Abstract
Background
There is a controversy on the suitable bariatric procedure for patients with BMI > 50 kg/m2. Many surgeons prefer the Roux en-Y gastric bypass (RYGB) while others resort to long biliopancreatic limb (BPL) one anastomosis gastric bypass (OAGB).
Methods
This study included patients with BMI > 50 kg/m2 who underwent 250-cm BPL OAGB with total bowel length (TBL) > 6 m and completed 24-month follow-up from July 2015 to November 2021. Demographic data with preoperative weight, BMI, hypertension (HTN), DM (HbA1C), Hb, iron, calcium, albumin, vitamin D, and parathormone levels (PTH) were recorded. Operative time, total bowel length (TBL), residual length (RBL), complications and postoperative weight, BMI, % of total weight loss (%TWL), HTN, DM, and alkaline reflux as well as Hb, iron, calcium, albumin, vitamin D, and PTH levels were recorded at 6, 12, 18, and 24 months.
Results
OAGB had a significant decrease in weight, BMI (25.6 ± 3.4 kg/m2 at 24 months) with %TWL of 48 ± 5% at 24 months. TBL and RBL were 6.7 ± 0.65 and 4.2 ± 0.65 m respectively. %BL (RBL/TBL*100) was 62.4 ± 3.3%. The HbA1C, HTN, and alkaline reflux incidence were 5.5 ± 0.29 gm%, 1.4%, and 3.7% respectively at 24 months. Hb, iron, calcium, albumin, and vitamin D showed a significant decrease but still within normal range, and PTH showed a significant increase at 24 months.
Conclusion
Long BP (250 cm) OAGB in patients with BMI > 50 kg/m2 with TWL > 6 m had good results in the achievement of weight loss and weight maintenance goals with remission of associated comorbidities as HTN and DM.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ideal bariatric procedure that provides the ideal postoperative body mass index (BMI) [1] with the remission of associated medical conditions as diabetes mellitus (DM) and hypertension (HTN) at minimal postoperative nutritional deficiencies and complications has not been found yet [2]. Many bariatric procedures are popular nowadays as sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and one anastomosis gastric bypass (OAGB) [3], and each one has its advantages and disadvantages. As a result, there is a controversy in the choice of the suitable procedure for each patient especially patients with body mass index (BMI) > 50 kg/m2 [4,5,6]. This class of patients usually resort to procedures that may fail to achieve target BMI [7] and require redo operations [8] or those that achieve the target BMI but exposes the patient to a debilitating course of nutritional deficiencies and malnutrition that may require reversal/redo operations or cause mortality. This may be due to subjective differences especially the total bowel length (TBL) and the absorptive capacity of the residual functioning part of the gastrointestinal tract.
The classical procedure of choice by most bariatric surgeons for patients with a BMI > 50 kg/m2 is the RYGB despite its technical difficulties and complications [9, 10]. OAGB has been introduced as an easy-to-perform one-stage procedure, and bariatric surgeons modified it to suit patients with BMI > 50 kg/m2 by increasing the length of the biliopancreatic limb (BPL) to accomplish more weight loss. However, the results obtained were not always the same. The YOMEGA study compared the 200-cm BPL OAGB with 150-cm alimentary limb (AL) and 50-cm BPL RYGB in patients with BMI > 40 kg/m2 or with BMI > 35 kg/m2 with associated medical conditions as DM, HTN, dyslipidemia, obstructive sleep apnea, or arthritis [11].
Yet, the application of long BPL OAGB in patients with BMI > 50 kg/ m2 has not been thoroughly studied in correlation with the TBL. In addition, the application of 250 cm in OAGB was not applied by many surgeons for fear of the nutritional drawbacks.
This study was different from the YOMEGA study in evaluating a 250-cm BPL OAGB (longer than 200 cm in YOMEGA) in patients with BMI > 50 kg/m2 (higher BMI than YOMEGA) specifically with more than 6-m TBL as a potential solution for obtaining the target BMI without causing morbidity for those patients with BMI > 50 kg/m2 guided by the TBL.
