Abstract
Purpose
The last 5 years have produced a dramatic transformation in the landscape of bariatric and metabolic surgery. Yet, while the landscape of bariatric procedures is changing, little is known about these trends or which factors are responsible for their evolution.
Methods
All primary elective laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG) cases were extracted from the comprehensive Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) data registry from 2015 to 2018.
Results
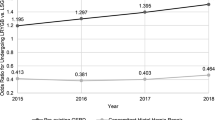
A total of 590,971 patients were identified, with 79.6% being female. Overall, 73.4% of patients underwent LSG. The mean age was 44.5 ± 12.0 years and mean BMI was 45.3 ± 7.9 kg/m2. An increase in proportion of LSG cases was observed and associated with a decrease in LRYGB cases from 2015 to 2018. Multivariable analysis identified dialysis dependence as the greatest predictor of LSG (OR 2.67; 95% CI 2.34–3.04), whereas insulin-dependent diabetes (OR 2.27; 95% CI 2.23–2.32) and gastroesophageal reflux disease (OR 1.52; 95% CI 1.51–1.55) were the two greatest predictors of LRYGB, respectively. Patients offered LSG in 2018 had a near 1.3-fold increase in odds of receiving sleeve gastrectomy vs. those offered surgery in 2015.
Conclusion
The overall numbers of bariatric cases have increased from 2015 to 2018 and are associated with an increase in proportion of LSG cases and a decrease in proportion of LRYGB cases over time. Factors other than patient comorbidities alone are responsible for the current trends and modern landscape of bariatric surgery.

Similar content being viewed by others
References
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288–298. https://doi.org/10.1038/s41574-019-0176-8
World Health Organization. Obesity and overweight: key facts. 2020. Retrieved from https://www.who.int/en/news-room/factsheets/detail/obesity-and-overweight. Accessed 29 Feb 2020.
Morgan DJR, Ho KM, Armstrong J, et al. Long-term clinical outcomes and health care utilization after bariatric surgery: a population-based study. Ann Surg. 2015;262(1):86–92. https://doi.org/10.1097/SLA.0000000000000972.
Pollard S. The current status of bariatric surgery. Frontline Gastroenterol. 2011;2(2):90–5. https://doi.org/10.1136/fg.2010.002626.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes-5-year outcomes. N Engl J Med. 2017;376(7):641–51. https://doi.org/10.1056/NEJMoa1600869.
Padwal R, Klarenbach S, Wiebe N, et al. Bariatric surgery : a systematic review of the clinical and economic evidence. 2011;1183–1194. https://doi.org/10.1007/s11606-011-1721-x.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity. Jama. 2018;319(3):255–65. https://doi.org/10.1001/jama.2017.20897.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. Jama. 2018;319(3):241–54. https://doi.org/10.1001/jama.2017.20313.
Lee W-J, Chong K, Ser K-H, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8. https://doi.org/10.1001/archsurg.2010.326.
Palmieri LJ, Rainteau D, Sokol H, et al. Inhibitory effect of ursodeoxycholic acid on clostridium difficilegermination is insufficient to prevent colitis: a study in hamsters and humans. Front Microbiol. 2018;9(NOV):2849. https://doi.org/10.3389/fmicb.2018.02849.
Chang SH, Freeman NLB, Lee JA, et al. Early major complications after bariatric surgery in the USA, 2003–2014: a systematic review and meta-analysis. Obes Rev. 2018;19(4):529–37. https://doi.org/10.1111/obr.12647.
DeMaria EJ, Pate V, Warthen M, et al. Baseline data from American society for metabolic and bariatric surgery-designated bariatric surgery centers of excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2010;6(4):347–55. https://doi.org/10.1016/j.soard.2009.11.015.
Kumar SB, Hamilton BC, Wood SG, et al. Is laparoscopic sleeve gastrectomy safer than laparoscopic gastric bypass? A comparison of 30-day complications using the MBSAQIP data registry. Surg Obes Relat Dis. 2018;14(3):264–9. https://doi.org/10.1016/j.soard.2017.12.011.
Pucci A, Batterham RL. Mechanisms underlying the weight loss effects of RYGB and SG: similar, yet different. J Endocrinol Investig. 2018;42:117–28. https://doi.org/10.1007/s40618-018-0892-2.
Alizadeh RF, Li S, Inaba C, et al. Risk factors for gastrointestinal leak after bariatric surgery: MBASQIP analysis. J Am Coll Surg. 2018;227(1):135–41. https://doi.org/10.1016/j.jamcollsurg.2018.03.030.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. Jama. 2018;319(3):255–65. https://doi.org/10.1001/jama.2017.20897.
Hoyuela C. Five-year outcomes of laparoscopic sleeve gastrectomy as a primary procedure for morbid obesity: a prospective study. World J Gastrointest Surg. 2017;9(4):109–117. https://doi.org/10.4240/wjgs.v9.i4.109.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27(9):2279–2289. https://doi.org/10.1007/s11695-017-2666-x.
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003−2008. J Am Coll Surg. 2011;213(2):261–6. https://doi.org/10.1016/j.jamcollsurg.2011.04.030.
Henkel DS, Mora-Pinzon M, Remington PL, et al. Trends in the prevalence of severe obesity and bariatric surgery access: a state-level analysis from 2011 to 2014. J Laparoendosc Adv Surg Tech A. 2017;27(7):669–75. https://doi.org/10.1089/lap.2017.0157.
Nguyen NT, Nguyen B, Gebhart A, et al. Changes in the makeup of bariatric surgery : a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216(2):252–7. https://doi.org/10.1016/j.jamcollsurg.2012.10.003.
Khan S, Rock K, Baskara A, et al. Trends in bariatric surgery from 2008 to 2012. Am J Surg. 2016;211(6):1041–6. https://doi.org/10.1016/j.amjsurg.2015.10.012.
Lee Y, Doumouras AG, Yu J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis of weight loss, comorbidities, and biochemical outcomes from randomized controlled trials. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003671.
Kizy S, Jahansouz C, Downey MC, Hevelone N, Ikramuddin S, Leslie D. National trends in bariatric surgery 2012–2015: demographics, procedure selection, readmissions, and cost. 2017;27(11):2933–2939. https://doi.org/10.1007/s11695-017-2719-1.
Santry HP, Lauderdale DS, Cagney K, et al. Predictors of patient selection in bariatric surgery. Ann Surg. 2007;245(1):59–67. https://doi.org/10.1097/01.sla.0000232551.55712.b3.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244(5):741–749. https://doi.org/10.1097/01.sla.0000224726.61448.1b.
Huang R, Sc M, Ding X, et al. Potential mechanisms of sleeve gastrectomy for reducing weight and improving metabolism in patients with obesity. Surg Obes Relat Dis. 2019;15(10):1861–71. https://doi.org/10.1016/j.soard.2019.06.022.
Butterworth J, Deguara J, Borg C-M. Bariatric surgery, polycystic ovary syndrome, and infertility. J Obes. 2016;2016:1871594–6. https://doi.org/10.1155/2016/1871594.
Acknowledgments
The authors would like to thank the Center for the Advancement of Minimally Invasive Surgery (CAMIS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. As this was a retrospective study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mocanu, V., Dang, J.T., Sun, W. et al. An Evaluation of the Modern North American Bariatric Surgery Landscape: Current Trends and Predictors of Procedure Selection. OBES SURG 30, 3064–3072 (2020). https://doi.org/10.1007/s11695-020-04667-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04667-1