Abstract
Background
Few investigations have been conducted that compared blood glucose in patients with diabetes mellitus (DM2) and morbid obesity who had undergone laparoscopic sleeve gastrectomy (LSG) or gastric bypass (LRYGB). We aimed to compare the effects of these procedures using continuous glucose monitoring (CGM).
Methods
We prospectively studied patients that had qualified for LSG or LRYGB. The inclusion criteria were DM2 of ≤ 5 years, for which patients were taking oral anti-diabetic drugs, or no glucose metabolism disorder; and morbid obesity. CGM was performed between admission and the 10th postoperative day.
Results
We studied 16 patients with DM2 and 16 without. Eighteen patients underwent LSG and 14 underwent LRYGB. The median hemoglobin A1c was 5.5% (5.4–5.9%) in DM2 patients, which did not differ from control (p = 0.460). Preoperative mean daily glucose concentration was similar between DM2 and control patients (p = 0.622). For patients with DM2, LRYGB was associated with more frequent low glucose status, and these episodes lasted longer than in DM2 patients that underwent LSG (p = 0.035 and 0.049, respectively). DM2 patients that underwent LRYGB demonstrated lower glucose concentrations from third postoperative day than those that underwent LSG. Patients without DM2 did not demonstrate differences in daily mean glucose concentrations, or in incidence nor duration of hypoglycemia throughout the observation period.
Conclusion
A significantly larger reduction in interstitial glucose concentration is present from third day in patients with DM2 who undergo LRYGB vs. LSG, accompanied by a lower incidence and shorter duration of low glucose episodes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improvements in control or complete resolution of obesity-related comorbidities are observed after various types of bariatric surgery. Previously published studies and recommendations have classified these types of surgery according to their effects on metabolism, and have concluded that laparoscopic Roux-en-Y gastric bypass (LRYGB) can be more beneficial than laparoscopic sleeve gastrectomy (LSG) for the treatment of type 2 diabetes mellitus (DM2), remission of other obesity-related comorbidities, and weight loss [1,2,3,4]. However, a literature search revealed that the changes in glucose concentration in patients with DM2 and morbid obesity in the perioperative period had not been thoroughly compared between LSG and LRYGB. Some previous studies have reported comparable efficacy of LSG and LRYGB in long-term treatment of DM2 [5]. However, we hypothesized that daily glycemic excursions in morbidly obese patients after LRYGB would differ significantly from those following LSG.
A comprehensive record of the changes in glucose homeostasis can be achieved by continuous glucose monitoring (CGM), which permits recording of 288 data points every 24 h. We therefore aimed to use this to monitor interstitial glucose concentrations in the perioperative period for patients who were undergoing bariatric surgery.
Materials and Methods
Study Design
A prospective observational study was performed using data derived from the anamnesis, physical examination, and the results of CGM, of consecutive patients in a tertiary academic referral surgical center.
Inclusion criteria:
-
Patients aged 18–65 years;
-
Patients with a body mass index (BMI) of 35–50 kg/m2;
-
Patients qualified for bariatric procedures (LSG or LRYGB) according to the Polish Guidelines for Bariatric and Metabolic Surgery [6, 7];
-
Patients who had been diagnosed with DM2 at least 6 months prior to the surgery, but who had had the disease for ≤ 5 years, and who were taking oral anti-diabetic medications (≤ 4), but not insulin (the DM2 group); OR an absence of diabetes mellitus (the control group);
Exclusion criteria:
-
Patients with complications following diabetes mellitus (diabetic nephropathy, diabetic retinopathy, diabetic neuropathy, or diabetic foot ulcers), type 1 diabetes, secondary diabetes, chronic pancreatitis, or oral steroid therapy;
-
Patients undergoing a revision procedure;
-
Patients with a diagnosis of mental illness that would impede cooperation;
-
Alcohol or drug abuse;
Study phases:
-
1.
Preparation and preoperative clinical assessment: informed consent, full clinical examination, measurement of body mass, calculation of BMI, and baseline evaluation of biochemical parameters (including fasting glucose and hemoglobin A1c [HbA1c]). Patients were divided in two groups on the basis of the procedure performed (LSG or LRYGB), with subgroups of individuals defined by the presence or absence of DM2.
