Abstract
Background
The aim of this study was to evaluate the effect of bariatric surgery on the defined daily dose of levothyroxine (DDD LT4), thyroid-stimulating hormone (TSH), and free thyroxine (fT4) in female patients with hypothyroidism until 48 months after surgery.
Methods
A retrospective observational study of hypothyroid patients who underwent bariatric surgery. Changes in DDD LT4, TSH, and fT4 over a 48 month period after surgery were analyzed.
Results
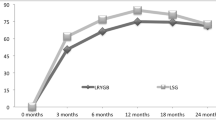
Thirty-seven patients were included: 27 Roux-en-Y gastric bypass (RYGB), 6 sleeve gastrectomy (SG), 3 adjustable gastric band, and 1 one anastomosis gastric bypass. The median DDD LT4 decreased from 125 µg at baseline to 100 µg 12 months after surgery. From 24 to 48 months after surgery, the median DDD LT4 was stable at 125 µg. Most dose adjustments occurred during the first 24 months after surgery. In the time period of 24–48 months after surgery, the dose remained stable in 73.1% of the RYGB patients and in 60.0% of the SG patients. After 48 months in the RYGB group, no significant change in TSH and fT4 levels was observed.
Conclusions
Bariatric surgery led to frequent dose adjustments during the first 2 years after surgery. However, 24–48 months after surgery in the majority of patients, the dosage remained stable. No significant change in TSH and fT4 was observed 48 months after RYGB. In the first 2 years after surgery, clinicians should frequently monitor TSH and fT4 for individual dose adjustment of levothyroxine. Thereafter, the frequency of monitoring may be decreased.
Graphical abstract



Similar content being viewed by others
References
Chang SH, Stoll CRT, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149:275–87.
Yska JP, van Roon EN, de Boer A, et al. Remission of type 2 diabetes mellitus in patients after different types of bariatric surgery: a population-based cohort study in the United Kingdom. JAMA Surg. 2015;150:1126–33.
Padwal R, Brocks D, Sharma AM. A systematic review of drug absorption following bariatric surgery and its theoretical complications. Obes Rev. 2010;11:41–50.
Gadiraju S, Lee CJ, Cooper DS. Levothyroxine dosing following bariatric surgery. Obes Surg. 2016;26:2538–42.
Zendel A, Abu-Ghanem Y, Dux J, et al. The impact of bariatric surgery on thyroid function and medication use in patients with hypothyroidism. Obes Surg. 2017;27:2000–4.
Rudnicki Y, Slavin M, Keidar A. The effect of bariatric surgery on hypothyroidism: sleeve gastrectomy versus gastric bypass. Surg Obes Relat Dis. 2018;14:1297–303.
Yska JP, van der Meer DH, Dreijer AR, et al. Influence of bariatric surgery on the use of medication. Eur J Clin Pharmacol. 2016;72:203–9.
Guan B, Chen YY, Yang J, et al. Effect of bariatric surgery on thyroid function in obese patients: a systematic review and meta-analysis. Obes Surg. 2017;27:3292–305.
Gokosmanoglu F, Aksoy E, Onmez A, et al. Thyroid homeostasis after bariatric surgery in obese cases. Obes Surg. 2020;30:274–8.
Julià H, Benaiges D, Mollà P, et al. Changes in thyroid replacement therapy after bariatric surgery: differences between laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Obes Surg. 2019;29:2593–9.
Pedro J, Cunha F, Souteiro P, et al. The effect of the bariatric surgery type on the levothyroxine dose of morbidly obese hypothyroid patients. Obes Surg. 2018;28:3538–43.
Raftopoulos Y, Gagné DJ, Papasavas P, et al. Improvement of hypothyroidism after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2004;14:509–13.
Szomstein S, Avital S, Brasesco O, et al. Laparoscopic gastric bypass in patients on thyroid replacement therapy for subnormal thyroid function - prevalence and short-term outcome. Obes Surg. 2004;14:95–7.
Michalaki MA, Vagenakis AG, Leonardou AS, et al. Thyroid function in humans with morbid obesity. Thyroid. 2006;16:73–8.
Azran C, Porat D, Fine-Shamir N, et al. Oral levothyroxine therapy postbariatric surgery: biopharmaceutical aspects and clinical effects. Surg Obes Relat Dis. 2019;15:333–41.
Gkotskina M, Michalaki M, Mamai I, et al. Improved levothyroxine pharmacokinetics after bariatric surgery. Thyroid. 2013;23:414–9.
Rubio IGS, Galrão AL, Santo MA, et al. Levothyroxine absorption in morbidly obese patients before and after Roux-en-Y gastric bypass (RYGB) surgery. Obes Surg. 2012;22:253–8.
Fierabracci P, Martinelli S, Tamberi A, et al. Weight loss and variation of levothyroxine requirements in hypothyroid patients after bariatric surgery. Thyroid. 2016;26:499–503.
Fazylov R, Soto E, Cohen S, et al. Laparoscopic Roux-en-Y gastric bypass surgery on morbidly obese patients with hypothyroidism. Obes Surg. 2008;18:644–7.
Author information
Authors and Affiliations
Contributions
All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Study on the long-term effect of bariatric surgery on the use of levothyroxine.
• Most dose changes of levothyroxine occurred in the first 2 years after surgery.
• Twenty-four to 48 months after surgery, most patients had a stable dosage of levothyroxine.
• Frequent monitoring of TSH and fT4 is advised in the first 2 years after surgery.
Rights and permissions
About this article
Cite this article
Yska, J.P., Arfman, I.J., van Oijen, M.A. et al. Long-term Effect of Bariatric Surgery on the Use of Levothyroxine and Thyroid Levels. OBES SURG 32, 742–748 (2022). https://doi.org/10.1007/s11695-021-05810-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05810-2