Abstract
Background
Sleeve gastrectomy (SG) is the most common bariatric procedure performed worldwide. It accounts for more than 50% of primary bariatric surgeries performed each year. Recent long-term data has shown an alarming trend of weight recidivism. Some authors have proposed the concurrent use of a non-adjustable gastric band to decrease long-term sleeve failure.
Objective
To compare the outcomes (weight loss) and safety (rate of complication and presence of upper GI symptoms) between SG and BSG.
Methods
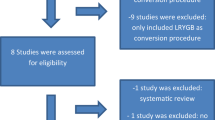
A systematic search with no language or time restrictions was performed to identify relevant observational studies and randomized controlled trials (RCT) evaluating people with morbid obesity undergoing SG or SGB for weight loss. An inverse-of-the-variance meta-analysis was performed by random effects model. Heterogeneity was assessed using Cochrane X2 and I2 analysis.
Results
A total of 7 observational studies and 3 RCT were included in the final analysis. There were 911 participants pooled from observational studies and 194 from RCT. BSG showed a significant higher excess of weight loss (% EWL). The difference among groups was clinically relevant after the third year where the weighted mean difference (SMD) was 16.8 (CI 95% 12.45, 21.15, p < 0.0001), while at 5 years, a SMD of 25.59 (16.31, 34.87, p < 0.0001) was noticed. No differences related to overall complications were noticed. Upper GI symptoms were up to three times more frequent in the BSG group (OR 3.26. CI 95% 1.96, 5.42, p < 0.0001).
Conclusions
According to the results, BSG is superior to SG in weight loss at 5 years but is associated with a higher incidence of upper GI symptoms. However, these conclusions are based mainly on data obtained from observational studies. Further RCT are needed to evaluate the effect and safety of BSG.
Graphical abstract









Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–94.
Li J-F, Lai D-D, Lin Z-H, Jiang T-Y, Zhang A-M, Dai J-F. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity. Surg Laparosc Endosc Percutan Tech. 2014;24(1):1–11.
Wang Y, Song Y, Chen J, Zhao R, Xia L, Cui Y, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy for super super obese and super obese: systematic review and meta-analysis of weight results, comorbidity resolution. Obes Surg. 2019;29(6):1954–64.
Vitiello A, Berardi G, Velotti N, De Palma GD, Musella M. Should sleeve gastrectomy be considered only as a first step in super obese patients? 5-year results from a single center. Surg Laparosc Endosc Percutan Tech. 2020;31(2):203–207.
Boza C, Daroch D, Barros D, León F, Funke R, Crovari F. Long-term outcomes of laparoscopic sleeve gastrectomy as a primary bariatric procedure. Surg Obes Relat Dis. 2014;10(6):1129–33.
Bhandari M, Ponce de Leon-Ballesteros G, Kosta S, Bhandari M, Humes T, Mathur W, et al. Surgery in patients with super obesity: medium-term follow-up outcomes at a high-volume center. Obesity. 2019;27(10):1591–7.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, Gfrerer L, Ludvik B, Zacherl J, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20(5):535–40.
Baltasar A, Serra C, Pérez N, Bou R, Bengochea M. Re-sleeve gastrectomy. Obes Surg. 2006;16(11):1535–8.
Gagner M, Rogula T. Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch. Obes Surg. 2003;13(4):649–54.
Fobi MAL, Lee H. The surgical technique of the fobi-pouch operation for obesity (the transected silastic vertical gastric bypass). Obes Surg. 1998;8(3):283–8.
Frezza EE, Herbert H, Wachtel MS. Combined laparoscopic gastric banding and stomach reduction (GBSR): initial experience after 1 year. Obes Surg. 2008;18(6):690–4.
Karcz WK, Karcz-Socha I, Marjanovic G, Kuesters S, Goos M, Hopt UT, et al. To band or not to band—early results of banded sleeve gastrectomy. Obes Surg. 2014;24(4):660–5.
Chamany T, Makam R, Kanth R. Early experience of laparoscopic banded sleeve gastrectomy using gabp ring. Abstracts from the 19th World Congress of the International Federation for the Surgery of Obesity & Metabolic Disorders (IFSO), Montreal, Canada 26–30 August 2014. Obes Surg. 2014;24(8):1136–378.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Univ Ottawa. 2014
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021) [Internet]. Cochrane; 2021. Available from: www.training.cochrane.org/handbook
Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ. 1998;316(7129):469.
Biljana M, Jelena M, Branislav J, Milorad R. Bias in meta-analysis and funnel plot asymmetry. Stud Health Technol Inform. 1999;68:323–8.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Soliman AMS, Lasheen M. Effect of banded laparoscopic sleeve gastrectomy on weight loss maintenance: comparative study between banded and non-banded sleeve on weight loss. Bariatr Surg Pract Patient Care. 2015;10(3):99–104.
Tognoni V, Benavoli D, Bianciardi E, Perrone F, Ippoliti S, Gaspari A, et al. Laparoscopic sleeve gastrectomy versus laparoscopic banded sleeve gastrectomy: first prospective pilot randomized study. Gastroenterol Res Pract. 2016;2016:1–5.
Fink JM, Hoffmann N, Kuesters S, Seifert G, Laessle C, Glatz T, et al. Banding the sleeve improves weight loss in midterm follow-up. Obes Surg. 2017;27(4):1098–103.