-
2.
Perioperative CGM using a FreeStyle Libre system: continuous monitoring of interstitial glucose concentration in the patients’ subcutaneous tissue. Preoperative mean daily glucose concentration was measured from the day prior to surgery starting at 8–9 am, up to the beginning of anesthesia (24 h, labeled as “day 1 of CGM”). Then, the measurement labeled as “day 2 of CGM” started. For 10 consecutive days, CGM was performed. Patients were discharged from hospital at day 3, since admission (postoperative day 2) and CGM was continued in patients’ homes.
-
3.
Devices were returned after completing 10 days of CGM, during follow-up visits. Adverse events were recorded at this time.
A study flow diagram is presented as Fig. 1.
Treatment Protocol
Patients were treated in accordance with the Enhanced Recovery after Surgery (ERAS) protocol, with regard to preoperative, intraoperative, and postoperative interventions [6, 8,9,10]. During the preoperative period, patients were appropriately counseled and thoroughly examined, with particular emphasis on the presence and management of DM2 and any significant comorbidities. Preoperatively, patients were scheduled for educational meetings, visits with the dietician, who is teaching them what and how to eat postoperatively. Patients’ diets were standardized during hospital stay. On admission day, a normocaloric diet was administered. Fasting time was started 6 h before anesthesia, while clear liquids were acceptable up to 2 h before. On the operation day, intravenous glucose and insulin were administered by anesthesiologist, if necessary. Postoperatively, patient was encouraged to drink clear liquids. If tolerated, patients were given yoghurt and high protein drinks in the evening. From the day after operation, patients were advanced to liquid diet, then received strict dietary recommendations to stay on liquid diet for the first month postoperatively. Postoperatively, patients were not on oral anti-diabetic medications. Then, in the first month, they had a follow-up visit with diabetologist, who was administering anti-diabetic medications if necessary (based on glucose profile done based on glucose finger prick testing). All patients were scheduled to have at least three follow-up appointments: 2 weeks, 1 month, and 3 months after discharge.
Surgical Techniques
The surgical techniques for LSG and LRYGB were standardized and have been described in previous publications [9, 11, 12]. Sleeve gastrectomy was commenced 4–5 cm proximal to the pylorus, followed by 38 F bougie trimming. During LRYGB, a pouch was formed using three 45-mm staplers (one horizontal and two vertical) and a gastrojejunal anastomosis was created using a linear stapler. The length of the Roux and biliopancreatic limbs was standardized to be up to 150 and 100 cm, respectively.
Continuous Glucose Monitoring Technique
The Freestyle Libre CGM is used for the continuous measurement of glucose concentration in the interstitial fluid (ISF) of subcutaneous tissue for up to 14 days. It is coupled with a sensor, which consists of a thin needle placed in the subcutaneous tissue on the posterior surface of the arm. If the patients were not able to reach the posterior surface of their arm, the sensor was allowed to be placed at anterior facet of abdominal wall, however none required that placement. Glucose oxidase, at the end of needle in subcutaneous tissue, catalyzes the glucose oxidation reaction that causes electrons to be transferred to a thin sensor needle. The resulting electric current is registered by the sensor and converted by the Freestyle Libre CGM into glucose concentration. The measurements are automatically saved on the device and can be synchronized and downloaded to a computer. The device is a wireless system and its use does not require additional training of the patient. Freestyle Libre CGM Software was used to analyze daily glycemic trends. The measurement error does not exceed 10% [13,14,15,16] and the system was validated for use in the operating room and intensive care unit [17]. The subcutaneous tissue comprises of interstitial fluid, which contains glucose transported from blood capillaries by simple diffusion [18]. The glucose concentration in the ISF closely follows blood glycemia, however with a slight time delay (between 5 and 10 min in different studies) [19]. For compensation in CGM devices, complex algorithms are employed, which can adjust for rapid changes of glycemia and time delays, resulting in more accurate glucose measurements for the end user [14, 20, 21].
