Abstract
Background
Bariatric surgery for severe obesity can lead to micronutrient/vitamin deficiencies.
Aims
To study baseline and post-surgical prevalence of vitamin D deficiency in patients undergoing bariatric surgery.
Participants and Setting
Patients undergoing bariatric surgery in a university teaching hospital in North West England.
Methods
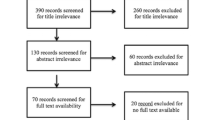
We performed an observational cohort analysis of longitudinal data on vitamin D and related parameters in patients who underwent bariatric surgery. Patients were routinely recommended daily combined calcium and vitamin D supplementation post-surgery.
Results
We studied 460 patients who had completed at least 12 months post-operatively; mean (standard deviation) age was 48.0 (10.5) years, weight 144.7 (27.3) kg and body mass index 50.0 (7.6) kg/m2; 292 (63.5%) underwent gastric bypass and 168 (36.5%) sleeve gastrectomy. Vitamin D level was 33.1 (23.9) nmol/L at baseline, rising to 57.1 (23.1) nmol/L at 12 months post-surgery. Whereas 43.2% had vitamin D deficiency and 34.7% insufficiency preoperatively, 8.9% and 26.7% had deficiency and insufficiency, respectively, at 12 months with similar trends up to 4 years of follow-up. There were no significant differences between procedures or sexes in vitamin D levels or sufficiency rates.
Conclusion
Vitamin D deficiency and insufficiency were prevalent pre-surgery and reduced significantly with routine supplementation post-surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a major public health concern of our times. Whilst lifestyle, dietary and behavioural changes and weight loss pharmacotherapy remain key interventions, bariatric surgery is the most effective treatment for severe obesity. It has been demonstrated that it leads to clinically significant weight loss and is cost-effective [1,2,3,4]. Post-bariatric surgery, patients typically achieve substantial weight loss and significant improvement or resolution of weight-related comorbidities including type 2 diabetes mellitus (T2DM), hypertension and hyperlipidaemia. A recent meta-analysis of observational data reported that patients who underwent bariatric surgery had 50% lower mortality than controls over follow-up of 2 to 15 years [5]. Thus, bariatric surgery is widely recommended as a treatment for severe obesity [6].
Bariatric procedures are associated with various micronutrient deficiencies including vitamin D deficiency [7,8,9,10,11]. Vitamin D is important for calcium homeostasis and bone metabolism. There are concerns that bone health may be adversely affected by bariatric surgery, and that vitamin D deficiency may play a part [12,13,14,15,16,17,18]. One meta-analysis of 51 studies found mean vitamin D levels ≤ 20 ng/mL (50 nmol/L) in a third of studies [10]; mean vitamin D levels remained ≤ 30 ng/mL (75 nmol/L) following bariatric surgery despite various vitamin D replacement regimens, with few exceptions. Another meta-analysis of 12 studies found that a daily vitamin D supplement of > 800 IU (but not < 800 IU) significantly reduced the prevalence of post-operative vitamin D depletion at 1 year [19]. Our centre recommends that patients take ≥ 800 IU vitamin D along with 1000–1200 mg calcium daily consistent with the British Obesity & Metabolic Surgery Society guideline [8]. Patients are encouraged to attend follow-up appointments for life-long monitoring, and supplement doses are adjusted according to requirements.
Gap in Knowledge
Vitamin D levels in the general population fluctuate through the year depending on levels of exposure to ultraviolet B radiation from sunlight, the major source of vitamin D synthesis for most people, and are frequently diminished in northern latitudes [20]. There is little known of prevalence of vitamin D insufficiency/deficiency in bariatric surgical candidates in North West England (54° N) and whether the usually recommended vitamin D supplementation is adequate following bariatric surgery. We report a longitudinal cohort analysis of vitamin D and associated outcomes of bariatric surgery over 4 years of follow-up.
Methods
We performed an observational cohort analysis of prospectively recorded longitudinal data on vitamin D and related parameters in patients who underwent bariatric surgery.