Lemmens L, Van Den Bossche J, Zaveri H, Surve A. Banded sleeve gastrectomy: better long-term results? A long-term cohort study until 5 years follow-up in obese and superobese patients. Obes Surg. 2018;28(9):2687–95.
Bhandari M, Mathur W, Kosta S, Mishra AK, Cummings DE. Banded versus nonbanded laparoscopic sleeve gastrectomy: 5-year outcomes. Surg Obes Relat Dis. 2019;15(9):1431–8.
Fink JM, von Pigenot A, Seifert G, Laessle C, Fichtner-Feigl S, Marjanovic G. Banded versus nonbanded sleeve gastrectomy: 5-year results of a matched-pair analysis. Surg Obes Relat Dis. 2019;15(8):1233–8.
Fink JM, Hetzenecker A, Seifert G, Runkel M, Laessle C, Fichtner-Feigl S, et al. Banded versus nonbanded sleeve gastrectomy. Ann Surg. 2020;272(5):690–5.
Gentileschi P, Bianciardi E, Siragusa L, Tognoni V, Benavoli D, D’Ugo S. Banded sleeve gastrectomy improves weight loss compared to nonbanded sleeve: midterm results from a prospective randomized study. J Obes. 2020;1(2020):1–7.
Bhandari M, Ponce de Leon-Ballesteros G, Kosta S, Bhandari M, Humes T, Mathur W, et al. Surgery in patients with super obesity: medium-term follow-up outcomes at a high-volume center. Obesity. 2019;27(10).
Clapp B, Wynn M, Martyn C, Foster C, O’Dell M, Tyroch A. Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis. 2018;14(6):741–7.
Nedelcu M, Noel P, Iannelli A, Gagner M. Revised sleeve gastrectomy (re-sleeve). Surg Obes Relat Dis. 2015;11(6):1282–8.
Noel P, Nedelcu A, Eddbali I, Gagner M, Danan M, Nedelcu M. Five-year results after resleeve gastrectomy. Surg Obes Relat Dis. 2020;16(9):1186–91.
Fobi MA, Lee H. SILASTIC ring vertical banded gastric bypass for the treatment of obesity: two years of follow-up in 84 patients [corrected]. J Natl Med Assoc. 1994;86(2):125–8.
Fobi MAL. Placement of the GaBP ring system in the banded gastric bypass operation. Obes Surg. 2005;15(8):1196–201.
Salvi P, Kosta S, Fobi M, Bhandari M, Reddy M, Gusani R, et al. Banded sleeve gastrectomy and one anastomosis gastric bypass/mini-gastric bypass for treatment of obesity: a retrospective cohort comparative study with 6 years follow-up. Obes Surg. 2020;30(4):1303–9.
Shoar S, Khorgami Z, Brethauer SA, Aminian A. Banded versus nonbanded Roux-en-Y gastric bypass: a systematic review and meta-analysis of randomized controlled trials. Surg Obes Relat Dis. 2019;15(5):688–95.
Magouliotis DE, Tasiopoulou VS, Svokos KA, Svokos AA, Sioka E, Tzovaras G, et al. Banded vs. non-banded Roux-en-Y gastric bypass for morbid obesity: a systematic review and meta-analysis. Clin Obes. 2018;8(6):424–33.
Buchwald H, Buchwald JN, McGlennon TW. Systematic review and meta-analysis of medium-term outcomes after banded Roux-en-Y gastric bypass. Obes Surg. 2014;24(9):1536–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conclusions
According to the results, BSG is a safe and effective procedure with acceptable rates of perioperative and band-related complications. Mid- (3 years) and long-term (5 years) weight loss may be superior in BSG compared to SG but may come at the expense of a higher incidence of upper GI symptoms such as food intolerance, vomiting, and regurgitation. A 6.5-cm band is associated to a higher incidence of upper GI symptoms, in comparison to a band greater than 7 cm.
However, these findings are mainly based on data obtained from observational studies. Further RCT are needed to validate these results, as well as studies with longer follow-up to assess safety and efficacy of BSG at long term.
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent Statements
Non-applicable.
Conflict of Interest
Guillermo Ponce de Leon-Ballesteros has nothing to disclose. Gustavo Romero-Velez has nothing to disclose. Raigam Jafet Martinez-Portilla has nothing to disclose. Xavier Pereira has nothing to disclose. Ivonne Roy-Garcia has nothing to disclose. Mathias AL Fobi has ownership of share in Bariatec Corporation. Miguel F Herrera has nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
- Banded sleeve gastrectomy (BSG) has been proposed as an alternative to SG as it can limit gastric pouch dilation.
- Seven case-control studies and three randomized clinical trials have compared the outcomes between SG and BSG.
- BSG has significant higher %EWL compared to SG.
- BSG showed a higher frequency of upper gastrointestinal symptoms on follow-up on observational studies. According to the RCT, there was no significant difference among groups.
Article Category: Systematic review. No previous presentation in a meeting or to a society.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ponce de Leon-Ballesteros, G., Romero-Velez, G., Martinez-Portilla, R.J. et al. Comparison of Outcomes Between Banded and Non-banded Sleeve Gastrectomy: a Systematic Review and Meta-analysis. OBES SURG 32, 1–12 (2022). https://doi.org/10.1007/s11695-022-06043-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06043-7