Abstract
Purpose
Identify, 18 months after bariatric surgery, the binge eating variation and its relation with weight regain or loss.
Materials and Methods
Cross-sectional, retrospective study with 108 patients, assisted by an obesity walk-in clinic of a specialized hospital in São Paulo (Brazil), who had undergone bariatric surgery a minimum of 18 months previously. The anthropometric and clinic data were collected from medical records, and binge eating symptoms were evaluated with the application of the Binge Eating Scale (BES). Scale outcomes were related to weight regain and loss at the application moment.
Results
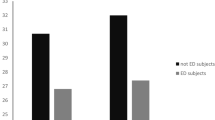
The average age (standard error) of the sample was 47 years (±0.91) and 93% were female. Patients had lost 52.2% of their body weight and regained 4.7% of their weight 18 months after the surgery. The elapsed surgical time (> 50 months) was associated with a higher gross weight (p<0.0001).
Conclusions
Bariatric surgery has been shown to be effective for improving diabetes mellitus as well as for controlling obesity. The variation in binge eating intensity 18 months after bariatric surgery is a factor that interferes in the amount of weight regained. The presence of binge eating symptoms negatively affects the % total weight loss (%TWL).
Graphical abstract


Similar content being viewed by others
References
Ministério da Saúde. Secretaria de Vigilância em Saúde. Secretaria de Atenção à saúde. Política Nacional de Promoção da Saúde. 3a edição. Brasília; 2006. 60 p.
Sarwer DB, Dilks RJ, Spitzer JC, et al. Changes in dietary intake and eating behavior in adolescents after bariatric surgery: an ancillary study to the teen-LABS consortium. Obes Surg. 2017;27(12):3082–91.
Al-Najim W, Docherty NG, le Roux CW. Food intake and eating behavior after bariatric surgery. Physiol Rev. 2018;98(3):1113–41.
Opozda M, Wittert G, Chur-Hansen A. Patients’ expectations and experiences of eating behaviour change after bariatric procedures. Clin Obes. 2018;8(5):355–65.
Russel SM, Valle V, Spagni G, et al. Physiologic mechanisms of type II diabetes mellitus remission following bariatric surgery: a meta-analysis and clinical implications. J Gastrointest Surg. 2020;24(3):728–41.
Ii MT, Forcina DV, De Almeida BO, Ribeiro-Jr MAF. The role of bariatric surgery on diabetes mellitus type 2 control. 2008;21(3):130–2.
Meany G, Conceição E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22(2):87–91.
Pinto-Bastos A, De Lourdes M, Brand I, et al. Weight loss trajectories and psychobehavioral predictors of outcome of primary and reoperative bariatric surgery : a 2-year longitudinal study. Surg Obes Relat Dis. 2019;15:1104–12.
Brandão I, Pinho AM, Arrojado F, et al. Diabetes mellitus tipo 2, depressão e alterações do comportamento alimentar em doentes submetidos a cirurgia bariátrica. Acta Medica Port. 2016;29(3):176–81.
Behary P, Miras AD. Food preferences and underlying mechanisms after bariatric surgery. Proc Nutr Soc. 2015;74(4):419–25.
Ivezaj V, Wiedemann AA, Grilo CM. Food addiction and bariatric surgery: a systematic review of the literature. Obes Rev. 2017;18(12):1386–97.
Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA - J Am Med Assoc. 2014;311(22):2297–304.
Buchwald H. The evolution of metabolic/bariatric surgery. Obes Surg. 2014;24(8):1126–35.
Freitas S, Lopes CS, Coutinho W, et al. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215–20.
Chao AM, Wadden TA, Faulconbridge LF, et al. Binge-eating disorder and the outcome of bariatric surgery in a prospective, observational study: two-year results. Obesity. 2016;24(11):2327–33.
Dawes AJ, Maggard-Gibbons M, Maher AR, et al. Mental health conditions among patients seeking and undergoing bariatric surgery a meta-analysis. JAMA - J Am Med Assoc. 2016;315(2):150–63.
Associação Brasileira para o estudo da obesidade e da síndrome metabólica (ABESO). Diretrizes brasileiras de obesidade 2016. VI Diretrizes Bras Obesidade. 2016;7–186.
Brasil. Guia Alimentar para a População Brasileira. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Coordenação-Geral da Política de Alimentação e Nutrição. 5–145 p.
Nikiforova I, Barnea R, Azulai S, et al. Analysis of the association between eating behaviors and weight loss after laparoscopic sleeve gastrectomy. Obes Facts. 2019;12(6):618–31.
Ribeiro G, Giapietro H, Belarmino L, et al. Depressão, Ansiedade e Compulsão Alimentar Antes e Após Cirurgia Bariátrica: Problemas que persistem. Arq Bras Cir Dig. 2018;31(1):1–4.
Smith KE, Orcutt M, Steffen KJ, et al. Loss of control eating and binge eating in the 7 years following bariatric surgery. Obes Surg. 2019;29(6):1773–80.
Freire CC, Zanella MT, Segal A, Arasaki CH, Matos MIR, Carneiro G. Associations between binge eating, depressive symptoms and anxiety and weight regain after Roux-en-Y gastric bypass surgery. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2021;26:191–9. https://doi.org/10.1007/s40519-019-00839-w.
