, Gómez-Pérez AM, et al. Factors related to weight loss maintenance in the medium–long term after bariatric surgery: a review. J Clin Med. 2021;10:1739.
Athanasiadis DI, Martin A, Kapsampelis P, et al. Factors associated with weight regain post-bariatric surgery: a systematic review. Surg Endosc. 2021;35:4069–84.
Bobbioni-Harsch E, Huber O, Morel P, et al. Factors influencing energy intake and body weight loss after gastric bypass. Eur J Clin Nutr. 2002;56:551–6.
Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence, and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4:640–6.
Andreu A, Moizé V, Rodríguez L, et al. Protein intake, body composition, and protein status following bariatric surgery. Obes Surg. 2010;20:1509–15.
Moizé V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-En-Y gastric bypass in a mediterranean population. J Acad Nutr Diet. 2013;113:400–10.
Hörchner R, Tuinebreijer W, Kelder H. Eating patterns in morbidly obese patients before and after a gastric restrictive operation. Obes Surg. 2002;12:108–12.
Mathus-Vliegen E. Long-term health and psychosocial outcomes from surgically induced weight loss: results obtained in patients not attending protocolled follow-up visits. Int J Obes. 2007;31:299–307.
Pepino MY, Bradley D, Eagon JC, et al. Changes in taste perception and eating behavior after bariatric surgery-induced weight loss in women. Obesity. 2014;22:E13–20.
Subramaniam K, Low W-Y, Lau P-C, et al. Eating behaviour predicts weight loss six months after bariatric surgery: a longitudinal study. Nutrients. 2018;10:1616.
Wong L, Zafari N, Churilov L, et al. Change in emotional eating after bariatric surgery: systematic review and meta-analysis. BJS Open. 2020;4:995–1014.
Mirmiran P, Esfahani FH, Mehrabi Y, et al. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13:654–62.
Vanegas P, Zazpe I, Santiago S, et al. Macronutrient quality index and cardiovascular disease risk in the Seguimiento Universidad de Navarra (SUN) cohort. Eur J Nutr. 2022;61:3517–30.
Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr. 2002;76:5–56.
Taleban F, Esmaeili M. Glycemic index of Iranian foods: Guideline for diabetic and hyperlipidemic patients (in persian). Tehran: National Nutrition and Food Technology Research Institute publication. 1999.
Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–602.
National Cancer Institute. HEI-2015 dietary components, constituents, and scoring standards. http://epi.grants.cancer.gov/hei/hei-2015-table1.html. Updated Feb 22, 2022.
Van Strien T, Frijters JE, Bergers GP, et al. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5:295–315.
Arhire LI, Niță O, Popa AD, et al. Validation of the Dutch Eating Behavior Questionnaire in a Romanian adult population. Nutrients. 2021;13:3890.
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28:53–8.
Berkowitz SA, O'Neill J, Sayer E, et al. Health center–based community-supported agriculture: An RCT. Am J Prev Med. 2019;57:S55–64.
Sioka E, Tzovaras G, Oikonomou K, et al. Influence of eating profile on the outcome of laparoscopic sleeve gastrectomy. Obes Surg. 2013;23:501–8.
Sarwer DB, Dilks RJ, West-Smith L. Dietary intake and eating behavior after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis. 2011;7:644–51.
Nielsen MS, Christensen BJ, Ritz C, et al. Factors associated with favorable changes in food preferences after bariatric surgery. Obes Surg. 2021;31:3514–24.
Sun W, Zhang Y, Shen Q, et al. Prevalence and risk factors for symptoms suggestive of hypoglycemia and early dumping syndrome after sleeve gastrectomy. Surg Obes Relat Dis. 2019;15:1439–46.
Berg P, McCallum R. Dumping syndrome: a review of the current concepts of pathophysiology, diagnosis, and treatment. Dig Dis Sci. 2016;61:11–8.
Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211.
Acknowledgements
This article has been extracted from the M.Sc. thesis written by Ms. Zahra Kamali.
Funding
This article has been financially supported by the National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Diet and eating behaviors were assessed according to times since SG.
• Macronutrient quality and overall diet quality were lower as time passed after the SG.
• Refined grain consumption increased as time passed after the SG.
• There were no significant differences in eating behavior based on time after SG.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kamali, Z., Tabesh, M.R., Moslehi, N. et al. Dietary Macronutrient Composition and Quality, Diet Quality, and Eating Behaviors at Different Times Since Laparoscopic Sleeve Gastrectomy. OBES SURG 33, 2158–2165 (2023). https://doi.org/10.1007/s11695-023-06651-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06651-x