Abstract
Background
While laparoscopic sleeve gastrectomy (LSG) continues to be the most commonly performed bariatric operation, several variables influence surgeons’ practice patterns and patients’ decision-making in the type of bariatric procedure to perform. The aim of this study was to evaluate patient factors that influence the decision between laparoscopic Roux-en-Y gastric bypass (LRYGB) versus LSG.
Methods
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database was queried for patients undergoing LSG and LRYGB between 2015 and 2017. Univariate analysis and multivariate logistic regression were used to evaluate factors associated with performing LRYGB compared to LSG.
Results
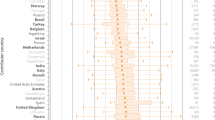
A total of 252,117 (72.3%) LSG and 96,677 (27.7%) LRYGB cases were identified. Patients undergoing LSG were younger (44.3 ± 12.0 vs 45.2 ± 11.8 years; p < 0.01) and had a lower body mass index (BMI; 45.1 ± 7.8 vs 46.2 ± 8.1 kg/m2; p < 0.01). Most of the patients were females (79.4%), white (73.0%), with an American Society of Anesthesiology (ASA) class ≤ 3 (96.4%). The factors associated with undergoing LRYGB compared to LSG were diabetes mellitus, gastroesophageal reflux disease, BMI ≥ 50 kg/m2, ASA class > 3, obstructive sleep apnea, hypertension, and hyperlipidemia. However, patients with kidney disease, black race, chronic steroid use, age ≥ 60 years, recent smoking history, chronic obstructive pulmonary disease, and coronary artery disease were more likely to undergo LSG.
Conclusions
The decision to perform LRYGB is primarily driven by obesity-associated comorbidities and higher BMI, whereas LSG is more likely to be performed in higher risk patients.

Similar content being viewed by others
References
English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, Brethauer SA, Morton JM (2020) American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 16:457–463. https://doi.org/10.1016/j.soard.2019.12.022
El Chaar M, Lundberg P, Stoltzfus J (2018) Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass : first report based on Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis 14:545–553. https://doi.org/10.1016/j.soard.2018.01.011
Osland E, Yunus RM, Khan S, Alodat T, Memon B, Memon MA (2016) Postoperative early major and minor complications in laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a meta-Analysis and systematic review. Obes Surg 26:2273–2284. https://doi.org/10.1007/s11695-016-2101-8
Peterli R, Wolnerhanssen BK, Peters T, Vetter D, Kroll D, Borbely Y, Schultes B, Beglinger C, Drewe J, Schiesser M, Nett P, Bueter M (2018) Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity: The SM-BOSS Randomized Clinical Trial. JAMA 319:255–265. https://doi.org/10.1001/jama.2017.20897
Salminen P, Helmiö M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, Hurme S, Soinio M, Nuutila P, Victorzon M (2018) Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss at 5 Years Among Patients With Morbid Obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA. https://doi.org/10.1001/jama.2017.20313
Shoar S, Saber AA (2017) Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis 13:170–180. https://doi.org/10.1016/j.soard.2016.08.011
Udelsman BV, Jin G, Chang DC, Hutter MM, Witkowski ER (2019) Surgeon factors are strongly correlated with who receives a sleeve gastrectomy versus a Roux-en-Y gastric bypass. Surg Obes Relat Dis 15:856–863. https://doi.org/10.1016/j.soard.2019.03.040