Patients and Methods
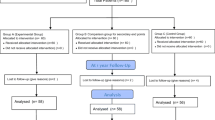
This study included 214 patients with BMI > 50 kg/m2 who underwent long BPL OAGB (250 cm) with TBL being measured (and found to be > 6 m) and completed 24-month follow-up from May 2015 to November 2021 in the department of general and bariatric surgery, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
Inclusion criteria were patients between 18 and 60 years that underwent a primary OAGB, TBL was more than 6 m, not suffering from preoperative GERD symptoms, fit for surgery, and with no history of abdominal surgeries.
Exclusion criteria were previous bariatric (or operations other than the specified lengths) or abdominal surgeries, patients with hiatus hernia or GERD on routine preoperative upper GI endoscopy, or with cardiovascular or chest problems.
Data Collection
Age, sex, height, weight, BMI, and associated medical conditions as DM (level of HbA1C), and HTN status where HTN was present with blood pressure > 140/90 mmHg were recorded preoperatively. Levels of hemoglobin (Hb), iron (Fe), calcium (Ca), albumin (Alb), vitamin D (Vit D), and parathormone (PTH) were recorded preoperatively.
The operative time and the incidence of postoperative complications were monitored. Total bowel length (TBL) was measured and recorded together with the residual bowel length (RBL) after bypassing 250 cm of proximal jejunum. Ratio (%BL) between TBL and RBL (RBL/TBL*100) representing the % of the remaining bowel length acting as the alimentary limb was calculated.
For each patient, the postoperative weight, BMI, percent of total weight loss (%TWL), the incidence of remission in preoperative medical conditions as HTN (defined as blood pressure below 140/90 mmHg without antihypertensive medications), DM (monitored through the change of level of HbA1C with level below 6 gm% without the use of antidiabetic drugs and insulin was considered as remission), incidence of alkaline reflux (by pH monitoring), and levels of Hb, Fe, Ca, Alb, Vit D, and PTH at 6, 12, 18, and 24 months were recorded. Patients underwent regular upper endoscopy at 6 monthly intervals to detect marginal ulcers and alkaline gastritis.
Preoperative Investigations
All patients underwent routine preoperative investigations including routine laboratory investigations, chest X-ray, pulmonary function test, ECG, echocardiography, and upper GI endoscopy.
Surgical Procedure
The gastric pouch was constructed by creating a window in the lesser omentum with a harmonic scalpel at the crow’s foot and firing a 45-mm cartridge horizontally and 4–5 cartridges vertically guided by a 36 F bougie for pouch calibration. The gastrojejunostomy was constructed at a distance of 250 cm from the duodenojejunal (DJ) junction by a 45-mm cartridge after measuring the entire length of the small intestine to make sure that TBL > 6 m. A minimum of 350 cm of the small intestine was ensured to be present distally to prevent the incidence of a short common limb (CL). Shorter lengths of the small intestine were allowed to have the RYGB procedure to be carried out instead and not included in the study. The enterotomies were then closed using V-lock sutures (V-lock 3/0, Medtronic™, Minneapolis, USA). The afferent and efferent loops were then fixed to the remnant stomach and the pylorus respectively using non-absorbable sutures to minimize reflux and facilitate the passage of food. An 18 F drain was left in the surgical bed.
Data Analysis
The collected data were revised, coded, tabulated, and introduced to a PC using the Statistical Package for Social Science (SPSS 26). Data were presented, and suitable analysis was done according to the type of data obtained for each parameter. Student’s t test was used in continuous values. Pearson’s chi-squared test and Fisher’s exact test were used in categorical variables. Repeated measure ANOVA was done to detect the significance of the difference between means measured more than twice for the same study group. Pairwise comparisons were done within each pair of successive readings of variables using paired t test with a correlation between them. Scatter plots and Pearson product-moment bivariate correlation were done to determine the association between two variables.
