Abstract
Purpose
The effectiveness of the standard biliopancreatic diversion with duodenal switch (BPD/DS) in terms of weight loss has been demonstrated. Increasing the strict alimentary limb length while maintaining the length of the common channel could lead to similar weight loss while reducing side effects.
Materials and Methods
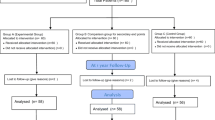
The objective was to evaluate the effect of increasing the strict alimentary limb length on weight loss, comorbidities, nutritional deficiencies, and quality of life 2 years after surgery, compared with standard BPD/DS. An exploratory randomized, double-blind study evaluated the results of LADS at 2 years in comparison with the standard BPD/DS. Common channel was kept at 100 cm in both groups while alimentary limb was created at 100 cm from Treitz angle in the LADS group and at 150 cm total in the BPD/DS group.
Results
Twenty patients were recruited from May 2013 to June 2015. Mean percentage of excess weight loss was statistically significantly lower in the LADS group at 24 months (81.6 ± 6.6% in the LADS group and 97.1 ± 11.1% in the BPD/DS group (p = 0.001). No significant difference regarding the rate of remission of comorbidities was noted. Mean calcium, vitamin D, hemoglobin, zinc, and copper levels were statistically lower in the BPD/DS group. Quality of life was significantly improved in both groups, with no statistically significant difference between the two groups.
Conclusions
At 24 months, weight loss was lower in the LADS group. However, no difference was observed in the improvement in quality of life. LADS technique was discontinued following this study.
Trial registration
ClinicalTrial.gov Ref. NCT03097926





Similar content being viewed by others
Abbreviations
- LADS:
-
Long alimentary limb duodenal switch
- BPD/DS:
-
Biliopancreatic diversion with duodenal switch
- BMI:
-
Body mass index
- EWL:
-
Excess weight loss
- EWL%:
-
Percentage of excess weight loss
- NIH:
-
National Institutes of Health
- SG:
-
Sleeve gastrectomy
- CPAP:
-
Continuous positive airway pressure
- HDL:
-
High-density lipoprotein
- TWL%:
-
Percentage of total weight loss
- SIPS:
-
Stomach intestinal pylorus sparing surgery
- OADS:
-
One-anastomosis duodenal switch
- kg/m2 :
-
Kilogram per meter squared
- kg:
-
Kilogram
- %:
-
Percentage
- N:
-
Number
- CVD:
-
Cardiovascular disease
- T2D:
-
Type 2 diabetes
- COPD:
-
Chronic obstructive pulmonary disease
- HTN:
-
Arterial hypertension
- g/L:
-
Gram per liter
- mM:
-
Millimole
- ng/L:
-
Nanogram per liter
- μM:
-
Micromole
- μg/L:
-
Microgram per liter
- mg:
-
Milligram
- IU:
-
International unit
References
Obesity in Canada - a joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. 2011.
Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr 1992;55(2 Suppl):615S–9S. https://doi.org/10.1093/ajcn/55.2.615s.
Marceau P, Biron S, Fau-Hould F-S, et al. Duodenal switch: long-term results. Obes Surg. 2007;17(11):1421–30.
Anderson B, Gill RS, de Gara CJ, et al. Biliopancreatic diversion: the effectiveness of duodenal switch and its limitations. Gastroenterol Res Pract. 2013;2013:974762. https://doi.org/10.1155/2013/974762.
Homan J, Betzel B, Fau-Aarts EO, et al. Vitamin and mineral deficiencies after biliopancreatic diversion and biliopancreatic diversion with duodenal switch—the rule rather than the exception. Obes Surg. 2015;25(9):1626–32.
Cloutier A, Lebel S, Hould F, et al. Long alimentary limb duodenal switch (LADS): a short-term prospective randomized trial. Surg Obes Relat Dis. 2018;14(1):30–7.
Therrien F, Marceau P, Turgeon N, et al. The Laval questionnaire: a new instrument to measure quality of life in morbid obesity. Health Qual Life Outcomes. 2011;9:66.
Biertho L, Lebel S, Marceau S, et al. Biliopancreatic diversion with duodenal switch: surgical technique and perioperative care. Surg Clin North Am. 2016;96(4):815–26.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Hamoui N, Anthone Gj Fau-Kaufman HS, Kaufman Hs Fau-Crookes PF, et al. Maintenance of weight loss in patients with body mass index >60 kg/m2: importance of length of small bowel bypassed. Surg Obes Relat Dis. 2008;4(3):404–6.
McConnell DB, O’Rourke Rw Fau- Deveney CW, Deveney CW. Common channel length predicts outcomes of biliopancreatic diversion alone and with the duodenal switch surgery. Am J Surg 2005;189(5):536–540.
Cottam A, Cottam D, Portenier D, et al. A matched cohort analysis of stomach intestinal pylorus saving (SIPS) surgery versus biliopancreatic diversion with duodenal switch with two-year follow-up. Obes Surg. 2017;27(2):454–61.
Surve A, Zaveri H, Cottam D, et al. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13(3):415–22.
Sanchez-Pernaute A, Rubio MA, Conde M, et al. Single-anastomosis duodenoileal bypass as a second step after sleeve gastrectomy. Surg Obes Relat Dis. 2015;11(2):351–5.
Shoar S, Poliakin L, Rubenstein R, et al. Single anastomosis duodeno-Ileal switch (SADIS): a systematic review of efficacy and safety. Obes Surg. 2018;28(1):104–13.
Moon RC, Gaskins L, Teixeira AF, et al. Safety and effectiveness of single-anastomosis duodenal switch procedure: 2-year result from a single US institution. Obes Surg. 2018;28(6):1571–7.
Brown WA, Ooi G, Higa K, et al. IFSO-appointed task force reviewing the literature on SADI-S/OADS. Single anastomosis duodenal-Ileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS) IFSO position statement. Obes Surg. 2018;28(5):1207–16.
Moon RC, Kirkpatrick V, Gaskins L, et al. Safety and effectiveness of single- versus double-anastomosis duodenal switch at a single institution. Surg Obes Relat Dis févr. 2019;15(2):245–52.
Finno P, Osorio J, García-Ruiz-de-Gordejuela A, et al. Single versus double-anastomosis duodenal switch: single-site comparative cohort study in 440 consecutive patients. Obes Surg. 2020;30(9):3309–16.
Acknowledgments
The authors thank IUCPQ’s foundation for their support to this work.
Funding
Research grant from the Fondation de l’Institut universitaire de cardiologie et pneumologie de Quebec, Université Laval
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malo, FC., Marion, A., Rioux, A. et al. Long Alimentary Limb Duodenal Switch (LADS): an Exploratory Randomized Trial, Results at 2 Years. OBES SURG 30, 5047–5058 (2020). https://doi.org/10.1007/s11695-020-04968-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04968-5