Outcomes
The primary outcome was to record the fluctuation in interstitial glucose concentration each day in patients undergoing LSG or LRYGB.
Statistical Analysis
Comparisons of baseline patient data were conducted using Student’s t test or the Mann-Whitney U test for quantitative variables, and the chi-square test, with or without Yates’s correction, for qualitative variables. All repeated measurements were analyzed with MANOVA or Friedman ANOVA, with post hoc analyses. Results were considered significant with p value < 0.05. Data were analyzed using Statistica version 13.0 PL (StatSoft Inc., Tulsa, OK, USA).
Results
Characteristics of the Study Group
We enrolled 32 patients undergoing surgery in the 2nd Department of General Surgery, Jagiellonian University Medical College. There were 12 men and 20 women, with a mean age of 43 ± 10 years. Eighteen patients underwent LSG (10 men and 8 women), while 14 underwent LRYGB (2 men and 12 women).
The baseline characteristics of patients with and without DM2, who qualified for bariatric procedures, are presented in Table 1. Patients with DM2 were mostly assigned to LRYGB (62.5 vs. 25%). There were no differences in sex distribution between the DM2 and control groups. However, patients with DM2 were significantly older than controls [46.5 (40–58.5) vs. 39 (30–44.5)]. Comorbidity index, assessed using American Society of Anesthesiologists class (ASA class), was higher in DM2 patients, reflecting higher prevalence of arterial hypertension, coronary and peripheral vascular disease, and obstructive sleep apnea. The preoperative metabolic panel was comparable in the DM2 patients and control group. In the group of patients assigned to LSG, most were male (56%), while the opposite was true for those assigned to LRYGB (14%) (p = 0.020; subsequent ANOVA analyses were standardized with regard to sex). Age did not differ among the surgical subgroups, and neither did maximal preoperative BMI, nor BMI on admission to hospital. The median duration of DM2 was 2.5 (1.5–3.5) years, with no significant difference between the type of procedure undergone (p = 0.062). Fourteen patients were being treated with metformin (eight patients with prolonged-release tablets at 1000 mg/dose and six patients with coated tablets at doses of 500 or 850 mg, with the appropriate daily dose having been determined by a diabetes specialist) and two were being treated with gliclazide (prolonged-release tablets; 30 mg daily). The patients’ DM2 was well-controlled by their oral medication, which was reflected in a median HbA1c concentration of 5.5% (5.4–5.9%). The median HbA1c in non-diabetic individuals was 5.3% (5.2–5.4%; p = 0.460). Preoperative mean daily non-fasting glucose concentrations did not differ between patients with DM2 and those without (p = 0.622).
Main Outcomes
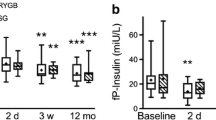
The median postoperative glucose concentration over the entire study was 4.6 (4.1–5.2) mmol/L and did not differ between the groups [LSG vs. LRYGB, p = 0.426; DM2 vs. control, p = 0.469 (standardized for differences in sex distribution)]. In all 32 patients, glucose concentration was within the target range (3.9–6.7 mmol/L) 68% of the time over the 10-day postoperative period of the study. During this time, we recorded 12 ± 6 low glucose events (< 3.9 mmol/L) per patient, which were more frequent in patients being treated for DM2 than in those without the disease (14 ± 5 vs. 9 ± 6; p = 0.035). The mean duration of a hypoglycemic event was 245 (165.5–364) min. Table 2 presents the CGM data for patients with DM2 after either LSG or LRYGB. After LRYGB, patients with DM2 had a higher incidence of low glucose concentration episodes (< 3.9 mmol/L), which lasted significantly longer than they did in patients with DM2 who had undergone LSG (p = 0.035 and 0.049, respectively). Mean daily glucose concentration on day 1 and days 2–3 did not differ between the groups. Significantly lower glucose concentrations were measured from fourth day of CGM (third postoperative day) until the end of the observation period in patients with DM2 that had undergone LRYGB, compared with patients with DM2 that had undergone LSG. Symptomatic hypoglycemic events were observed in four patients after LRYGB with DM2. They required infusions of intravenous glucose due to altered mental status or symptoms of increased activity of sympathetic system. Only two patients, both after LSG, did not suffer from any hypoglycemia. Low glucose concentrations, either symptomatic or asymptomatic, were present both after LSG and LRYGB respectively in 16 and 14 patients. The variations in daily glucose concentrations are presented in Fig. 2.