Results
From May 2015 to November 2021, 214 patients with BMI > 50 kg/m2 and had TBL > 6 m underwent 250-cm BPL OAGB who met the inclusion criteria and completed 24-month follow-up with 6-month interval.
Preoperative and Operative Data
The preoperative age, height, weight, BMI, level of HbA1C, Hb, Fe, Ca, Alb, Vit D, PTH, operative time, TBL, RBL, %BL sex distribution, and HTN status were detailed in (Table 1). The mean DM duration was 5.7 ± 2.3 years. The mean TBL, RBL, and %BL were 6.7 ± 0.65 m, 4.2 ± 0.65 m, and 62.4 ± 3.3%.
Postoperative Data
The postoperative weight, BMI, %TWL, level of HbA1C, Hb, Fe, Ca, Alb, Vit D, PTH, alkaline reflux incidence, and HTN status at 6, 12, 18, and 24 months were detailed in (Table 2). The rate of complications was 5.1% (11/214 patients) with 3 patients having a minor anastomotic leak, 3 patients having DVT, 2 patients having hematomas, 2 patients having marginal ulcers, and 1 patient having a chest infection (pneumococcal pneumonia).
Weight, BMI, and %TWL
The weight and BMI mean ± SD showed highly significant differences with time from preoperative value till 24 months postoperative by repeated measure ANOVA (p < 0.001) with highly significant differences, and positive correlation within each pair of successive readings by paired t test till 24 months postoperative (71.5 ± 10.8 kg and 25.6 ± 3.4 kg/m2 at 24 months respectively) (Tables 3 and 4). A histogram graphic representation of BMI preoperatively, at 12 months and 24 months, showed normal distribution of values (skewness value between 1 and − 1 with standard error 0.166) with most subjects distributed around BMI 25 kg/m2 denoting achievement of target BMI as seen in (Figs. 1, 2, and 3).
The %TWL mean ± SD showed highly significant differences with time from 6 months value till 24 months postoperative by repeated measure ANOVA (p < 0.001) with highly significant differences and positive correlation within each pair of successive readings by paired t test till 24 months postoperative (48 ± 5% at 24 months) (Tables 3 and 4).
A Pearson product-moment bivariate correlation was run to determine the relationship between the RBL and 24-month BMI. There was a strong positive correlation between the RBL and 24-month BMI which was statistically significant (r = 0.903, n = 214, p < 0.001). Scatter plot with linear fit of RBL against 24-month BMI was shown in (Fig. 4) with R2 = 0.815. A Pearson product-moment bivariate correlation was run to determine the relationship between the %BL and 24-month BMI. There was a strong positive correlation between the %BL and 24-month BMI which was statistically significant (r = 0.912, n = 214, p < 0.001). Scatter plot with linear fit of %BL against 24-month BMI was shown in (Fig. 5) with R2 = 0.832.
A RBL of 4.2 ± 0.65 m was enough to achieve and maintain the target BMI evidenced by the strong positive correlation between RBL and 24-month BMI. The application of nearly 40:60% ratio between the bypassed length and residual length allowed for achieving target BMI in this study.
DM and HTN
The level of HbA1C (mean ± SD) showed highly significant differences with time from preoperative value till 24 months of postoperative repeated measure ANOVA (p < 0.001) with highly significant differences and positive correlation within each pair of successive readings by paired t test till 18 months postoperative and negative correlation and non-significant difference (p = 0.432) within 18–24 months pair (5.5 ± 0.8 gm% at 18 months and 5.5 ± 0.2 gm% at 24 months) (Tables 3 and 4).
The HTN incidence showed a non-significant decrease from preoperative value till 6 months postoperative and a highly significant decrease from 6 to 12, 12 to 8, and 18 to 24 months (only 1.4% at 24 months) (Tables 1, 2, and 4).