Patients and Setting
We studied patients who had undergone primary bariatric surgery over a 4-year follow-up period at a university teaching hospital in the North West of England, UK. Permission was obtained from the Clinical Audit department of our institution. Patient selection for primary bariatric surgery was in accordance with the National Institute for Health and Care Excellence (NICE) clinical guideline and the National Health Service (NHS) clinical commissioning policy for complex and severe obesity [6, 21]. Patients who had undergone gastric bypass or sleeve gastrectomy were included; other primary bariatric surgeries, such as gastric banding, and revisional procedures were excluded. Patients who were undergoing another surgical procedure at the same time as gastric bypass or sleeve gastrectomy (e.g. laparoscopic cholecystectomy or hernia repair along with primary bariatric surgery) were not excluded.
A total of 460 patients who underwent primary bariatric surgery between March 2012–March 2016 were included, and data were extracted from electronic patient records in April 2017 such that all patients had completed a minimum of 12 months post-operatively; the number of patients who had completed 24, 36 and 48 months post-operatively was 362, 253 and 149, respectively. Data collected included patient demographics, preoperative baseline data and post-operative follow-up data, including weight, height, body mass index (BMI; kg/m2) and percent total weight loss (%TWL); and blood tests including total vitamin D (25-hydroxyvitamin D, 25(OH)D), phosphate, alkaline phosphatase (ALP), parathyroid hormone (PTH), albumin and total calcium. The laboratory recommended reference ranges for the time period of study were used [22]. The calcium level was adjusted for serum albumin < 40 g/L by applying the formula, adjusted calcium (mmol/L) = total calcium (mmol/L) + 0.02*[40 – albumin (g/L)] [23]. Vitamin D levels were categorised using the thresholds recommended by the National Osteoporosis Society as deficient (25(OH)D < 25 nmol/L), insufficient (25–50 nmol/L) or sufficient (> 50 nmol/L) [24]. Glycated haemoglobin (HbA1c) was also recorded as a metabolic disease measure.
Statistical Analysis
We performed descriptive statistics of demographic characteristics with parametric tests (or non-parametric tests for non-normative data), with measures of dispersion as appropriate. Comparative analyses were performed with independent or paired samples t tests as appropriate. The Fisher exact test was used to analyse contingency tables of categorical variables. Linear associations were analysed with the Pearson correlation formula. A two-sided P < 0.05 was considered statistically significant. To cope with missing values because of the retrospective, observational nature of the study, frequencies were reported as valid percentages and significant results were confirmed by reanalysing data after multiple imputation by fully conditional specification method [25]. Results were reported based on original, unimputed data. Data were analysed using IBM SPSS Statistics 23.0 (IBM Corp, Armonk, NY) and GraphPad Prism 7.0 (GraphPad Software, La Jolla, CA).
Results
We studied longitudinal vitamin D status in patients who underwent primary bariatric surgery.
Patient Demographics
The 460 patients comprised 299 women (65%) and 161 men (35%). The mean (standard deviation; SD) age at time of surgery was 48.0 (10.5) years. Baseline weight was 144.7 (27.3) kg and BMI 50.0 (7.6) kg/m2. Gastric bypass was the most frequent operation (292, 63.5%), followed by sleeve gastrectomy (168, 36.5%).
Weight Loss (and Metabolic) Outcomes
Following bariatric surgery there was significant weight loss, with mean (SD) reduction in BMI of 14.7 (4.8) kg/m2 (P < 0.001) at 12 months (Table 1). The weight loss was sustained over 4 years of follow-up, with a non-significant (ns) rise in BMI from 35.1 (6.6) kg/m2 at 12 months to 37.2 (7.2) kg/m2 at 48 months. The weight loss equated to %TWL of 31.4 (8.1) % at 12 months (Fig. 1a). The %TWL for gastric bypass vs. sleeve gastrectomy was 32.6% vs. 29.4% (P < 0.001) at 12 months, 35.5% vs. 29.1% (P < 0.001) at 24 months, 33.5% vs. 27.0% (P < 0.006) at 36 months and 30.8% vs. 25.8% (ns) at 48 months. There were no consistent significant differences in weight loss between men and women or people with or without diabetes.