In Table 3 we show a comparison of CGM data for patients without DM2 following LSG or LRYGB. There were no significant differences in mean glucose concentration over the whole period, nor in the incidence of low glucose events or their duration. The variations in glucose concentrations are presented in Fig. 3.
Table 4 shows comparison of studied parameters of CGM in all LSG vs. all LRYGB patients. We were able to document significantly lower mean glucose concentrations in all LRYGB on days 7–10 of CGM in comparison with patients after LSG. Additionally, Fig. 4 demonstrates significant increase in mean glucose concentrations from days 2 to 6 of CGM present after both types of procedures. On days 7–10 of CGM, mean glucose concentrations after LRYGB were significantly lower than on day 1, which was not observed in case of patients after LSG.
Discussion
This pilot study is one of the few studies that has been conducted using CGM to compare glucose metabolism during a significant period (10 days) following LSG and LRYGB. Our main goal was to investigate changes in glycemic control in the early postoperative period and to compare daily glucose fluctuations in patients who underwent LRYGB and LSG. We included 16 patients with DM2 and 16 in control group. Patients with DM2 predominantly underwent LRYGB and were significantly older than in control group. ASA class was higher in DM2 patients, what was reflected by higher comorbidity index. Diabetes mellitus was well-controlled on oral medications, which reflects in preoperative HbA1c and means of daily glucose concentrations on the day prior to operations. We recorded metabolic reaction to surgery, which is reflected by significantly higher glucose concentrations on the first and second postoperative day after both LSG and LRYGB, which normalized overtime. Starting from the third day after surgery, significantly lower glucose concentrations were measured in patients with DM2 that had undergone LRYGB, compared with patients with DM2 that had undergone LSG. In patients without DM2, there were no significant differences in mean glucose concentration during the observation period, or in the incidence or duration of low glucose events, between those who had undergone LSG and LRYGB.
Previously published studies of the changes in glucose status during the postoperative period after surgical treatment of obesity that used CGM were conducted over a shorter period and focused only on patients who had undergone gastric bypass or had DM2 [22, 23]. Numerous publications have demonstrated the clinical benefits of the CGM system used in this study in various patient populations. These included pediatric, adolescent, and adult patients with type 1 and type 2 diabetes, patients with poor baseline glycemic control, and patients undergoing bariatric surgery [24,25,26,27,28,29,30,31]. The use of this system is associated with an improvement in HbA1c and a reduction in the risk of hypoglycemia [29]. This is because continuous subcutaneous glucose measurement provides the most relevant information regarding glucose status of the available methods [32].
Bariatric surgery improves glycemic control by multiple weight-dependent and weight-independent mechanisms, which have their origin in the gastrointestinal system [33]. This study investigated the changes in glucose status for a relatively short period of 10 days, which did not allow us to draw conclusions regarding the resolution of DM2 after bariatric surgery. However, previous publications have reported that shortly after both LRYGB and LSG there is an improvement in glycemic control in patients with DM2. The main finding of this study was that there are significantly lower glucose concentrations from the third postoperative day in patients with DM2 that undergo LRYGB, compared with patients with DM2 that undergo LSG. This could be explained by greater incretin release following LRYGB. This finding, if replicated in a larger-scale, longer-term study, preferably a randomized controlled trial (RCT), would indicate a need for an early reduction in the dose of administered DM2 medication.
The prevalence of symptomatic hypoglycemic events have been reported as 0.1%, based on self-reported episodes or hospital admissions for hypoglycemia [34, 35]. Nevertheless, another study reported prevalence of 34% basing on self-reported symptoms consistent with hypoglycemia [36]. Direct testing, either with oral glucose test or CGM, showed that it can be present even in 10–70% patients [37,38,39,40]. In case of our study, symptomatic hypoglycemia (defined as need for intervention due to altered mental status or severe sympathetic symptoms) was observed in 12.5% of patients. Asymptomatic hypoglycemic events were recorded in almost all patients.