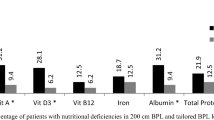
Nutritional Status
The level of Hb, Fe, Ca, albumin, vitamin D, and PTH (mean ± SD) showed highly significant differences with time from preoperative value till 24 months postoperative by repeated measure ANOVA (p < 0.001) (Table 3).
The level of Hb (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test till 24 months postoperative (11.4 ± 0.9 gm% at 24 months) (Tables 2 and 4). The level of Fe (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test (at preop. − 6 months, 6–12 months, and 18–24 months with 98.9 ± 9.7 mcg/dl at 24 months) and negative correlation with significant difference (p = 0.078) at 12–18 months (Tables 2 and 4).
The level of Ca (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test (at preop. − 6 months and 18–24 months with 8.7 ± 0.19 gm/dl at 24 months), negative correlation with a highly significant difference at 6–12 months, and positive correlation with a non-significant difference (p = 0.292) at 12–18 months (Tables 2 and 4). The level of albumin (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test (at preop. − 6 months, 6–12 months, and 18–24 months with 3.6 ± 0.2 gm/dl at 24 months) and negative correlation with a highly significant difference at 12–18 months (Tables 2 and 4).
The level of vitamin D (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test (at preop. − 6 months, 6–12 months, and 12–18 months) and negative correlation with a highly significant difference at 18–24 months (24.2 ± 4.1 ng/ml at 24 months) (Tables 2 and 4).
The level of PTH (mean ± SD) showed highly significant differences with positive correlation within each pair of successive readings by paired t test (at 6–12 months, 12–18 months, and 18–24 months with 69.9 ± 10.3 pg/ml at 24 months) and negative correlation with a highly significant difference at preop. − 6 months (Tables 2 and 4).
The effect size expressed by partial eta squared (ηρ2) ranged from 0.419 to 0.987 by repeated measure ANOVA yielding observed power 1.00.
Alkaline Reflux
The alkaline reflux incidence showed a highly significant decrease from 6 to 12, 12 to 18, and 18 to 24 months (only 3.7% at 24 months) (Tables 1, 2, and 4).
Discussion
OAGB had achieved its place as one of the popular bariatric procedures. However, the potentiality of the classic OAGB with 180-cm biliopancreatic limb (BPL) to achieve weight loss decreases with an increase in BMI. The YOMEGA study compared the 200-cm BPL OAGB with RYGB in patients with BMI < 50 kg/m2 and found no significant difference between them [11]. Yet, the patients with BMI > 50 kg/m2 will not achieve the target BMI with 180–200-cm BPL especially with long total bowel length (TBL), and many bariatric surgeons resort to long BPL RYGB. This study included patients with BMI > 50 kg/m2 who underwent 250-cm BPL OAGB and had TBL > 6 m to evaluate the effects and outcomes in those patients.
The procedure of OAGB adopted in this study was to do gastrojejunostomy at a distance of 250 cm from the DJ junction after creating a gastric pouch of 15 cm long on a 36 F bougie. A study by Plamper et al. [12] performed OAGB at a length of 250 cm for patients of BMI 50–60 while Madhok et al. [13] performed OAGB at 200 cm and both with good results. In this study, the procedure included measuring the TBL to ensure the presence of at least 350 cm distally to prevent the incidence of short common limb (CL) and decrease the nutritional deficiencies. Similar lengths of CL were suggested by Khalaj et al., Felsenreich et al., and Soong et al. [14,15,16]. OAGB had a short operative time with similar results obtained by Soong et al. and Lee et al. [16, 17].
As regards the weight, BMI, and %TWL preoperatively and at 6, 12, 18, and 24 months postoperatively, there was a significant decrease in weight and BMI from preoperative values to the postoperative values till 24 months in OAGB with a mean BMI of around 25 kg/m2 which was the target BMI (20–25 kg/m2). As regards the %TWL, OAGB achieved 48 ± 5%. A study by Singla et al. [18] reported a %TWL of 39.9% with OAGB in super obesity which was less than this study. Another study done by Bhandari et al. [3] stated that %TWL at 2 years was 43% in OAGB and also in a study by Soong et al. [16].
