Abstract
Background
Surgical training may potentially influence patient care. A safe, high-quality bariatric and metabolic surgery practice requires dedicated and specialized training commonly acquired during a fellowship. This study evaluates the impact of fellow participation on early postoperative outcomes in bariatric surgery.
Methods
From the American College of Surgeons (ACS-NSQIP) database, we identified all obese patients who had undergone primary laparoscopic Roux-en-Y gastric bypass (LRYGB) and sleeve gastrectomy (LSG) between 2010 and 2012. Logistic regression was used to prognosticate the surgical fellow (PGY-6, 7, or 8) participation in bariatric surgeries on perioperative outcomes, as compared to surgeries with no trainee participation.
Results
The study cohort consisted of 10,838 patients (8819 LRYGB, 2019 LSG, 32 % fellow participation). Fellows participated in higher-risk surgeries. Fellow involvement was associated with increased operative time in LRYGB (difference 42.4 ± 1.2 min, p < 0.001) and in LSG (difference 38.8 ± 2.5 min, p < 0.001). Multivariate regression revealed that fellow involvement in LSG did not significantly alter postoperative adverse events. Conversely, in the LRYGB group, fellow participation was independently associated with higher rates of overall complications (OR = 1.37, 95 % CI 1.16–1.63), serious complications (OR = 1.23, 95 % CI 1.00–1.52), surgical complications (OR = 1.42; 95 % CI 1.17–1.73), and reoperation (OR = 1.43, 95 % CI 1.10–1.87). On adjusted analysis, while readmission was higher with fellow involvement in both procedures, mortality rates were comparable.
Conclusions
Fellow involvement resulted in a clinically appreciable increase in operative times. Fellow participation in the operating room was also independently associated with worse early postoperative outcomes following LRYGB, but was not the case for LSG. Promoting proficiency in surgical simulation laboratories and a gradual participation of fellows from LSG to LRYGB during fellowship may be associated with a reduction in postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The growing pandemic of obesity and diabetes, along with the relative ineffectiveness of conventional weight reduction therapies in severely obese population, has led to a significant rise in the number of surgical weight loss procedures in the last two decades [1–3]. In 2013, the total number of bariatric procedures performed worldwide was near 500,000, 96 % of which were carried out laparoscopically. North America was the region with the highest number of bariatric procedures [4]. As the number of centers doing bariatric and metabolic surgery has increased, a heightened awareness of quality improvement measures and perioperative outcomes has become the focus of hospital administrations and surgeons alike. Improvement in surgical techniques and perioperative management protocols has led to continuous improvement of the safety profile of bariatric surgery [5–8]. What is quite evident is that high-volume surgeons and high-volume centers achieve better outcomes. A recent systematic review of the literature found a positive association between surgeon and hospital volume with patient outcomes [9]. The Metabolic Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), which is the national bariatric surgery accreditation program established in 2012, continues to investigate how to improve overall surgical outcomes in today’s laparoscopic era [10].
Parallel to the rise in laparoscopic bariatric surgery over the past 10 years, an increasing number of bariatric fellowship programs have developed around the country. Mainly in response to meet the demands of inadequately trained general surgeons finishing their residencies, these training programs focus on teaching advanced minimally invasive surgical techniques and in particular, laparoscopic bariatric procedures. According to the most recent update from the Fellowship Council (FC) website, there are 61 accredited 1-year bariatric surgical fellowship programs in North America training about 77 clinical surgical fellows each year [11]. The American Society for Metabolic and Bariatric Surgery (ASMBS) certifies satisfactory fellowship training if graduating fellow meets the educational requirements needed to practice safe and effective bariatric surgery [12]. Although high-volume bariatric centers have been shown to produce better outcomes [9], what is not evident is the association between patient outcomes and trainee participation in surgery. Numerous reports in the literature have reported mixed results analyzing general surgical outcomes with resident involvement [13–19], but there are limited reports examining the impact fellows have on bariatric surgical outcomes [20–22].
The aim of this study was to examine the impact of fellow involvement on early postoperative adverse outcomes following laparoscopic Roux-en-Y gastric bypass (LRYGB) and sleeve gastrectomy (LSG).
