Abstract
Background
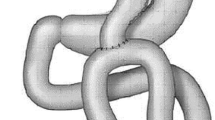
We started laparoscopic mini-gastric bypass (MGB) for the first time in India in February 2007 for its reported safety, efficacy, and easy reversibility.
Methods
A retrospective review of prospectively maintained data of all 1,054 consecutive patients (342 men and 712 women) who underwent MGB at our institute from February 2007 to January 2013 was done.
Results
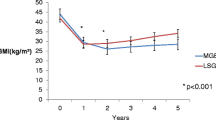
Mean age was 38.4 years, preoperative mean weight was 128.5 kg, mean BMI was 43.2 kg/m2, mean operating time was 52 ± 18.5 min, and mean hospital stay was 2.5 ± 1.3 days. There were 49 (4.6 %) early minor complications, 14 (1.3 %) major complications, and 2 leaks (0.2 %). In late complications, one patient had low albumin and one had excess weight loss; MGB was easily reversed in both (0.2 %). Marginal ulcers were noted in five patients (0.6 %) during follow-up for symptomatic dyspepsia, and anemia was the most frequent late complication occurring in 68 patients (7.6 %). Patient satisfaction was high, and mean excess weight loss was 84, 91, 88, 86, 87, and 85 % at years 1 to 6, respectively.
Conclusion
This study confirms previous publications showing that MGB is quite safe, with a short hospital stay and low risk of complications. It results in effective and sustained weight loss with high resolution of comorbidities and complications that are easily managed.



Similar content being viewed by others
References
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410–20.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4:353–7.
Hess DW, Hess DS. Laparoscopic vertical banded gastroplasty with complete transection of the staple line. Obes Surg. 1994;4:44–6.
Belachew M, Legrand M, Vincent V, et al. Laparoscopic placement of adjustable silicone gastric band in the treatment of morbid obesity: how to do it. Obes Surg. 1995;5:66–70.
Lee WJ, Lai IR, Huang MT, et al. Laparoscopic versus open vertical banded gastroplasty for the treatment of morbid obesity. Surg Laparosc Endosc. 2001;11:9–13.
Schauer P, Ikramuddin S. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232:515–29.
Fobi MA, Lee H, Felahy B, et al. Fifty consecutive patients with the GaBP ring system used in the banded gastric bypass operation for obesity with follow up of at least 1 year. Surg Obes Relat Dis. 2005;1(6):569–72.
Moszkowicz D, Arienzo R, Khettab I, et al. Sleeve gastrectomy severe complications: is it always a reasonable surgical option? Obes Surg. 2013;23(5):676–86.
Rutledge R. The mini-gastric bypass: experience with first 1,274 cases. Obes Surg. 2001;11:270–80.
Chevallier JM, Chakhtoura G, Zinzindohoué F. Laparoscopic mini-gastric bypass. J Chir (Paris). 2009;146(1):60–4.
Tacchino RM, Greco F, Matera D, et al. Single-incision laparoscopic gastric bypass for morbid obesity. Obes Surg. 2010;20(8):1154–60.
Lee WJ, Yu PJ, Wang W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity. Ann Surg. 2005;242:20–8.
Wang W, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15:648–54.
Noun R, Skaff J, Riachi E, et al. One thousand consecutive mini-gastric bypass: short and long-term outcome. Obes Surg. 2012;22(5):697–703.
Rutledge R, Walsh W. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8.
Lakdawala M, Bhasker A, Asian Consensus Meeting on Metabolic Surgery (ACMOMS). Report: Asian Consensus Meeting on Metabolic Surgery. Recommendations for the use of bariatric and gastrointestinal metabolic surgery for treatment of obesity and type II diabetes mellitus in the Asian population: August 9th and 10th, 2008, Trivandrum, India. Obes Surg. 2010;20(7):929–36.
Suter M, Calmes J, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16:829–35.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Griffen WO, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186:500–9.
Higa K, Boone K, Ho T, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity. Arch Surg. 2000;135:1029–34.
Lee W-J, Ser K-H, Lee Y-C, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–34.
Fisher BL, Buchwald H, Clark W, et al. Mini-gastric bypass controversy. Obes Surg. 2001;11(6):773–7.
Mahawar KK, Jennings N, Rown J, Gupta A, Balupuri S, Small PK. “Mini” gastric bypass :systematic review of a controversial procedure obesity. November 2013;23(11):1890–1898.
Gagner M, Deitel M, Erickson AL, et al. Fourth International Consensus Summit on sleeve gastrectomy. Obes Surg. 2013;23(12):2013–7.
Pontiroli AE, Laneri M, Veronelli A, et al. Biliary pancreatic diversion and laparoscopic adjustable gastric banding in morbid obesity: their long-term effects on metabolic syndrome and on cardiovascular parameters. Cardiovascular Diabetology. 2009;8:3.
Larrad-Jiménez Á, Sánchez-Cabezudo Díaz-Guerra C, de Cuadros Borrajo P, et al. Short-, mid- and long-term results of larrad biliopancreatic diversion. Obes Surg. 2007;17(2):202–10.
Theodore K. Alexandrides, George Skroubis, Fotis KalfarentzosResolution of diabetes mellitus and metabolic syndrome following Roux-en-Y gastric bypass and a variant of biliopancreatic diversion in patients with morbid obesity. Obes Surg. 2007;17(2):176–84.
Mason EF, Ito C. Gastric bypass in obesity. Surg Clin N Am. 1967;47:1345–52.
Conflict of Interest
All the contributing authors declare that they have no disclosures and no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kular, K.S., Manchanda, N. & Rutledge, R. A 6-Year Experience with 1,054 Mini-Gastric Bypasses—First Study from Indian Subcontinent. OBES SURG 24, 1430–1435 (2014). https://doi.org/10.1007/s11695-014-1220-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1220-3