A RBL of 4.2 ± 0.65 m was enough to achieve and maintain the target BMI evidenced by the strong positive correlation between RBL and 24 months BMI. The application of nearly 40:60% ratio between the bypassed length and residual length allows for achieving target BMI without serious consequences in patients with > 6 m TBL.
As regards the HTN, there was a decrease in the percent of patients suffering from HTN from 61.7% preoperatively to 1.7% at 24 months as the results obtained by Magouliotis et al. [19]. The HTN status did not significantly change in the first 6 months then showed progressive improvement from 6 to 24 months. As regards the DM, there was a reduction in the mean level of HbA1C postoperatively to non-diabetic levels (< 6 gm%) at 18 and remained almost stationary till 24 months. This confirms the metabolic effect in remission of HTN and DM of OAGB.
The incidence of alkaline reflux was 7.5% at 6 months that was reduced to 3.7% at 24 months. In literature, alkaline reflux varied from 0.6 to 10% [20]. The adopted method of the long gastric pouch as in the study by Soong et al. and Deitel et al. [16, 21] and the application of draining technique in the form of side-to-side anastomosis of gastrojejunostomy and fixation of afferent and efferent loops to help passage of gastric contents distally lead to a relatively low incidence of alkaline reflux in comparison to other studies as that performed by Keleidari et al. [22].
The levels of Hb, Fe, Ca, and vitamin D levels showed progressive decrease till 24 months but remain within normal range. The albumin levels decrease till 18 months then showed a tendency to stabilize by 24 months. The PTH level remains high normal till 12 months then became higher than the normal range with a tendency to rise till 24 months.
OAGB had decreased nutrient absorption owing to the bypassed part of the proximal jejunum. As the long BP OAGB had 250 cm of excluded jejunum, nutrients absorbed in the proximal jejunum had more deficiencies in OAGB as the results confirmed in the reduction of Hb, Fe, Ca, albumin, and Vit D levels with significant differences with time despite the compliance of the patients to postoperative vitamin and mineral supplements, yet the levels are within the normal range. PTH levels showed a significant increase with time yet were mildly elevated after 12 months due to chronically impaired absorption of Ca.
Similar results concerning Hb, Alb, Ca, and PTH were obtained by Soong et al. [16] and Omar et al. [23]. Similar differences between OAGB and RYGB concerning low Hb levels were obtained by Lee et al. [17]. Carbajo et al. [24] stated that in OAGB nutritional deficiencies and malnutrition are increasingly reported when the bypassed jejunum is > 250 cm. Charalampos et al. [25] did not find any differences in nutritional deficiencies in OAGB between BP limbs of 200, 250, and 300 cm. IFSO Consensus Conference recommends OAGB to be performed if BMI > 50 with the presence of a suitable length common channel in OAGB if BP is to be more than 200 cm [26].
There is a controversy on the length of bypassed jejunum ranging from 150 to 350 cm in OAGB [14, 27]. This study concluded that OAGB with 250 cm bypassed part of jejunum (with nearly 40:60% ratio between the bypassed part and the remaining part) is a good choice for patients with BMI > 50 kg/m2 [16] after ensuring the presence of at least 350 cm distally as CL (it was 4.2 ± 0.65 m in this study) with comparable results with long BP RYGB (BP limb = 150 cm and AL = 100 cm) with < 30 BMI kg/m2 after 2 years and more than 45% TWL. Both procedures have good metabolic effects on associated comorbidities with remission of HTN and DM. OAGB had a more yet non-significant incidence of alkaline reflux due to long gastric pouch (15 cm) and drainage procedure through fixation of afferent and efferent limbs and if present can be controlled by medications up to 50% of cases. RYGB had significantly more operative time as confirmed by Soong et al. [16] with more incidence of complications.