In patients without DM2 that had undergone LSG or LRYGB, we did not show significant differences in mean glucose concentration over time, or in the incidence or duration of low glucose events, which is not consistent with some reports that have documented postoperative hypoglycemia in non-diabetic patients. Following bariatric surgery, hepatic insulin sensitivity is elevated because of caloric restriction and an increase in β-cell insulin secretion, secondary to an increase in postprandial GLP-1 secretion, caused by changes in the nutrients entering the distal small intestine [41,42,43]. Non-diabetic patients are commonly affected by hypoglycemic episodes after the surgical treatment of obesity [39, 44]. A study by Tharakan et al. demonstrated associations between higher plasma GLP-1, glucagon, and the hyperinsulinemic hypoglycemia observed in this situation [45]. Yip et al. showed that both LRYGB and LSG reduce glycemia and increase glucose tolerance [46], while Kellog et al. proposed that hyperinsulinemic hypoglycemia results from a severe form of late dumping syndrome after gastric bypass surgery, and can be significantly ameliorated through dietary intervention [47]. Despite including patients with short duration of DM2 and not on insulin injections, the incretin effect was stronger in patients without DM2 than in patients with DM2. This was reflected by higher prevalence of low glucose concentrations overtime (19.5 and 31% in no-DM2 subgroups vs. 1 and 25% in DM2 subgroups) and low glucose events (14.8 and 12.5 in non-DM2 vs. 5 and 11.6 in DM2 subgroups). However we did not find research investigating that phenomenon. Degeneration of pancreatic β-cells is pathophysiologically related to onset of DM2 along with peripheral insulin resistance. We can only hypothesize that in patients with DM2, the degeneration of β-cells is weakening incretin effect.
We observed a rapid elevation in interstitial glucose concentration after surgery, which was similar between patients with and without DM2. This increase was larger in the LSG group, although the difference between the type of procedure was not statistically significant. Patients regained their preoperative glucose concentration after ~ 7–10 days. Gastrointestinal surgery is associated with a complex metabolic response, as well as surgical stress inducing endocrine and inflammatory responses. During the period following a gastrointestinal procedure, patients experience elevations in cortisol, growth hormone, glucagon, catecholamine, and pro-inflammatory cytokines (interleukins, IL-1 and IL-6), followed by increases in anti-inflammatory cytokines [48, 49]. Prior to conducting surgery on patients with DM2, preoperative assessment and planning is required to establish a suitable treatment regimen that will minimize the risk of complications [50, 51]. Previous studies, in addition to our data, have shown that the period following a surgical procedure is often characterized by hyperglycemia, which results in a greater incidence of complications and higher costs connected to hospitalization [52,53,54].
Despite a limited number of patients, we were able to demonstrate a significant difference in the mean daily glucose concentrations on days 4–6 and 7–10 in patients with DM2 after LRYGB in comparison to patients with DM2 after LSG. Additionally, we found significantly more frequent low glucose concentration events and a longer time of those events in the first subgroup. We suggest that with larger study population there would also likely be a significant difference in the frequency of glucose concentrations below targeted compartment (LRYGB vs. LSG, 25 and 1%) and above the targeted compartment (LRYGB vs. LSG, 1 and 11%). In that situation, LRYGB would be a more curative procedure for DM2 in the early postoperative period. Supportive observation is that when analyzing all LSG vs. all LRYGB patients, we found significant difference in mean glucose concentrations on the days 7–10, lower in the LRYGB subgroup. Perioperative shock reaction was an increase in mean glucose concentrations from days 2 to 6 of CGM present after both types of procedures, as mentioned previously. On days 7–10 of CGM, mean glucose concentrations after LRYGB were significantly lower than on day 1, what was not observed in case of patients after LSG.