Out of 189 people with pre-existing T2DM, 180 had baseline HbA1c recorded; of these, 69.4% had HbA1c ≥ 48 mmol/mol prior to surgery, but by 4 months, this prevalence had fallen to 23.3% (P < 0.001). At baseline, the mean HbA1c in the gastric bypass group (n = 129) vs. sleeve gastrectomy group (n = 51) was 63.0 vs. 58.2 mmol/mol (ns). At baseline, the mean HbA1c in women (n = 98) vs. men (n = 82) was 60.9 vs. 62.5 mmol/mol (ns). Post-operative reductions in HbA1c were similar with no significant difference between surgical or sex groups.
Vitamin D, Parathyroid Hormone and Calcium
Preoperatively, mean (SD) vitamin D level was 33.1 (23.9) nmol/L (Fig. 1b ); post-operatively, the vitamin D level increased to 57.4 (27.4) nmol/L at 4 months (P < 0.001) and was maintained at subsequent timepoints. There was no significant difference in vitamin D levels between gastric bypass and sleeve gastrectomy throughout the period of study. There was no significant change in mean parathyroid hormone levels overall or by type of surgery throughout (Fig. 1 c). Mean adjusted calcium levels reduced significantly by 12 months post-surgery and beyond compared to baseline (Fig. 1d ).
At baseline, there was a significant inverse correlation between BMI and vitamin D level (r = − 0.270, P < 0.001) (Fig. 2 a). This inverse correlation became weaker with significant weight loss at 12 months (r = − 0.130, P < 0.02) and thereafter. This was corroborated by a significant positive correlation between %TWL and vitamin D level, i.e. the greater the excess weight loss, the higher the vitamin D level. At 4 months, a significant positive correlation between %TWL and vitamin D was demonstrated (r = 0.142, P < 0.034). This was also seen at 12 months (r = 0.113, P < 0.049) and 24 months (r = 0.185, P < 0.019) but not thereafter. However, at no timepoints was there a significant correlation between %TWL and change in vitamin D level from baseline.
At baseline, there was an inverse correlation between vitamin D and PTH levels (r = − 0.204, P < 0.001) (Fig. 2b ). A similar strength of correlation was seen at all timepoints from 4 to 48 months post-bariatric surgery. There was positive correlation between vitamin D and adjusted calcium levels at baseline (r = 0.144, P = 0.013) (Fig. 2 c), and at 12 months post-bariatric surgery (r = 0.161, P < 0.004) but not thereafter. PTH and adjusted calcium levels were inversely correlated at baseline (r = − 0.142, P = 0.012) (Fig. 2d ), and at 12 months post-bariatric surgery (r = − 0.160, P < 0.003).
At baseline, 43.2% of all patients had vitamin D deficiency and 34.7% had insufficiency; rates of vitamin D sufficiency increased significantly at all post-operative timepoints, with no significant differences between procedures or sexes (Fig. 3 a). Patients with high PTH or low adjusted calcium levels had higher rates of vitamin D insufficiency/deficiency (Fig. 3b ).
Vitamin D status: proportions of patients with vitamin D sufficiency (> 50 nmol/L; bottom stack, black), insufficiency (25–50 nmol/L; middle stack, light grey) or deficiency (< 25 nmol/L; top stack, dark grey); a in each set, the first column depicts all patients, second column gastric bypass, third sleeve gastrectomy, fourth men and fifth women; b in each set, the first column depicts all patients, second column patients with normal PTH, third patients with normal adjusted calcium, fourth patients with high PTH and fifth patients with low adjusted calcium levels
At baseline, 23.8% of all patients had raised PTH levels; rates of hyperparathyroidism increased over time but there were no significant differences between procedures or sexes (Fig. 4a ). Among patients with vitamin D sufficiency, 20.0% had raised parathyroid hormone levels at baseline and hyperparathyroidism persisted at rates of 15–30% throughout the 4 years of follow-up (non-significant change compared to baseline at all timepoints), whilst patients with vitamin D insufficiency/deficiency or hypocalcaemia had higher rates of hyperparathyroidism (Fig. 4b ).
