Abstract
Introduction
Levothyroxine (LT4) requirements can presumably be modified differently after laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG). The present study compared changes in LT4 dose in hypothyroid subjects undergoing LRYGB or LSG 2 years after the procedure.
Material and Methods
A 2-year follow-up observational study was conducted in a prospective cohort of obese patients who had undergone bariatric surgery and were receiving LT4. Indication for the type of surgical procedure was based on clinical criteria. Repeated measures ANOVA models were used to examine differences within and between groups.
Results
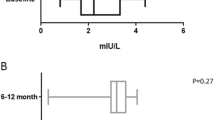
Thirty-five consecutive patients were included for analysis: 22 LRYGB and 13 LSG. Total daily LT4 dosage decreased in the LSG group (133.7 ± 50.3 mcg/day at baseline to 104.3 ± 43.3 mcg/day at 2 years; p = 0.047) whereas it remained stable in the LRYGB group (129.5 ± 46.1 mcg/day at baseline to 125.2 ± 55.7 mcg/day at 2 years; p = 1.000). Differences between groups became significant at 24 months. Daily weight-based LT4 dose increased in the LRYGB group (1.11 ± 0.38 mcg/kg day at baseline to 1.57 ± 0.74 mcg/kg day at 2 years; p = 0.005) with no significant changes in the LSG group (1.15 ± 0.35 mcg/kg day at baseline vs 1.11 ± 0.49 mcg/kg day at 2 years; p = 1.000).
Conclusion
LRYGB and LSG showed different changes in LT4 requirements 2 years after surgery. There was an early decrease in daily total LT4 dose requirements after LSG, which suggests an early preventive reduction to be validated in future studies.




Similar content being viewed by others
References
Dall’Asta C, Paganelli M, Morabito A, et al. Weight loss through gastric banding: effects on TSH and thyroid hormones in obese subjects with normal thyroid function. Obesity. 2010;18:854–7.
Gadiraju S, Lee CJ, Cooper DS. Levothyroxine dosing following bariatric surgery. Obes Surg. 2016;26:2538–42. https://doi.org/10.1007/s11695-016-2314-x.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type °2 diabetes. Diabet Med. 2011;28:628–42. https://doi.org/10.1111/j.1464-5491.2011.03306.x.
Sundaram U, McBride C, Shostrom V, et al. Prevalence of preoperative hypothyroidism in bariatric surgery patients and postoperative change in thyroid hormone requirements. Bariatr Surg Pract Patient Care. 2013;8:147–51. https://doi.org/10.1089/bari.2013.0006.
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2013;37:889–91.
Brethauer SA, S FAC, Mattar SG, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis Elsevier Inc. 2018;14:259–63. https://doi.org/10.1016/j.soard.2017.12.013.
Welbourn R, Pournaras DJ, Dixon J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the second IFSO global registry report 2013–2015. Obes Surg. 2018;28:313–22.
Padwal R, Brocks D, Sharma AM. A systematic review of drug absorption following bariatric surgery and its theoretical implications. Obes Rev. 2010;11:41–50.
Fierabracci P, Martinelli S, Tamberi A, et al. Weight loss and variation of levothyroxine requirements in hypothyroid obese patients after bariatric surgery. Thyroid. 2016;26:499–503. https://doi.org/10.1089/thy.2015.0473.
Zendel A, Abu-Ghanem Y, Dux J, et al. The impact of bariatric surgery on thyroid function and medication use in patients with hypothyroidism. Obes Surg. 2017;27:2000–4.
Pedro J, Cunha F, Souteiro P, et al. The effect of the bariatric surgery type on the levothyroxine dose of morbidly obese hypothyroid patients. Obes Surg. 2018:1–6.
Sioka E, Tzovaras G, Perivoliotis K, et al. Impact of laparoscopic sleeve gastrectomy on gastrointestinal motility. Gastroenterol Res Pract. 2018;2018:1–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29849586%0A, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC5907392%0A, https://www.hindawi.com/journals/grp/2018/4135813/.