We can speculate that more significant findings and correlations would have been identified if the study had been conducted on a larger group of patients. However, an appropriate sample size for a more comprehensive future study can be calculated using the data presented in this publication. Unfortunately, for the moment, the differences in glucose status in the period following LSG and LRYGB remains to be conclusively established.
Limitations
This study had several limitations. First, the sample size was small and the duration of observation was short, because of funding restrictions. Therefore, we decided to conduct a pilot study, which would validate methodology for a more comprehensive follow-up study, preferably an RCT. A potential source of bias associated with this study is an error in glucose measurement, as described by the CGM device manufacturer, as well as patient error, although a precise description of the device, including data on measurement error, has been added to the manuscript, and patients were thoroughly instructed on the use of the CGM device prior to their enrolment in the study. Further studies of larger groups of patients, categorized according to the clinical severity of their DM2, and conducted over a longer period, are required.
Conclusions
In conclusion, significantly lower glucose concentration is present from the third postoperative day in patients with DM2 that undergo LRYGB, than in those that undergo LSG. However, patients with DM2 that undergo LRYGB are more likely to experience low glucose episodes and these are likely to be longer, than in those that undergo LSG. This indicates the dose of anti-diabetic medication should be reduced in the former group, even before significant weight reduction occurs. CGM permits a very effective demonstration of the perioperative metabolic reaction to bariatric procedures.
References
Rometo D, Korytkowski M. Perioperative glycemic management of patients undergoing bariatric surgery. Curr Diab Rep. 2016;16:23.
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care. 2016;39:861–77.
Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Complete guidelines. Endocr Pract. 2016;22:842–84.
Janik MR, Stanowski E, Paśnik K. Present status of bariatric surgery in Poland. Videosurgery Other Miniinvasive Tech [Internet]. 2016;1:22–5. Available from:. https://doi.org/10.5114/wiitm.2016.58742.
Zhang C, Yuan Y, Qiu C, et al. A meta-analysis of 2-year effect after surgery: laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for morbid obesity and diabetes mellitus. Obes Surg. 2014;24:1528–35.
Budzyński A, Major P, Głuszek S, et al. Polskie rekomendacje w zakresie chirurgii bariatrycznej i metabolicznej. Med Prakt – Chir. 2016;6:13–25.
Wyleżoł M, Paśnik K, Dąbrowiecki S, et al. Polish recommendations for bariatric surgery. Wideochirurgia i inne Tech małoinwazyjne/Videosurgery Other Miniinvasive Tech Suppl. 2009;4:8.
Małczak P, Pisarska M, Piotr M, et al. Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg. 2017;27:226–35.
Major P, Stefura T, Malczak P, et al. Postoperative care and functional recovery after laparoscopic sleeve gastrectomy vs. laparoscopic Roux-en-Y gastric bypass among patients under ERAS protocol. Obes Surg. 2018;28:1031–9.
Kostecka M, Bojanowska M. Problems in bariatric patient care—challenges for dieticians. Videosurgery Other Miniinvasive Tech [Internet]. 2017;3:207–15.
Major P, Wysocki M, Torbicz G, et al. Risk factors for prolonged length of hospital stay and readmissions after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2017;28:1–10.
Major P, Janik MR, Wysocki M, et al. Comparison of circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass: a multicenter study. Wideochirurgia I Inne Tech Maloinwazyjne. 2017;12:140–6.
Damiano ER, El-Khatib FH, Zheng H, et al. A comparative effectiveness analysis of three continuous glucose monitors. Diabetes Care. 2013;36:251–9.
Bailey T, Bode BW, Christiansen MP, et al. The performance and usability of a factory-calibrated flash glucose monitoring system. Diabetes Technol Ther. 2015;17:787–94.
Pleus S, Schoemaker M, Morgenstern K, et al. Rate-of-change dependence of the performance of two CGM systems during induced glucose swings. J Diabetes Sci Technol. 2015;9:801–7.
Nakamura Y, Matsumoto S, Matsushita A, et al. Pancreaticojejunostomy with closure of the pancreatic stump by endoscopic linear stapler in laparoscopic pancreaticoduodenectomy: a reliable technique and benefits for pancreatic resection. Asian J Endosc Surg. 2012;5:191–4.