Parathyroid hormone (PTH) status: proportions of patients with normal PTH (bottom stack; black) or high PTH (top stack; light grey); a in each set, the first column depicts all patients, second column gastric bypass, third sleeve gastrectomy, fourth men and fifth women; b in each set, the first column depicts all patients, second column patients with vitamin D sufficiency (> 50 nmol/L), third patients with normal adjusted calcium, fourth patients with vitamin D insufficiency/deficiency (≤ 50 nmol/L) and fifth patients with low adjusted calcium levels
At baseline, 8.5% of all patients had low adjusted calcium levels; rates of hypocalcaemia increased over time, with no significant differences between procedures or sexes (Fig. 5 a). Patients with hyperparathyroidism or vitamin D insufficiency/deficiency had higher rates of hypocalcaemia (Fig. 5b ).
Calcium status: proportions of patients with normal adjusted calcium (bottom stack, black) or low adjusted calcium (top stack, light grey); a in each set, the first column depicts all patients, second column gastric bypass, third sleeve gastrectomy, fourth men and fifth women; b in each set, the first column depicts all patients, second column patients with normal PTH, third patients with vitamin D sufficiency (> 50 nmol/L), fourth patients with high PTH and fifth patients with vitamin D insufficiency/deficiency (≤ 50 nmol/L)
Discussion
We assessed longitudinal vitamin D status in patients undergoing bariatric surgery. The pre-operative mean vitamin D level of 33 nmol/L, with over two-fifths of patients having deficiency and a further one-third having insufficiency, was not dissimilar to previous studies [10]. Patients in our centre were routinely advised daily vitamin D supplementation ≥ 800 IU. We observed significant improvement in vitamin D level post-operatively that was maintained over 4 years of follow-up, with no differences between types of surgery. However, some patients remained deficient in vitamin D despite supplementation, consistent with previous research [7, 10, 11, 13, 15, 26,27,28,29]. Previous meta-analyses have reported wide variation in vitamin D supplementation regimens with a proportionate increase in post-operative vitamin D levels [10]; whilst a daily vitamin D supplement of more than 800 IU significantly reduced the prevalence of vitamin D depletion at 12 months, a dosage of less than 800 IU did not [19].
Vitamin D deficiency has a significant background prevalence in the UK, with 17% of adults aged 19–64 having levels lower than 25 nmol/L [30, 31]. Rates of deficiency increase to 30–40% during winter months as most vitamin D is obtained through the action of sunlight on the skin. This is influenced by many factors including, but not limited to, season, use of sunscreen, cloud cover, time spent outside during the optimal latitude of the sun and amount of skin exposure [20]. The reference nutrient intake (RNI) for vitamin D is 10 microgram (400 IU) per day [31]. Dietary sources of vitamin D include oily fish, eggs, meat, fortified cereals and fat spreads, and nutritional supplements. Eating a diet rich in vitamin D will help to prevent deficiency, but data from the national diet and nutrition survey show that adults from the UK aged 19–64 have an average daily intake of 42% of the RNI from diet and supplements [30]. Therefore, the advice for the general population is to routinely take a supplement to ensure healthy vitamin D status, especially during the autumn and winter months [32].