Burton PR, Yap K, Brown WA, et al. Changes in satiety, supra- and infraband transit, and gastric emptying following laparoscopic adjustable gastric banding: a prospective follow-up study. Obes Surg. 2011;21:217–23.
Raftopoulos Y, Gagne DJ, Papasavas P, et al. Improvement of hypothyroidism after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2004;14:509–13. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L38570291%5Cn, https://doi.org/10.1381/096089204323013514%5Cn, http://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=09608923&id=doi:10.1381%2F096089204323013514&atitle=Improvement+of+hypot.
Fazylov R, Soto E, Cohen S, et al. Laparoscopic Roux-en-Y gastric bypass surgery on morbidly obese patients with hypothyroidism. Obes Surg. 2008;18:644–7.
Aggarwal S, Modi S, Jose T. Laparoscopic sleeve gastrectomy leads to reduction in thyroxine requirement in morbidly obese patients with hypothyroidism. World J Surg. 2014;38:2628–31.
Pirola I, Formenti AM, Gandossi E, et al. Oral liquid l-thyroxine (l-T4) may be better absorbed compared to l-T4 tablets following bariatric surgery. Obes Surg. 2013;23:1493–6.
Fallahi P, Ferrari SM, Antonelli A. Oral l-thyroxine liquid versus tablet in patients with hypothyroidism without malabsorption: a prospective study. Endocrine Springer US. 2016;52:597–601.
Rubio IGS, Galrão AL, Santo MA, et al. Levothyroxine absorption in morbidly obese patients before and after Roux-En-Y gastric bypass (RYGB) surgery. Obes Surg. 2012;22:253–8.
Gkotsina M, Michalaki M, Mamali I, et al. Improved levothyroxine pharmacokinetics after bariatric surgery. Thyroid. 2013;23:414–9. https://doi.org/10.1089/thy.2011.0526.
Nakatani H, Kasama K, Oshiro T, et al. Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism. 2009;58:1400–7.
Bétry C, Challan-Belval MA, Bernard A, et al. Increased TSH in obesity: evidence for a BMI-independent association with leptin. Diabetes Metab. Elsevier Masson SAS. 2015;41:248–51. https://doi.org/10.1016/j.diabet.2014.11.009.
Santini F, Pinchera A, Marsili A, et al. Lean body mass is a major determinant of levothyroxine dosage in the treatment of thyroid diseases. J Clin Endocrinol Metab. 2005;90:124–7. https://doi.org/10.1210/jc.2004-1306.
Kulovitz MG, Kolkmeyer D, Conn CA, et al. Medical weight loss versus bariatric surgery: does method affect body composition and weight maintenance after 15% reduction in body weight? Nutrition Elsevier Inc. 2014;30:49–54. https://doi.org/10.1016/j.nut.2013.06.008.
Zalesin KC, Franklin BA, Lillystone MA, et al. Differential loss of fat and lean mass in the morbidly obese after bariatric surgery. Metab Syndr Relat Disord. 2010;8:15–20. https://doi.org/10.1089/met.2009.0012.
Muñoz R, Hernández J, Palacio A, et al. El ejercicio físico disminuye la pérdida de masa magra en pacientes obesos sometidos a cirugía bariátrica. Rev Chil Cir. 2016;68:411–6.
Acknowledgements
We thank Miss Christine O’Hara for the review of the English version of the manuscript. CIBEROBN and CIBERESP are an initiative of the Instituto de Salud Carlos III (ISCIII).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Julià, H., Benaiges, D., Mollà, P. et al. Changes in Thyroid Replacement Therapy after Bariatric Surgery: Differences between Laparoscopic Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy. OBES SURG 29, 2593–2599 (2019). https://doi.org/10.1007/s11695-019-03890-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03890-9