Grupski AE, Hood MM, Hall BJ, et al. Examining the Binge Eating Scale in screening for binge eating disorder in bariatric surgery candidates. Obes Surg. 2013;23(1):1–6.
Cella S, Fei L, D’Amico R, et al. Binge eating disorder and related features in bariatric surgery candidates. Open Med. 2019;14(1):407–15.
Ricca V, Mannucci E, Moretti S, et al. Screening for binge eating disorder in obese outpatients. Compr Psychiatry. 2000;41(2):111–5.
Marek RJ, Heinberg LJ, Lavery M, et al. A Review of psychological assessment instruments for use in bariatric surgery evaluations. Psychol Assess. 2016;28(9):1142–57.
Järvholm K, Bruze G, Peltonen M, Marcus C, Flodmark C, Henfridsson P, et al. 5-year mental health and eating pattern outcomes following bariatric surgery in adolescents : a prospective cohort study. 2020;4(March).
Spirou D, Raman J, Smith E. Psychological outcomes following surgical and endoscopic bariatric procedures : a systematic review. Obes Rev. 2019;2020:1–24. https://doi.org/10.1111/obr.12998.
Järvholm K, Olbers T, Peltonen M, et al. Binge eating and other eating-related problems in adolescents undergoing gastric bypass: results from a Swedish nationwide study (AMOS). Appetite. 2018;127:349–55.
Peterhänsel C, Linde K, Wagner B, et al. Subtypes of personality and ‘locus of control’ in bariatric patients and their effect on weight loss, eating disorder and depressive symptoms, and quality of life. Eur Eat Disord Rev. 2017;25(5):397–405.
Vanoh D, Shahar S, Mahmood NRKN. Association between nutrient adequacy and psychosocial factors with overall rate of weight loss after bariatric surgery. Asia Pac J Clin Nutr. 2015;24(4):610–9.
Sociedade Brasileira de Cirurgia Bariátrica e Metabólica (SBCBM). Técnicas cirúrgicas. Técnicas Cirúrgicas. 2017.
Opolski M, Chur-Hansen A, Wittert G. The eating-related behaviours, disorders and expectations of candidates for bariatric surgery. Clin Obes. 2015;5(4):165–97. https://doi.org/10.1111/cob.12104.
Sarwer DB, Allison KC, Wadden TA, et al. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surg Obes Relat Dis. 2019;15(4):650–5.
Nasirzadeh Y, Kantarovich K, Wnuk S, et al. Binge eating, loss of control over eating, emotional eating, and night eating after bariatric surgery: results from the Toronto Bari-PSYCH cohort study. Obes Surg. 2018;28(7):2032–9.
Conceição EM, Mitchell JE, Pinto-Bastos A, et al. Stability of problematic eating behaviors and weight loss trajectories after bariatric surgery: a longitudinal observational study. Surg Obes Relat Dis. 2017;13(6):1063–70.
Cardoso C, Maria F, Zanella T, Segal A, Haruo C, Isabel M, et al. Associations between binge eating , depressive symptoms and anxiety and weight regain after Roux - en - Y gastric bypass surgery. Eat Weight Disord - Stud Anorexia, Bulim Obes. 2020;(0123456789).
Ivezaj V, Barnes RD, Cooper Z, Grilo CM. Loss-of-control eating after bariatric/sleeve gastrectomy surgery: similar to binge-eating disorder despite differences in quantities. Gen Hosp Psychiatry. 2018;54(July):25–30. https://doi.org/10.1016/j.genhosppsych.2018.07.002.
Andrea AP, Ana BG. The utility of DSM-5 indicators of loss of control eating for the bariatric surgery population. 2020;(September 2019):1–10.
Goldschmidt AB. Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obes Rev. 2017;18(4):412–49. https://doi.org/10.1111/obr.12491.
Gradaschi R, Molinari V, Giuseppe S, Paola S, Gian DN, Adami F, et al. Disordered eating and weight loss after bariatric surgery. Eat Weight Disord - Stud Anorexia, Bulim Obes. 2019;(0123456789).
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric Surgery. Am Med Assoc. 2004;292(14):1724–37. https://doi.org/10.1001/jama.292.14.1724.
Maggard MA, Shugarman LR, Suttorp M, et al. Clinical guidelines meta-analysis : surgical treatment of obesity. Ann Intern Med. 2005;142(7):542–58.
Eldar S, Heneghan HM, Brethauer SA, et al. Bariatric surgery for treatment of obesity. Int J Obes. 2011;35(S3):S16–21.
Fanin A, Benetti A, Ceriani V, et al. Bariatric surgery versus medications in the treatment of type 2 diabetes. Minerva Endocrinol. 2015;40(4):297–306.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval Statement
This study is in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bullet points
• The presence of binge eating symptoms was significantly related to weight gain.
• The presence of binge eating symptoms was related to greater weight gain.
• The longer the time elapsed after bariatric surgery, the greater the weight gain.
• Bariatric surgery promotes permanent changes in the glucose regulation in diabetics.
Rights and permissions
About this article
Cite this article
Fangueiro, F.S., França, C.N., Fernandez, M. et al. Binge Eating After Bariatric Surgery in Patients Assisted by the Reference Service in a Brazilian Hospital and the Correlation with Weight Loss. OBES SURG 31, 3144–3150 (2021). https://doi.org/10.1007/s11695-021-05372-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05372-3