It has been consistently demonstrated that there is a high prevalence of vitamin D deficiency in patients with obesity. One meta-analysis reported vitamin D deficiency to be 35% more prevalent in individuals with obesity than in controls of normal weight, and 24% more than in those who were classed as overweight [29]. Several different reasons have been proposed. Evidence suggests that vitamin D becomes sequestered in adipose tissue in individuals with obesity, contributing to low circulating levels of vitamin D. One study found visceral fat (of which individuals with obesity have a high proportion) to have 21% higher vitamin D levels than subcutaneous fat [33]. Oral vitamin D may also be reduced in individuals with obesity due to low intake of vitamin D-containing foods—termed high-calorie malnutrition. Individuals with obesity may also have less exposure to sunlight due to a relatively sedentary lifestyle, resulting in less vitamin D being produced in the skin. It has also been suggested that obesity-related steatosis of the liver may lead to reduced activation of vitamin D [34]. Recent research has found that the proinflammatory state which comes with obesity may lead to alterations in vitamin D metabolism and lowered circulating levels [35]. Furthermore, chronic kidney disease, which is more prevalent in obese individuals [36], is associated with vitamin D deficiency [37]. Adiposity and BMI have been shown to have a negative correlation with serum vitamin D levels [16, 38,39,40]. Thus, bariatric surgical candidates have a predisposition to vitamin D deficiency. Studies have reported that typically over 50% of bariatric surgical candidates are deficient in vitamin D, and in some cases over 90% [28].
There have been concerns that bariatric surgery may induce or exacerbate vitamin D deficiency. Key reasons for this which have been proposed include reduced oral intake and malabsorptive effects of the procedures. For these reasons, routine supplementation is recommended after bariatric surgery, though there is no consensus on dose or regimen, with doses used in studies ranging from 200 to 28,500 IU daily [10]. In the US, consensus guidelines recommend at least 3000 IU daily [41]. The British Obesity & Metabolic Surgery Society recognises that usual practice following gastric bypass or sleeve gastrectomy is oral supplementation with 20 micrograms (800 IU) vitamin D (commonly as a combined calcium and vitamin D tablet) per day, with higher doses if still deficient [8]. Most studies have reported difficulty in optimisation of vitamin D levels after bariatric surgery, despite varying doses of supplementation. Reasons for this may include malabsorption of supplements, inadequate supplement dose and lack of concordance. Residual excess adiposity may also play a role. Some studies have suggested that vitamin D optimisation is possible in many patients after bariatric surgery. In particular, a rapid rise in vitamin D has been demonstrated in the period immediately after surgery [10, 19]. This may be due to a high level of compliance with supplementation soon after surgery. It has also been suggested that the rapid weight loss following surgery may liberate vitamin D sequestered in visceral fat, augmenting vitamin D levels initially [42].
Previous studies of vitamin D status after bariatric surgery have illustrated marked variation in numerous factors, most notably vitamin D dose and regimen, definition of vitamin D deficiency and length of follow-up. However, some authors have performed systematic reviews and meta-analyses, and have reported a variety of findings [10, 15, 19, 26,27,28, 43, 44]. Most studies have only followed patients for 1 or 2 years post-operatively, limiting their long-term significance. Some have found post-operative supplementation to be ineffective almost universally whilst others have found some regimens to be successful in preventing post-operative vitamin D deficiency in some patients [10, 19, 27, 28, 43, 44]. Many have reported that requirements for vitamin D supplementation vary significantly between patients. It is our policy to screen all bariatric surgical candidates prior to their operation and treat deficiencies. Our centre recommends post-operative maintenance supplementation with 1000–1200 mg of elemental calcium combined with vitamin D > 800 IU daily. We have found that this regimen with subsequent monitoring and dose modification can prevent vitamin D deficiency post-operatively in most patients. We found no significant difference in vitamin D deficiency rates between gastric bypass and sleeve gastrectomy. Secondary hyperparathyroidism was seen in up to two-thirds of patients with vitamin D deficiency. Intriguingly, about one-fifths of patients with vitamin D sufficiency also had raised PTH levels. Despite calcium supplementation and maintenance of normocalcaemia, notably there was a statistically significant fall in mean calcium levels following bariatric surgery by 12 months and beyond. It has been suggested that calcium deficiency seems to play the driving force for secondary hyperparathyroidism in patients with vitamin D sufficiency [14]; serum calcium levels may be maintained within the normal range by bone resorption in these patients. Clinically significant reduction in bone mineral density (BMD) has been reported in three-fifths of patients at 6 months and in seven-tenths at 12 months after bariatric surgery, alongside a significant association with greater weight loss [18]. Individuals with T2DM treated by gastric bypass, compared to individuals with T2DM of similar age and body composition not treated by gastric bypass, have been reported to have lower BMD, lower bone strength, and increased levels of several bone turnover markers [45]. Another recent study has also reported that levels of bone turnover markers increased significantly after gastric bypass surgery [46]. Systematic vitamin D and calcium supplementation seems advisable although its beneficial effect on BMD in the post-surgical population remains to be seen.