Munekage M, Yatabe T, Sakaguchi M, et al. Comparison of subcutaneous and intravenous continuous glucose monitoring accuracy in an operating room and an intensive care unit. J Artif Organs. 2016;19:159–66.
Cengiz E, Tamborlane WV. A tale of two compartments: interstitial versus blood glucose monitoring. Diabetes Technol Ther [Internet]. 2009;11:S-11–6. Available from:. https://doi.org/10.1089/dia.2009.0002.
Rebrin K, Sheppard NF, Steil GM. Use of subcutaneous interstitial fluid glucose to estimate blood glucose: revisiting delay and sensor offset. J Diabetes Sci Technol. 2010;4:1087–98.
Shi T, Li D, Li G, et al. Modeling and measurement of correlation between blood and interstitial glucose changes. J Diabetes Res. 2016;2016:1–9.
Koutny T. Blood glucose level reconstruction as a function of transcapillary glucose transport. Comput Biol Med. 2014;53:171–8.
Ramos-Leví AM, Sánchez-Pernaute A, Marcuello C, et al. Glucose variability after bariatric surgery: is prediction of diabetes remission possible? Obes Surg. 2017;27:3341–3.
Hanaire H, Dubet A, Chauveau ME, et al. Usefulness of continuous glucose monitoring for the diagnosis of hypoglycemia after a gastric bypass in a patient previously treated for type 2 diabetes. Obes Surg. 2010;20:126–9.
Tramunt B, Vaurs C, Lijeron J, et al. Impact of carbohydrate content and glycemic load on postprandial glucose after Roux-en-Y gastric bypass. Obes Surg. 2016;26:1487–92.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359:1464–76.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Effectiveness of continuous glucose monitoring in a clinical care environment: evidence from the Juvenile Diabetes Research Foundation continuous glucose monitoring (JDRF-CGM) trial. Diabetes Care. 2010;33:17–22.
Chase HP, Beck RW, Xing D, et al. Continuous glucose monitoring in youth with type 1 diabetes: 12-month follow-up of the Juvenile Diabetes Research Foundation continuous glucose monitoring randomized trial. Diabetes Technol. Ther. 2010;12:507–15.
Lawson ML, Bradley B, McAssey K, et al. The JDRF CCTN CGM TIME trial: timing of initiation of continuous glucose monitoring in established pediatric type 1 diabetes: study protocol, recruitment and baseline characteristics. BMC Pediatr. 2014;14:183.
Vigersky RA. The benefits, limitations, and cost-effectiveness of advanced technologies in the management of patients with diabetes mellitus. J Diabetes Sci Technol. 2015;9:320–30.
Klonoff DC, Buckingham B, Christiansen JS, et al. Continuous glucose monitoring: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:2968–79.
Ehrhardt NM, Chellappa M, Walker MS, et al. The effect of real-time continuous glucose monitoring on glycemic control in patients with type 2 diabetes mellitus. J Diabetes Sci Technol. 2011;5:668–75.
Klonoff DC. The need for separate performance goals for glucose sensors in the hypoglycemic, normoglycemic, and hyperglycemic ranges. Diabetes Care. 2004;27:834–6.
Andrew CA, Umashanker D, Aronne LJ, et al. Intestinal and gastric origins for diabetes resolution after bariatric surgery. Curr Obes Rep. 2018;7:139–46.
Marsk R, Jonas E, Rasmussen F, et al. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in Sweden. Diabetologia. 2010;53:2307–11.
Sarwar H, Chapman WH, Pender JR, et al. Hypoglycemia after Roux-en-Y gastric bypass: the BOLD experience. Obes Surg. 2014;24:1120–4.
Lee CJ, Clark JM, Schweitzer M, et al. Prevalence of and risk factors for hypoglycemic symptoms after gastric bypass and sleeve gastrectomy. Obesity. 2015;23:1079–84.