Methods
This study was based on the data from the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) database between 2010 and 2012. ACS-NSQIP prospectively collects information on over 300 variables, including demographic variables, comorbidities, laboratory values, and 30-day postoperative morbidity and mortality outcomes for patients undergoing major surgical procedures in over 430 participating community and academic centers in the USA by the end of 2013. The ACS-NSQIP utilizes several mechanisms to ensure that the data collected are of the highest consistency and reliability [23].
We identified adult patients with body mass index (BMI) ≥ 35 kg/m2, who underwent elective LRYGB and LSG using their respective Current Procedural Terminology codes (LSG 43775; LRYGB 43644, 43645). All operations were performed laparoscopically. We excluded patients, who underwent a revisional or open bariatric procedure along with a procedure coded as emergent. Patients who had a surgery in the 30 days prior to the index bariatric surgery and cases with any evidence of preoperative sepsis, disseminated cancer, and American Society of Anesthesiology (ASA) class 5 (Moribund) were also excluded.
The main exposure variable was the fellow participation in bariatric surgeries as compared to no trainee participation (attending/surgeon only). We identified fellows as trainees in post-graduate year (PGY) 6, 7, or 8. Independent demographic variables were age, sex, weight, BMI, and race. Examined comorbidities included diabetes mellitus, hypertension, history of cardiac disease (binary variable representing congestive heart failure (CHF), angina, myocardial infarction, cardiac interventions, and cardiac surgeries), chronic obstructive pulmonary diseases, history of cerebrovascular diseases (binary variable representing transient ischemic attack and stroke), chronic renal failure requiring dialysis, and chronic steroid use. Other baseline characteristics included were active smoking and functional status. Preoperative laboratory variables included serum hematocrit, albumin, and creatinine. All variables are clearly defined in the ACS-NSQIP database user guide [23]. Operative variables considered were the ASA classification, type of bariatric surgery, and operation time.
Outcomes were chosen as the 30-day postoperative composite “overall complication” defined as presence of any of 18 adverse events including urinary tract infection (UTI), wound infection, organ/space surgical site infection (SSI), myocardial infarction (MI), cardiac arrest, progressive renal insufficiency, acute renal failure (ARF), deep vein thrombosis (DVT), pulmonary embolism (PE), pneumonia, reintubation, failure to wean (mechanical ventilation >48 h), stroke, sepsis, septic shock, bleeding (need for transfusion), reoperation, and death. We also defined a “serious complication” as a composite binary variable representing the occurrence of any major postoperative complication, which excludes urinary tract and wound infections. Finally, a “surgical complication” was defined as a composite binary variable representing the occurrence of surgical complications, which includes wound infections, organ/space surgical site infection (SSI), bleeding led to transfusion, and 30-day reoperation. Thirty-day readmission was also considered as an endpoint in the statistical analysis.
Statistical Analysis
The information on the study parameters are expressed as mean ± standard deviation (SD) and number (%). Cases performed with fellows’ involvement and those carried out by the attending/surgeon only were compared using chi-square or fisher’s exact tests for categorical variables and student’s t test or Mann-Whitney U tests for continuous variables. Logistic regression models were fit to examine the contribution of fellow involvement on outcomes. Multivariate models included patient characteristics with p < 0.1 found in univariate analysis for each outcome, and adjustments were made in a backward stepwise elimination pattern. Odds ratios (OR) along with 95 % confidence intervals (CI) were reported, and inference was based on a two-sided 5 % level. In multiple comparisons (effect of fellow participation on each individual 16 postoperative adverse events), significance level was corrected using Bonferroni’s correction, and p < 0.003 was considered as significant. The analysis was carried out using SPSS (Version 20, Chicago Inc, IL, USA).
Results
The study cohort consisted of 10,838 patients including 8819 patients who underwent LRYGB and 2019 who had LSG. Fellows were involved in 2795 (31.7 %) cases of LRYGB and 641 (31.7 %) cases of LSG. Table 1 highlights the baseline characteristics between the two groups. Fellows were involved in higher-risk cases including patients with higher BMI. Patients in the fellow involvement group were more likely to have some comorbid conditions (Table 1).
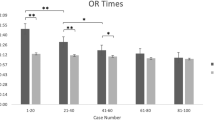
Fellow involvement was associated with increased operative time in LRYGB (average mean difference 42.4 ± 1.2 min, p < 0.001) and in LSG (average mean difference 38.8 ± 2.5 min, p < 0.001, Table 2).