Kallies KJ, Ramirez LD, Grover BT, Kothari SN (2018) Roux-en-Y gastric bypass versus sleeve gastrectomy: what factors influence patient preference? Surg Obes Relat Dis 14:1843–1849. https://doi.org/10.1016/j.soard.2018.08.015
Opozda M, Wittert G, Chur-Hansen A (2017) Patients’ reasons for and against undergoing Roux-en-Y gastric bypass, adjustable gastric banding, and vertical sleeve gastrectomy. Surg Obes Relat Dis 13:1887–1898. https://doi.org/10.1016/j.soard.2017.07.013
(2018) MBSAQIP: User Guide for the 2017 Participant Use Data File (PUF). 1–20
Westerveld D, Yang D (2016) Through Thick and Thin: Identifying Barriers to Bariatric Surgery, Weight Loss Maintenance, and Tailoring Obesity Treatment for the Future. Surg Res Pract 2016:8616581. https://doi.org/10.1155/2016/8616581
Funk LM, Jolles S, Fischer LE, Voils CI (2015) Patient and Referring Practitioner Characteristics Associated With the Likelihood of Undergoing Bariatric Surgery: A Systematic Review. JAMA Surg 150:999–1005. https://doi.org/10.1001/jamasurg.2015.1250
Chawla AS, Hsiao C-W, Romney MC, Cohen R, Rubino F, Schauer P, Cremieux P (2015) Gap Between Evidence and Patient Access: Policy Implications for Bariatric and Metabolic Surgery in the Treatment of Obesity and its Complications. Pharmacoeconomics 33:629–641. https://doi.org/10.1007/s40273-015-0302-y
Coulman KD, Howes N, Hopkins J, Whale K, Chalmers K, Brookes S, Nicholson A, Savovic J, Ferguson Y, Owen-Smith A, Blazeby J, Blazeby J, Welbourn R, Byrne J, Donovan J, Reeves BC, Wordsworth S, Andrews R, Thompson JL, Mazza G, Rogers CA (2016) A Comparison of Health Professionals’ and Patients’ Views of the Importance of Outcomes of Bariatric Surgery. Obes Surg 26:2738–2746. https://doi.org/10.1007/s11695-016-2186-0
Wee CC, Jones DB, Davis RB, Bourland AC, Hamel MB (2006) Understanding patients’ value of weight loss and expectations for bariatric surgery. Obes Surg 16:496–500. https://doi.org/10.1381/096089206776327260
Rozier MD, Ghaferi AA, Rose A, Simon N-J, Birkmeyer N, Prosser LA (2019) Patient Preferences for Bariatric Surgery: Findings From a Survey Using Discrete Choice Experiment Methodology. JAMA Surg 154:e184375. https://doi.org/10.1001/jamasurg.2018.4375
Bachler T, le Roux CW, Bueter M (2016) How do patients’ clinical phenotype and the physiological mechanisms of the operations impact the choice of bariatric procedure? Clin Exp Gastroenterol 9:181–189. https://doi.org/10.2147/CEG.S87205
Zhang Y, Zhao H, Cao Z, Sun X, Zhang C, Cai W, Liu R, Hu S, Qin M (2014) A Randomized Clinical Trial of Laparoscopic Roux-en-Y Gastric Bypass and Sleeve Gastrectomy for the Treatment of Morbid Obesity in China : a 5-Year Outcome. Obes Surg 24:1617–1624. https://doi.org/10.1007/s11695-014-1258-2
Jimenez A, Casamitjana R, Flores L, Viaplana J, Corcelles R, Lacy A, Vidal J (2012) Long-Term Effects of Sleeve Gastrectomy and Roux-en-Y Gastric Bypass Surgery on Type 2 Diabetes Mellitus in Morbidly Obese Subjects. Ann Surg 256:1023–1029. https://doi.org/10.1097/SLA.0b013e318262ee6b
Abbatini F, Rizzello M, Casella G, Alessandri G, Capoccia D, Leonetti F, Basso N (2010) Long-term effects of laparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes. Surg Endosc 24:1005–1010. https://doi.org/10.1007/s00464-009-0715-9
Boza C, Gamboa C, Salinas J, Achurra P, Vega A, Pérez G (2012) Laparoscopic Roux-en- Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis 8:243–249. https://doi.org/10.1016/j.soard.2011.08.023