Limitations
Despite careful manual collection of data from a prospective electronic database, our study was restricted by the retrospective nature of the cohort analysis. Whilst we did not record racial demographics, we should remark that our catchment population is comprised of mostly White British ethnicity. In common with many longitudinal observational studies, data attrition due to patients being lost to follow-up was a major limitation of this study. Despite a large initial sample size, data for key measurements (such as vitamin D) was unavailable for 30% of completers at 1 year and 60% of completers at 4 years. Whilst multiple imputation by fully conditional specification is deemed a powerful and statistically valid method for handling missing data [25], and significant results were confirmed by this method in our study, we have reported results based on original unimputed data in recognition of the inherent bias of data attrition from “missing not at random”. We were unable to collect data on personalised dose adjustments of supplements and patients’ adherence to treatment, or seasonal variations in vitamin D levels. Although vitamin D, calcium and PTH are useful indicators, we were unable to include markers of bone turnover, bone densitometry or fracture data and so cannot report directly the skeletal effects of bariatric surgery in our cohort. Despite these limitations, our observational study provides useful insights into vitamin D status in bariatric surgical patients in northern latitudes.
Conclusion
We report that vitamin D deficiency was prevalent in bariatric surgical candidates pre-operatively and routine vitamin D supplementation can reduce rates of post-operative vitamin D deficiency in patients undergoing weight loss surgery. However, some patients remain poorly optimised despite this. Further research could investigate risk factors for difficult-to-optimise vitamin D status as well as different supplementation methods and dose regimens.
References
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23163728
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25105982
Welbourn R, le Roux CW, Owen-Smith A, Wordsworth S, Blazeby JM. Why the NHS should do more bariatric surgery; how much should we do? BMJ. 2016;353:i1472. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27169605
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190, 215–357, iii–iv. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19726018
Kwok CS, Pradhan A, Khan MA, Anderson SG, Keavney BD, Myint PK, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173:20–8. Available from: https://doi.org/10.1016/j.ijcard.2014.02.026
Obesity: Identification, Assessment and Management. Clinical Guideline (CG189). London: National Institute for Health and Care Excellence; 2014. Available from: https://www.nice.org.uk/guidance/cg189/resources/obesity-identification-assessment-and-management-pdf-35109821097925
Via MA, Mechanick JI. Nutritional and micronutrient care of bariatric surgery patients: Current Evidence Update. Curr Obes Rep. 2017;6:286–96. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28718091
O’Kane M, Pinkney J, Aasheim ET, Barth JH, Batterham RL, Welbourn R, et al. BOMSS guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery. London: British Obesity & Metabolic Surgery Society; 2014. Available from: http://www.bomss.org.uk/wp-content/uploads/2014/09/BOMSS-guidelines-Final-version1Oct14.pdf
Damms-Machado A, Friedrich A, Kramer KM, et al. Pre- and postoperative nutritional deficiencies in obese patients undergoing laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:881–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22403000
Chakhtoura MT, Nakhoul NN, Shawwa K, Mantzoros C, El Hajj Fuleihan GA. Hypovitaminosis D in bariatric surgery: a systematic review of observational studies. Metabolism. 2016;65:574–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26805016
van der Beek ESJ, Monpellier VM, Eland I, et al. Nutritional deficiencies in gastric bypass patients; incidence, time of occurrence and implications for post-operative surveillance. Obes Surg. 2015;25:818–23. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25330868
Ablett AD, Boyle BR, Avenell A. Fractures in adults after weight loss from bariatric surgery and weight management programs for obesity: systematic review and meta-analysis. Obes Surg. 2019;29:1327–42. Available from:. https://doi.org/10.1007/s11695-018-03685-4.