Multivariate logistic regression revealed that fellow involvement in LSG did not significantly alter overall complications (OR = 1.31, 95 % CI 0.89–1.93), serious complications (OR = 1.41, 95 % CI 0.91–2.20), surgical complications (OR = 0.91, 95 % CI 0.56–1.46), and 30-day reoperation (OR = 0.93, 95 % CI 0.47–1.86). Conversely, in the LRYGB group, fellow participation was independently associated with higher rates of overall complications (OR = 1.37, 95 % CI 1.16–1.63), serious complications (OR = 1.23, 95 % CI 1.00–1.52), surgical complications (OR = 1.42, 95 % CI 1.17–1.73), 30-day reoperation (OR = 1.43, 95 % CI 1.10–1.87), and 30-day readmission (OR = 3.15, 95 % CI 2.22–4.46). On adjusted analysis, mortality rates were comparable between both groups (Table 3).
In terms of comparison of 16 individual complications between two groups, multivariate analysis showed that wound infection (OR = 1.78, 95 % CI 1.27–2.50) was significantly higher in cases in which fellows performed the LRYGB compared to the attending only. While incidence of progressive renal insufficiency (defined as a rise in creatinine of >2 mg/dl from preoperative value) was significant between two LRYGB groups at p < 0.05, it did not reach to a conservative Bonferroni’s corrected threshold (p < 0.003). However, on adjusted analysis, other individual complication rates were not significantly different between two groups (data not shown). Of note, incidence of all of individual complications was <1 % in the entire cohort, except wound infection (2 %) and postoperative bleeding (1.3 %).
Discussion
During the 3-year study period, we noted different outcomes between the LSG and LRYGB when fellows performed or were involved in the operation. Regression analysis, adjusted for baseline characteristics, showed worsening of outcomes with fellow participation in LRYGB, which was not observed in LSG cases. The increased operative times when fellows were involved could be a contributing factor. LRYGB operation requires an advanced level of laparoscopic skills, one in which the surgeon must not only complete two intra-corporeal anastomoses safely but must also contend with the abundant visceral adiposity, increased abdominal wall torque, and enlarged livers obscuring the stomach that accompany patients with severe obesity. In fact, Schauer et al. showed that the learning curve for the LRYGB was 100 cases [24]. Higa et al. demonstrated a steep decline in operating times from 200 min in their initial LRYGB cases to 60–90-min range after having performed over 300 operations [25].
Our results are quite similar to the Bhayani and colleagues study which reported higher rates of superficial SSI, UTI, and sepsis, and overall morbidity in LRYGB performed by fellows compared to attending staff between the years 2005 and 2009. They also noted that the higher rates of complications only existed during the first half of the training year, and during the latter half of the fellowship year (i.e., January to July), complication rates were equivalent to cases performed by the attending only [20]. This finding supports the notion of a steep learning curve associated with the LRYGB, one that levels off after several months of training. In the current study, we did not have data to independently assess outcomes at different time frames of the fellowship year. Certainly, the expectation would be to see decreased operative times and thus decreased rates of complications for the cases in which the fellows were involved. Data of Michigan Bariatric Surgery Collaborative also shows that “resident” involvement in LRYGB was independently associated with an increased risk for wound infections and venous thromboembolism after controlling for patient comorbidity differences and surgeon/hospital case volume. With regard to venous thromboembolism, much of the resident effect appears to be mediated through prolonged operative times. However, operative duration did not fully account for the resident effect on wound infection rates [21]. Compatible with these two large studies [20, 21], after risk adjustment, we also observed a higher rate of overall morbidity and particularly wound infection with trainee involvement in LRYGB. Differences in operative skill (e.g., gentle tissue handling) between trainees and attending surgeons, more spillage of enteric juice during two anastomoses, break in sterile technique associated with a new practitioner in a new training environment, and longer operative time may play a role in the increased risk for wound infection [20, 21]. Our study, consistent with many others that have utilized the ACS-NSQIP database, did not show an increase in overall mortality despite the higher rates of early postoperative complications when trainees were involved in the operation [17, 18].