Yip S, Plank LD, Murphy R (2013) Gastric Bypass and Sleeve Gastrectomy for Type 2 Diabetes : A Systematic Review and Meta-analysis of Outcomes. Obes Surg 23:1994–2003. https://doi.org/10.1007/s11695-013-1030-z
Salminen P, Helmiö M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, Hurme S, Soinio M, Nuutila P, Victorzon M (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity The SLEEVEPASS Randomized Clinical Trial. JAMA - J Am Med Assoc 319:241–254. https://doi.org/10.1001/jama.2017.20313
Wallenius V, Dirinck E, Fändriks L, Maleckas A, le Roux CW, Thorell A (2018) Glycemic Control after Sleeve Gastrectomy and Roux-En-Y Gastric Bypass in Obese Subjects with Type 2 Diabetes Mellitus. Obes Surg 28:1461–1472
Peterli R, Wölnerhanssen BK, Vetter D, Nett P, Gass M, Borbély Y, Peters T, Schiesser M, Schultes B, Beglinger C, Drewe J, Bueter M (2017) Laparoscopic sleeve gastrectomy versus Roux-Y-Gastric bypass for morbid obesity - 3-year outcomes of the prospective randomized Swiss Multicenter Bypass Or Sleeve Study (SM-BOSS). Ann Surg 265:466–473. https://doi.org/10.1097/SLA.0000000000001929
Li J, Lai D, Wu D (2016) Laparoscopic Roux-en-Y Gastric Bypass Versus Laparoscopic Sleeve Gastrectomy to Treat Morbid Obesity-Related Comorbidities : a Systematic Review and Meta-analysis. Obes Surg 26:429–442. https://doi.org/10.1007/s11695-015-1996-9
Jiménez A, Ibarzabal A, Moizé V, Pané A, Andreu A, Molero J, De HA, Flores L, Ortega E, Lacy A, Vidal J (2019) Ten-year outcomes after Roux-en-Y gastric bypass and sleeve gastrectomy : an observational nonrandomized cohort study ✩. Surg Obes Relat Dis 15:382–388. https://doi.org/10.1016/j.soard.2019.01.020
Ahmed B, King WC, Gourash W, Belle SH, Hinerman A, Pomp A, Dakin G, Courcoulas AP (2018) Long-term weight change and health outcomes for sleeve gastrectomy (SG) and matched Roux-en-Y gastric bypass (RYGB) participants in the Longitudinal Assessment of Bariatric Surgery (LABS) Study. Surgery 164:774–783. https://doi.org/10.1016/j.surg.2018.06.008
Hong J, Park S, Lo ME, Rosenthal R (2018) Midterm outcomes of laparoscopic sleeve gastrectomy as a stand-alone procedure in super-obese patients. Surg Obes Relat Dis 14:297–303. https://doi.org/10.1016/j.soard.2017.11.021
Celio AC, Wu Q, Kasten KR, Manwaring ML, Pories WJ, Spaniolas K (2017) Comparative effectiveness of Roux-en-Y gastric bypass and sleeve gastrectomy in super obese patients. Surg Endosc 31:317–323. https://doi.org/10.1007/s00464-016-4974-y
Sheppard CE, Sadowski DC, de Gara CJ, Karmali S, Birch DW (2015) Rates of Reflux Before and After Laparoscopic Sleeve Gastrectomy for Severe Obesity. Obes Surg 25:763–768. https://doi.org/10.1007/s11695-014-1480-y
Mahawar KK, Jennings N, Balupuri S, Small PK (2013) Sleeve gastrectomy and gastro-oesophageal reflux disease: A complex relationship. Obes Surg 23:987–991. https://doi.org/10.1007/s11695-013-0899-x
Coupaye M, Gorbatchef C, Calabrese D, Sami O, Msika S, Coffin B, Ledoux S (2018) Gastroesophageal Reflux After Sleeve Gastrectomy: a Prospective Mechanistic Study. Obes Surg 28:838–845. https://doi.org/10.1007/s11695-017-2942-9
Munie S, Nasser H, Gould JC (2019) Salvage Options for Fundoplication Failure. Curr Gastroenterol Rep 21:41
Mandeville Y, Van Looveren R, Vancoillie PJ, Verbeke X, Vandendriessche K, Vuylsteke P, Pattyn P, Smet B (2017) Moderating the Enthusiasm of Sleeve Gastrectomy: Up to Fifty Percent of Reflux Symptoms After Ten Years in a Consecutive Series of One Hundred Laparoscopic Sleeve Gastrectomies. Obes Surg 27:1797–1803. https://doi.org/10.1007/s11695-017-2567-z