Conclusion
Two-hundred fifty-cm BPL OAGB with > 350-cm common limb in patients with BMI > 50 kg/m2 and total bowel length more than 6 m can achieve a target BMI of 25 kg/m2 with nearly 40:60% ratio between the bypassed length and residual length. This was accompanied by remission of associated comorbidities as HTN and DM without causing serious nutritional deficiencies with the maintenance of target BMI for at least 2 years. The limitations of this study were the absence of long-term follow-up till 5–10 years, the absence of comparative design, and the need for larger number of patients.
References
Carbajo MA, Jiménez JM, Luque-de-León E, et al. Evaluation of weight loss indicators and laparoscopic one-anastomosis gastric bypass outcomes. Sci Rep. 2018;8:1961. https://doi.org/10.1038/s41598-018-20303-6.
Cadena-Obando D, Ramírez-Rentería C, Ferreira-Hermosillo A, et al. Are there really any predictive factors for a successful weight loss after bariatric surgery? BMC Endocr Disord. 2020;20:20. https://doi.org/10.1186/s12902-020-0499-4.
Bhandari M, Leon-Ballesteros GP, Kosta S, et al. Surgery in patients with super obesity: medium-term follow-up outcomes at a high-volume center. Obesity. 2019;27:1591–7. https://doi.org/10.1002/oby.22593.
DeMaria EJ, Schauer P, Patterson E, et al. The optimal surgical management of the super obese patient: the debate. Surg Innov. 2005;12(2):107–21.
Parikh MS, Shen R, Weiner M, et al. Laparoscopic bariatric surgery in super-obese patients (BMI>50) is safe and effective: a review of 332 patients. Obes Surg. 2005;15:858–63.
Peterson K, Anderson J, Boundy E, et al. Rapid evidence review of bariatric surgery in super obesity (BMI ≥ 50 kg/m2). J Gen Intern Med. 2017;32(Suppl 1):S56–64. https://doi.org/10.1007/s11606-016-3950-5.
Bloomston M, Zervos EE, Camps MA, et al. Outcome following bariatric surgery in super versus morbidly obese patients: does weight matter? Obes Surg. 1997;7:414–9.
Poublon N, Chidi I, Bethlehem M, et al. One anastomosis gastric bypass vs. Roux-en-Y gastric bypass, remedy for insufficient weight loss and weight regain after failed restrictive bariatric surgery. Obes Surg. 2020;30:3287–94. https://doi.org/10.1007/s11695-020-04536-x.
Meytes V, Chang GC, Iskandar M, et al. Gastric bypass is safe and effective for the super-super-obese patient. Ann Laparosc Endosc Surg. 2017;2:38. https://doi.org/10.21037/ales.2017.02.27.
Ribeiro R, Guerra A, Viveiros O. Diverted MGB: a new procedure. In: Deitel M. (eds) Essentials of mini ‒ one anastomosis gastric bypass. Springer, Cham (2018). https://doi.org/10.1007/978-3-319-76177-0_30
Robert M, Espalieu P, Pelascini E, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393:1299–309.
Plamper A, Lingohr P, Nadal J, et al. Comparison of mini-gastric bypass with sleeve gastrectomy in a mainly super-obese patient group: first results. Surg Endosc. 2017;31:1156–62.
Madhok B, Mahawar KK, Boyle M, et al. Management of super-super obese patients: comparison between mini (one anastomosis) gastric bypass and sleeve gastrectomy. Obes Surg. 2016;26:1646–9.
Khalaj A, Motamedi MAK, Mousapour P, et al. Protein-calorie malnutrition requiring revisional surgery after one-anastomosis-mini-gastric bypass (OAGB-MGB): case series from the Tehran Obesity Treatment Study (TOTS). Obesity Surgery. 2019. https://doi.org/10.1007/s11695-019-03741-7.
Felsenreich DM, Langer FB, Eichelter J, et al. Bariatric surgery–how much malabsorption do we need?—a review of various limb lengths in different gastric bypass procedures. J Clin Med. 2021;10:674. https://doi.org/10.3390/jcm10040674.