The current study is the only one known to date to report outcomes on fellows participating in LSG, which is currently as popular, if not more than the LRYGB [26]. We believe the learning curve can be shorter for the LSG, mainly because there are no anastomoses involved. Even though the mean duration of the operation increased by 39 min when fellows performed the LSG compared to the attending alone, we did not note higher rates of early postoperative complications. The only statistically significant adverse effect when fellows performed the LSG was higher 30-day readmission rates. It is difficult to determine the cause for higher readmissions since the respective readmission diagnoses are not available.
Though the results show higher early complication rates when fellows perform the LRYGB, these outcomes may vary at institutions that perform a high percentage of LRYGB compared to those that perform very few, given that it has already been shown that the outcomes of bariatric surgery are superior at high-volume centers (9). Our data does not stratify results based on high-volume centers versus low-volume since the information identifying the center is not provided in the ACS-NSQIP dataset. It would also be interesting to see if complication rates were less in centers where fellows perform a higher number of primary LRYGB procedures.
These data also highlight the importance of a strategic approach to improve and assess fellow technical proficiency outside the operating room in surgical simulation laboratories. As part of the core curriculum of surgical training, residents graduating from general surgery programs are required to pass Fundamentals of Laparoscopic Surgery (FLS). As part of the FLS program, trainees are required to complete basic laparoscopic skills, such as laparoscopic suturing and pattern cutting [27]. Box trainers which simulate the environment in obese patients’ peritoneal cavities (i.e., reduced exposure from visceral adiposity and enlarged livers) and live surgeries on animal models may help improve skills for surgeons in fellowship training and may also translate to better postoperative outcomes. Another possible approach would be a gradual participation of fellows from less complex procedure (LSG) to LRYGB during fellowship. Creating a time goal for fellows to accomplish critical steps of the operation can potentially prevent excessive operative times caused by technical inefficiency [20, 21].
There are inherent limitations when the ACS-NSQIP database is used that can introduce both selection and misclassification bias. ACS-NSQIP captures only a sample of all procedures from each participating center and does not collect data unique to bariatric surgery patients (preoperative comorbidities such as obstructive sleep apnea, pulmonary hypertension, and history of venous thromboembolism) or unique bariatric postoperative complications such as anastomotic leaks. Senior residents who took research time during residency could be misclassified as fellows (PGY 6, 7, or 8). Despite this shortcoming, our study conclusions can be still applicable to advanced trainees. Furthermore, the database only captures the overall frequency of participation, and we cannot determine what proportion of the procedure was actually performed by the fellow, thus the degree of involvement of the fellows cannot be determined. In addition, the level of involvement in postoperative care provided by the fellow is unclear. The database only includes short-term postoperative outcomes up to day 30, and one cannot conclude that the observed increase in the early postoperative complications following LRYGB when fellows were involved will translate into a long-term negative effect.
The effectiveness of bariatric surgery as a cure for obesity and its associated metabolic diseases has never been as apparent as it is today [28–30]. As the obesity epidemic continues to escalate, so does the need for trained bariatric and metabolic surgeons. Recent survey indicated that there has been a constant increase in the total number of bariatric procedures performed worldwide over the past 10 years [4]. Furthermore, in 2013, almost 96 % of bariatric procedures were performed laparoscopically with less complications and shorter hospital stays compared to older data with the open approach [1–4]. We need to continue to focus on improving the safety and efficiency of the operation through simulator-based training programs and structured, graduated responsibility in the operating room to train the next generation of metabolic and bariatric surgeons.
Conclusions
Regardless of the bariatric procedure, fellow involvement resulted in a clinically appreciable increase in operative times. In this analysis of multi-institutional data, fellow participation in the operating room was independently associated with worse early postoperative outcomes following LRYGB, but was not the case for LSG. These findings support the need for continuous close supervision of fellows during the learning phase of LRYGB. Moreover, promoting proficiency in surgical simulation laboratories and a gradual participation of fellows from LSG to LRYGB during fellowship may be associated with better patient care and a reduction in early postoperative complications.
References
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
ASMBS Estimate of Bariatric Surgery Numbers. Available at:http://asmbs.org/2014/03/estimate-of-bariatric-surgery-numbers/ Accessed August 15, 2015.