Genco A, Soricelli E, Casella G, Maselli R, Castagneto-Gissey L, Di Lorenzo N, Basso N (2017) Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis 13:568–574
Rebecchi F, Allaix ME, Giaccone C, Ugliono E, Scozzari G, Morino M (2014) Gastroesophageal reflux disease and laparoscopic sleeve gastrectomy: A physiopathologic evaluation. Ann Surg 260:909–915. https://doi.org/10.1097/SLA.0000000000000967
Patti MG, Shlottmann F (2018) Gastroesophageal Reflux After Sleeve Gastrectomy. JAMA Surg 153:1147–1148. https://doi.org/10.1097/SLA
Koh CY, Inaba CS, Sujatha-bhaskar S, Nguyen NT (2018) Outcomes of Laparoscopic Bariatric Surgery in the Elderly Population. Am Surg 84:1600–1603
Sadhasivam S, Larson CJ, Lambert PJ, Mathiason MA, Kothari SN (2007) Refusals, denials, and patient choice: reasons prospective patients do not undergo bariatric surgery. Surg Obes Relat Dis 3:531–536. https://doi.org/10.1016/j.soard.2007.07.004
Martin M, Beekley A, Kjorstad R, Sebesta J (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis 6:8–15. https://doi.org/10.1016/j.soard.2009.07.003
Santry HP, Lauderdale DS, Cagney KA, Rathouz PJ, Alverdy JC, Chin MH (2007) Predictors of patient selection in bariatric surgery. Ann Surg 245:59–67. https://doi.org/10.1097/01.sla.0000232551.55712.b3
Dallal RM, Bailey L, Guenther L, Curley C, Sergi F (2008) Comparative analysis of short-term outcomes after bariatric surgery between two disparate populations. Surg Obes Relat Dis 4:110–114. https://doi.org/10.1016/j.soard.2007.04.007
Flum DR, Khan TV, Dellinger EP (2007) Toward the rational and equitable use of bariatric surgery. JAMA 298:1442–1444. https://doi.org/10.1001/jama.298.12.1442
(2019) MBSC - Weight the odds (1.0.0) [Mobile application software]. https://appadvice.com/app/mbsc-weigh-the-odds/1261031243
Mazzei M, Zhao H, Edwards MA (2019) Perioperative outcomes of bariatric surgery in the setting of chronic steroid use: an MBSAQIP database analysis. Surg Obes Relat Dis 15:926–934. https://doi.org/10.1016/j.soard.2019.02.007
Di Palma A, Liu B, Maeda A, Anvari M, Jackson T, Okrainec A (2020) Marginal ulceration following Roux-en-Y gastric bypass: risk factors for ulcer development, recurrence and need for revisional surgery. Surg Endosc. https://doi.org/10.1007/s00464-020-07650-0
King WC, White GE, Belle SH, Yanovski SZ, Pomp A, Pories WJ, Wolfe BM, Ahmed B, Courcoulas AP (2020) Changes in Smoking Behavior Before and After Gastric Bypass: A 7-year Study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003828
Gesquiere I, Lannoo M, Augustijns P, Matthys C, Van der Schueren B, Foulon V (2014) Iron deficiency after Roux-en-Y gastric bypass: insufficient iron absorption from oral iron supplements. Obes Surg 24:56–61. https://doi.org/10.1007/s11695-013-1042-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Arthur M. Carlin receives an honorarium from Blue Cross Blue Shield of Michigan as Executive Committee Chair of the Michigan Bariatric Surgery Collaborative. Dr. Hassan Nasser and Dr. Tommy Ivanics have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nasser, H., Ivanics, T. & Carlin, A.M. Factors influencing the choice between laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Endosc 35, 4691–4699 (2021). https://doi.org/10.1007/s00464-020-07933-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07933-6