Wei J-H, Lee W-J, Chong K, et al. High incidence of secondary hyperparathyroidism in bariatric patients: comparing different procedures. Obes Surg. 2018;28:798–804. Available from:. https://doi.org/10.1007/s11695-017-2932-y.
Peters T, Toelle P, Gebhart M, et al. Risk factors for secondary hyperparathyroidism after bariatric surgery. Clin Rev Bone Miner Metab. 2014;12:228–33. Available from:. https://doi.org/10.1007/s12018-014-9173-6.
Liu C, Wu D, Zhang J-F, Xu D, Xu W-F, Chen Y, et al. Changes in bone metabolism in morbidly obese patients after bariatric surgery: a meta-analysis. Obes Surg. 2016;26:91–7. Available from: https://doi.org/10.1007/s11695-015-1724-5
Stein EM, Strain G, Sinha N, Ortiz D, Pomp A, Dakin G, et al. Vitamin D insufficiency prior to bariatric surgery: risk factors and a pilot treatment study. Clin Endocrinol (Oxf). 2009;71:176–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19018785
Santos D, Lopes T, Jesus P, et al. Bone metabolism in adolescents and adults undergoing Roux-en-Y gastric bypass: a comparative study. Obes Surg. 2019;29:2144–50. Available from:. https://doi.org/10.1007/s11695-019-03797-5.
Geoffroy M, Charlot-Lambrecht I, Chrusciel J, Gaubil-Kaladjian I, Diaz-Cives A, Eschard J-P, et al. Impact of bariatric surgery on bone mineral density: observational study of 110 patients followed up in a specialized center for the treatment of obesity in France. Obes Surg. 2019;29:1765–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30734230
Li Z, Zhou X, Fu W. Vitamin D Supplementation for the prevention of vitamin D deficiency after bariatric surgery: a systematic review and meta-analysis. Eur J Clin Nutr. 2018;72:1061–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29288249
Webb AR, Kazantzidis A, Kift RC, Farrar MD, Wilkinson J, Rhodes LE. Meeting vitamin D requirements in White Caucasians at UK latitudes: providing a choice. Nutrients. 2018;10:497. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29673142
NHS Commissioning Board Clinical Reference Group for Severe and Complex Obesity. Clinical commissioning policy: complex and specialised obesity surgery. Leeds: NHS Commissioning Board; 2013. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/05/appndx-6-policy-sev-comp-obesity-pdf.pdf
Pathology at Wigan and Salford (PAWS) Department of Clinical Biochemistry User Guide. Salford: Pathology at Wigan and Salford; 2016 [cited 2019 Apr 27]. Available from: https://www.srft.nhs.uk/EasysiteWeb/getresource.axd?AssetID=2824
O’Kane M, Jassam N, Barth J, Day A, Bowles S, MacKenzie F, et al. Albumin-adjusted calcium: a position paper. London: The Association for Clinical Biochemistry and Laboratory Medicine; 2015. Available from: http://acb.org.uk/docs/default-source/committees/clinical-practice/guidelines/acb-adjusted-calcium-position-paper-march-2015.pdf
Francis R, Aspray T, Fraser W, Macdonald H, Patel S, Mavroeidi A, et al. Vitamin D and bone health: a practical clinical guideline for patient management. Camerton: Royal Osteoporosis Society; 2018. Available from: https://theros.org.uk/healthcare-professionals/tools-and-resources/clinical-guidance/documents/vitamin-d-and-bone-health-in-adults/
Liu Y, De A. Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic study. Int J Stat Med Res. 2015;4:287–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27429686
Switzer NJ, Marcil G, Prasad S, Debru E, Church N, Mitchell P, et al. Long-term hypovitaminosis D and secondary hyperparathyroidism outcomes of the Roux-en-Y gastric bypass: a systematic review. Obes Rev. 2017;18:560–6. Available from: https://doi.org/10.1111/obr.12525
Compher CW, Badellino KO, Boullata JI. Vitamin D and the bariatric surgical patient: a review. Obes Surg. 2008;18:220–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18176832
Peterson LA, Zeng X, Caufield-Noll CP, Schweitzer MA, Magnuson TH, Steele KE. Vitamin D status and supplementation before and after bariatric surgery: a comprehensive literature review. Surg Obes Relat Dis. 2016;12:693–702. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27036669
Pereira-Santos M, Costa PRF, Assis AMO, Santos CAST, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. 2015;16:341–9. Available from: https://doi.org/10.1111/obr.12239
