Abstract
Background
There are no guidelines on ventilation modes in morbidly obese patients. We investigated the effects of volume-controlled (VCV) and pressure-controlled ventilation (PCV) on gas exchange, respiratory mechanics, and cardiovascular responses in laparoscopic gastric banding procedures.
Methods
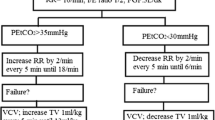
After Institutional Review Board approval, 24 adult consenting patients scheduled for laparoscopic gastric banding were studied. Anesthesia was standardized using remifentanil, propofol, rocuronium, and sevoflurane. All patients started with VCV with a tidal volume of 10 ml kg−1 ideal body weight, respiratory rate adjusted to obtain an end-tidal carbon dioxide of 35–40 mmHg, positive end-expiratory pressure of 5 cmH2O, an inspiratory pause of 10% and an inspiratory/expiratory ratio of 1:2. Fifteen minutes after pneumoperitoneum, the patients were randomly allocated to two groups. In Group VCV (n = 12), ventilation was with the same parameters. In Group PCV (n = 12), the airway pressure was set to provide a tidal volume of 10 ml kg−1 ideal body weight without exceeding 35 cm H2O. Respiratory rate was adjusted to keep an end-tidal carbon dioxide of 35–40 mmHg. Arterial blood samples were drawn after surgical positioning and 15 min after allocation. Analysis of variance (ANOVA) was used for statistical analysis.
Results
With constant minute ventilation, VCV generates equal airway pressures and cardiovascular effects with a lower PaCO2 as compared to PCV (42.5 (5.2) mmHg versus 48.9 (4.3) mmHg, p < 0.01 ANOVA). Arterial oxygenation remained unchanged.
Conclusions
VCV and PCV appear to be an equally suited ventilatory technique for laparoscopic procedures in morbidly obese patients. Carbon dioxide elimination is more efficient when using VCV.

Similar content being viewed by others
References
Clegg A, Colquitt J, Sidhu M, et al. Clinical and cost effectiveness of surgery for morbid obesity: a systematic review and economic evaluation. Int J Obes Relat Metab Disord. 2003;27:1167–77.
Mason EE. Surgery in the obese. Lancet. 2003;361:2001–2.
Pelosi P, Croci M, Ravagnan I, et al. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest. 1996;109:144–51.
Hedenstierna G, Santesson J. Breathing mechanics, dead space and gas exchange in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand. 1976;20:248–54.
Pelosi P, Ravagnan I, Giurati G, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91:1221–31.
Bardoczky GI, Yernault JC, Houben JJ, et al. Large tidal volume ventilation does not improve oxygenation in morbidly obese patients during anesthesia. Anesth Analg. 1995;81:385–8.
Sprung J, Whalley DG, Falcone T, et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg. 2003;97:268–74.
Jones K. Can the morbidly obese have the same “standard of care”? Anesth Analg. 2003;97:603; author reply 603–4.
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997;86:24–33.
Davis K Jr, Branson RD, Campbell RS, et al. Comparison of volume control and pressure control ventilation: is flow waveform the difference? J Trauma. 1996;41:808–14.
Campbell RS, Davis BR. Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care. 2002;47:416–24; discussion 424–6.
Cole AG, Weller SF, Sykes MK. Inverse ratio ventilation compared with PEEP in adult respiratory failure. Intensive Care Med. 1984;10:227–32.
Tharratt RS, Allen RP, Albertson TE. Pressure controlled inverse ratio ventilation in severe adult respiratory failure. Chest. 1988;94:755–62.
Gurevitch MJ, Van Dyke J, Young ES, et al. Improved oxygenation and lower peak airway pressure in severe adult respiratory distress syndrome. Treatment with inverse ratio ventilation. Chest. 1986;89:211–3.
Lessard MR, Guerot E, Lorino H, et al. Effects of pressure-controlled with different I:E ratios versus volume-controlled ventilation on respiratory mechanics, gas exchange, and hemodynamics in patients with adult respiratory distress syndrome. Anesthesiology. 1994;80:983–91.
Mancebo J, Vallverdu I, Bak E, et al. Volume-controlled ventilation and pressure-controlled inverse ratio ventilation: a comparison of their effects in ARDS patients. Monaldi Arch Chest Dis. 1994;49:201–7.
Mang H, Kacmarek RM, Ritz R, et al. Cardiorespiratory effects of volume- and pressure-controlled ventilation at various I/E ratios in an acute lung injury model. Am J Respir Crit Care Med. 1995;151:731–6.
Munoz J, Guerrero JE, Escalante JL, et al. Pressure-controlled ventilation versus controlled mechanical ventilation with decelerating inspiratory flow. Crit Care Med. 1993;21:1143–8.
Nyarwaya JB, Mazoit JX, Samii K. Are pulse oximetry and end-tidal carbon dioxide tension monitoring reliable during laparoscopic surgery? Anaesthesia. 1994;49:775–8.
Yamanaka MK, Sue DY. Comparison of arterial-end-tidal PCO2 difference and dead space/tidal volume ratio in respiratory failure. Chest. 1987;92:832–5.
Fleischmann E, Herbst F, Kugener A, et al. Mild hypercapnia increases subcutaneous and colonic oxygen tension in patients given 80% inspired oxygen during abdominal surgery. Anesthesiology. 2006;104:944–9.
Hager H, Reddy D, Mandadi G, et al. Hypercapnia improves tissue oxygenation in morbidly obese surgical patients. Anesth Analg. 2006;103:677–81.
Acknowledgement
This study was solely funded by institutional and departmental resources.
Author information
Authors and Affiliations
Corresponding author
Additional information
Performed at the University Hospital of Ghent, Department of Anesthesia, Gent Belgium.
Preliminary results of this study were presented as poster discussion at the Euroanaesthesia meeting 2005 in Vienna, Austria.
Rights and permissions
About this article
Cite this article
De Baerdemaeker, L.E.C., Van der Herten, C., Gillardin, J.M. et al. Comparison of Volume-controlled and Pressure-controlled Ventilation during Laparoscopic Gastric Banding in Morbidly Obese Patients. OBES SURG 18, 680–685 (2008). https://doi.org/10.1007/s11695-007-9376-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9376-8