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg. 2011;213:261–6.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Aminian A, Brethauer SA, Kirwan JP, et al. How safe is metabolic/diabetes surgery? Diabetes Obes Metab. 2015;17:198–201.
Kim JH, Wolfe B. Bariatric/metabolic surgery: short- and long-term safety. Curr Atheroscler Rep. 2012;14:597–605.
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium, Flum DR, Belle SH, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–54.
Aminian A, Brethauer SA, Sharafkhah M, et al. Development of a sleeve gastrectomy risk calculator. Surg Obes Relat Dis. 2015;11:758–64.
Zevin B, Aggarwal R, Grantcharov TP. Volume-outcome association in bariatric surgery: a systematic review. Ann Surg. 2012;256:60–71.
Morton J. The first metabolic and bariatric surgery accreditation and quality improvement program quality initiative: decreasing readmissions through opportunities provided. Surg Obes Relat Dis. 2014;10:377–8.
Directory of Fellowships. Available at: https://fellowshipcouncil.org/directory-of-fellowships/ Accessed August 15, 2015.
ASMBS Fellowship Certificate. Available at: https://asmbs.org/professional-education/fellowship Accessed August 15, 2015.
Davis Jr SS, Husain FA, Lin E, et al. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216:96–104.
Raval MV, Wang X, Cohen ME, et al. The influence of resident involvement on surgical outcomes. J Am Coll Surg. 2011;212:889–98.
Englesbe MJ, Fan Z, Baser O, et al. Mortality in medicare patients undergoing surgery in July in teaching hospitals. Ann Surg. 2009;249:871–6.
Advani V, Ahad S, Gonczy C, et al. Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg. 2012;203:347–51.
Fahrner R, Turina M, Neuhaus V, et al. Laparoscopic cholecystectomy as a teaching operation: comparison of outcome between residents and attending surgeons in 1,747 patients. Langenbecks Arch Surg. 2012;397:103–10.
Hwang CS, Pagano CR, Wichterman KA, et al. Resident versus no resident: a single institutional study on operative complications, mortality, and cost. Surgery. 2008;144:339–44.
Kazaure HS, Roman SA, Sosa JA. The resident as surgeon: an analysis of ACS-NSQIP. J Surg Res. 2012;178:126–32.
Bhayani NH, Gupta A, Kurian AA, et al. Does fellow participation in laparoscopic Roux-en-Y gastric bypass affect perioperative outcomes? Surg Endosc. 2012;26:3442–8.
Krell RW, Birkmeyer NJ, Reames BN, et al. Effects of resident involvement on complication rates after laparoscopic gastric bypass. J Am Coll Surg. 2014;218:253–60.
Fanous M, Carlin A. Surgical resident participation in laparoscopic Roux-en-Y bypass: Is it safe? Surgery. 2012;152:21–5.
American College of Surgeons. User Guide for the 2013 ACS NSQIP Participant Use Data File (PUF). Available at: https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Accessed August 15, 2015.
Schauer P, Ikrammudin S, Hamad G, et al. The learning curve of laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc. 2003;17:212–5.
Higa KD, Boone KB, Ho T, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg. 2000;135:1029–34.
Khorgami Z, Andalib A, Corcelles R, et al. Recent national trends in the surgical treatment of obesity: sleeve gastrectomy dominates. Surg Obes Relat Dis. 2015;11:S6–8.
Fried GM, Feldman LS, Vassiliou MC, et al. Proving the value of simulation in laparoscopic surgery. Ann Surg. 2004;240:518–25.
Aminian A, Daigle CR, Romero-Talamás H, et al. Risk prediction of complications of metabolic syndrome before and 6 years after gastric bypass. Surg Obes Relat Dis. 2014;10:576–82.
Brethauer SA, Aminian A, Romero-Talamás H, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:628–36.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Informed consent is not applicable in this study.
Disclaimer
Since this study was performed using de-identified nationwide data, informed consent was not obtained for the purposes of this research. The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Rights and permissions
About this article
Cite this article
Aminian, A., Chaudhry, R.M., Khorgami, Z. et al. A Challenge between Trainee Education and Patient Safety: Does Fellow Participation Impact Postoperative Outcomes Following Bariatric Surgery?. OBES SURG 26, 1999–2005 (2016). https://doi.org/10.1007/s11695-016-2073-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2073-8