Pigeyre M, Vaurs C, Raverdy V, et al. Increased risk of OGTT-induced hypoglycemia after gastric bypass in severely obese patients with normal glucose tolerance. Surg Obes Relat Dis. 2015;11:573–7.
Roslin MS, Oren JH, Polan BN, et al. Abnormal glucose tolerance testing after gastric bypass. Surg Obes Relat Dis. 2013;9:26–31.
Abrahamsson N, Eden Engstrom B, Sundbom M, et al. Hypoglycemia in everyday life after gastric bypass and duodenal switch. Eur J Endocrinol. 2015;173:91–100.
Kefurt R, Langer FB, Schindler K, et al. Hypoglycemia after Roux-En-Y gastric bypass: detection rates of continuous glucose monitoring (CGM) versus mixed meal test. Surg Obes Relat Dis. 2015;11:564–9.
Madsbad S, Dirksen C, Holst JJ. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol. 2014;2:152–64.
Ribaric G, Buchwald JN, Mcglennon TW. Diabetes and weight in comparatice studies of biriactric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24:437–55.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Lee CJ, Brown TT, Schweitzer M, et al. The incidence and risk factors associated with developing symptoms of hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2018;14:1–6.
Tharakan G, Behary P, Wewer Albrechtsen NJ, et al. Roles of increased glycaemic variability, GLP-1 and glucagon in hypoglycaemia after Roux-en-Y gastric bypass. Eur J Endocrinol. 2017;177:455–64.
Yip S, Signal M, Smith G, et al. Lower glycemic fluctuations early after bariatric surgery partially explained by caloric restriction. Obes Surg. 2014;24:62–70.
Kellogg TA, Bantle JP, Leslie DB, et al. Postgastric bypass hyperinsulinemic hypoglycemia syndrome: characterization and response to a modified diet. Surg Obes Relat Dis. 2008;4:492–9.
Scott MJ, Baldini G, Fearon KCH, et al. Enhanced Recovery after Surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand. 2015;59:1212–31.
Saito T, Tazawa K, Yokoyama Y, et al. Surgical stress inhibits the growth of fibroblasts through the elevation of plasma catecholamine and cortisol concentrations. Surg Today. 1997;27:627–31.
Levesque CM. Perioperative care of patients with diabetes. Crit Care Nurs Clin North Am. 2013;25:21–9.
Coan KE, Schlinkert AB, Beck BR, et al. Clinical inertia during postoperative management of diabetes mellitus: relationship between hyperglycemia and insulin therapy intensification. J Diabetes Sci Technol. 2013;7:880–7.
Won EJ, Lehman EB, Geletzke AK, et al. Association of postoperative hyperglycemia with outcomes among patients with complex ventral hernia repair. JAMA Surg. 2015;150:433–40.
Huang P, Lin M, Wen J, et al. Correlation of early postoperative blood glucose levels with postoperative complications, hospital costs, and length of hospital stay in patients with gastrointestinal malignancies. Endocrine. 2015;48:187–94.
Buehler L, Fayfman M, Alexopoulos A-S, et al. The impact of hyperglycemia and obesity on hospitalization costs and clinical outcome in general surgery patients. J Diabetes Complicat. 2015;29:1177–82.
Acknowledgments
We thank Mark Cleasby, PhD, from Edanz Group (www.edanzediting.com/ac) for language editing of this manuscript.
Funding
This study was funded by Grant of Students’ Scientific Society of Jagiellonian University Medical College, Krakow (#24/2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures followed the ethical standards of the responsible committee on human experimentation (institutional and national) and the 2013, Fortaleza revision of the 1964 Declaration of Helsinki. The study was approved by the independent ethics committee of the Jagiellonian University, Krakow, Poland (122/6120/5/2017). Informed consent for the study and surgical treatment was obtained from all patients before the procedure.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wysocki, M., Szopa, M., Stefura, T. et al. Continuous Glucose Monitoring in Bariatric Patients Undergoing Laparoscopic Sleeve Gastrectomy and Laparoscopic Roux-En-Y Gastric Bypass. OBES SURG 29, 1317–1326 (2019). https://doi.org/10.1007/s11695-018-03684-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-03684-5