Roberts C, Steer T, Maplethorpe N, Cox L, Meadows S, Nicholson S, et al. National diet and nutrition survey: results from years 7 and 8 (combined) of the rolling programme (2014/2015–2015/2016). London: Public Health England; 2018. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file-/699241/NDNS_results_years_7_and_8.pdf
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O'Karma M, Wallace TC, Zemel BS. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016;27:1281–386. Available from: https://doi.org/10.1007/s00198-015-3440-3
Vitamin D and Health. London: Scientific Advisory Committee on Nutrition; 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/537616/SACN_Vitamin_D_and_Health_report.pdf
Beckman LM, Earthman CP, Thomas W, Compher CW, Muniz J, Horst RL, et al. Serum 25(OH) vitamin D concentration changes after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring). 2013;21:E599-606. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23526677
Pickett-Blakely O, Young K, Carr RM. Micronutrients in nonalcoholic fatty liver disease pathogenesis. Cell Mol Gastroenterol Hepatol. 2018;6:451–62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30294653
Lespessailles E, Toumi H. Vitamin D alteration associated with obesity and bariatric surgery. Exp Biol Med (Maywood). 2017;242:1086–94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28103699
Garofalo C, Borrelli S, Minutolo R, Chiodini P, De Nicola L, Conte G. A systematic review and meta-analysis suggests obesity predicts onset of chronic kidney disease in the general population. Kidney Int. 2017;91:1224–35. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28187985
Jean G, Souberbielle JC, Chazot C. Vitamin D in chronic kidney disease and dialysis patients. Nutrients. 2017;9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28346348
Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe EL, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham heart study. Diabetes. 2010;59:242–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19833894
Coates PS, Fernstrom JD, Fernstrom MH, Schauer PR, Greenspan SL. Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab. 2004;89:1061–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15001587
DiGiorgi M, Daud A, Inabnet WB, Schrope B, Urban-Skuro M, Restuccia N, et al. Markers of bone and calcium metabolism following gastric bypass and laparoscopic adjustable gastric banding. Obes Surg. 2008;18:1144–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18335295
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21 Suppl 1:S1–27. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23529939
Saltzman E, Karl JP. Nutrient deficiencies after gastric bypass surgery. Annu Rev Nutr. 2013;33:183–203. Available from: https://doi.org/10.1146/annurev-nutr-071812-161225
Dewey M, Heuberger R. Vitamin D and calcium status and appropriate recommendations in bariatric surgery patients. Gastroenterol Nurs. 2011;34:367–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21979398
Dix CF, Bauer JD, Wright ORL. A systematic review: Vitamin D status and sleeve Gastrectomy. Obes Surg. 2017;27:215–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27815862
Madsen LR, Espersen R, Ornstrup MJ, Jørgensen NR, Langdahl BL, Richelsen B. Bone health in patients with type 2 diabetes treated by Roux-en-Y gastric bypass and the role of diabetes remission. Obes Surg. 2019;29:1823–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30719648
Svanevik M, Risstad H, Hofsø D, Blom-Høgestøl IK, Kristinsson JA, Sandbu R, et al. Bone turnover markers after standard and distal Roux-en-Y gastric bypass: results from a randomized controlled trial. Obes Surg. 2019; Available from: http://www.ncbi.nlm.nih.gov/pubmed/31065919
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval Statement
For this type of study, formal consent was not required.
Informed Consent Statement
Does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fox, A., Slater, C., Ahmed, B. et al. Vitamin D Status After Gastric Bypass or Sleeve Gastrectomy over 4 Years of Follow-up. OBES SURG 30, 1473–1481 (2020). https://doi.org/10.1007/s11695-019-04318-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04318-0