Soong TC, Lee MH, Lee WJ, et al. Long-term efficacy of bariatric surgery for the treatment of super-obesity: comparison of SG, RYGB, and OAGB. Obes Surg. 2021;31:3391–9. https://doi.org/10.1007/s11695-021-05464-0.
Lee WJ, Almalki OM, Ser KH, et al. Randomized controlled trial of one anastomosis gastric bypass versus Roux-En-Y gastric bypass for obesity: comparison of the YOMEGA and Taiwan studies. Obes Surg. 2019;29:3047–53. https://doi.org/10.1007/s11695-019-04065-2.
Singla V, Aggarwal S, Singh B, et al. Outcomes in super obese patients undergoing one anastomosis gastric bypass or laparoscopic sleeve gastrectomy. Obesity Surgery. 2019;29:1242–7. https://doi.org/10.1007/s11695-018-03673-8.
Magouliotis DE, Tasiopoulou VS, Tzovaras G. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for morbid obesity: a meta-analysis. Clin Obes. 2018;8:159–69. https://doi.org/10.1111/cob.12246.
Kassir R, Petrucciani N, Debs T, et al. Conversion of one anastomosis gastric bypass (OAGB) to Roux-en-Y gastric bypass (RYGB) for biliary reflux resistant to medical treatment: lessons learned from a retrospective series of 2780 consecutive patients undergoing OAGB. Obes Surg. 2020;30:2093–8. https://doi.org/10.1007/s11695-020-04460-0.
Deitel M, Hargroder D, Peraglie C. Mini-gastric bypass for bariatric surgery increasing worldwide. Austin J Surg. 2016;3(3):1092–6. https://doi.org/10.26420/austinjsurg.2016.1092.
Keleidari B, Dehkordi MM, Shahraki MS, et al. Bile reflux after one anastomosis gastric bypass surgery: a review study. Ann Med Surg. 2021;64:102248. https://doi.org/10.1016/j.amsu.2021.102248.
Omar I, Sam MA, Pegler ME, et al. Effect of one anastomosis gastric bypass on haematinics, vitamin D and parathyroid hormone levels: a comparison between 150 and 200 cm bilio-pancreatic limbs. Obes Surg. 2021;31:2954–61. https://doi.org/10.1007/s11695-021-05281-5.
Carbajo MA, Luque-de-León E, Jiménez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27:1153–67.
Charalampos T, Maria N, Vrakopoulou VGZ, et al. Tailored one anastomosis gastric bypass: 3-year outcomes of 94 patients. Obes Surg. 2019;29:542–51.
Ramos AC, Chevallier JM, Mahawar K, et al. IFSO (International Federation for Surgery of Obesity and Metabolic Disorders) consensus conference statement on one-anastomosis gastric bypass (OAGB-MGB): results of a modified Delphi study. Obes Surg. 2020;30:1625–34.
Carbajo MA, Vázquez-Pelcastre R, Aparicio-Ponce R, et al. 12-year old adolescent with super morbid obesity, treated with laparoscopic one anastomosis gastric bypass (LOAGB/BAGUA): a case report after 5-year follow-up. Nutr Hosp. 2015;31(5):2327–32. https://doi.org/10.3305/nh.2015.31.5.8884.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Keypoints
• Long BP (250 cm) OAGB in patients with BMI>50 kg/m2 with TWL>6 ms had good results in the achievement of target BMI.
• Long BP (250 cm) OAGB in patients with BMI>50 kg/m2 helps in the remission of associated comorbidities as HTN and DM.
• Long BP (250 cm) OAGB in patients with BMI>50 kg/m2 does not cause significant nutritional deficiencies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eskandaros, M.S. Outcomes and Effects of 250-cm Biliopancreatic Limb One Anastomosis Gastric Bypass in Patients with BMI > 50 kg/m2 with Total Bowel Length > 6 m: a 2-Year Follow-up. OBES SURG 32, 2309–2320 (2022). https://doi.org/10.1007/s11695-022-06078-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06078-w