Abstract
Background
Fractures of the coronoid process require adequate treatment, as otherwise they often lead to chronic instability and the development of rapidly progressive cubital osteoarthritis. Commonly, such patients are treated surgically; however, a defined fraction of patients might benefit from conservative treatment.
Methods
We systematically reviewed the available literature searching Medline using the PubMed interface. The primary objective was to determine indications, treatment protocols, and associated functional outcomes and complications of entirely conservatively treated fractures of the coronoid. The PRISMA guidelines were applied.
Results
We included five studies, all retrospective in design, with a total of 62 patients. For the indication of conservative treatment, joint congruency on imaging was a prerequisite in all studies. This was supplemented on most occasions by dynamic clinical examinations, with a focus on pain, range of motion, and adequate joint stability. Treatment protocols included close-meshed imaging, early functional mobilization, and some form of resting immobilization. Treatment success, defined as excellent or good results according to the Mayo Elbow Performance Score, was 95.1% at an average follow-up of 36 months. Six patients (9.7%) underwent surgical treatment during follow-up; 19 patients (30.6%) suffered complications that did not result in surgery.
Conclusion
The data of this work indicate that most patients achieve satisfactory results following conservative treatment of coronoid fractures caused by rotational moments. Concentric reduction of the joint, clinical exclusion of even mild subluxations, systematic early functional aftercare, and close radiographic monitoring appear to be mandatory requirements. The evidence remains scarce, and conclusions drawn from this review should be viewed with caution, as prospective randomized controlled trials are not available to date.
Level of evidence
IV, therapeutic
Zusammenfassung
Hintergrund
Frakturen des Koronoids bedürfen einer adäquaten Behandlung, da sie sonst zu chronischer Instabilität und der Entwicklung einer rasch fortschreitenden Kubitalarthrose führen können. In der Regel werden solche Patienten chirurgisch behandelt; ein bestimmter Anteil könnte jedoch von einer konservativen Behandlung profitieren.
Methodik
Die verfügbare Literatur wurde systematisch in der elektronischen Datenbank Medline über die PubMed-Oberfläche durchsucht. Primäres Ziel war es, Indikationen, Behandlungsprotokolle und damit verbundene funktionelle Ergebnisse und Komplikationen vollständig konservativ behandelter Frakturen des Koronoids zu identifizieren. Die Empfehlungen der PRISMA-Richtlinien (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) wurden angewandt.
Ergebnisse
Es wurden 5 Studien eingeschlossen, allesamt retrospektiv, mit insgesamt 62 Patienten. Voraussetzung für die Indikation zur konservativen Behandlung war in allen Studien über Bildgebung gesicherte Gelenkkongruenz. Diese wurde in den meisten Fällen durch dynamische klinische Untersuchungen ergänzt, wobei der Schwerpunkt auf Schmerzen, Bewegungsumfang und hinreichender Gelenkstabilität lag. Die Behandlungsprotokolle umfassten eine engmaschige Bildgebung, eine frühfunktionelle Mobilisierung und eine Form der Immobilisation in der Ruhephase. Der Behandlungserfolg, definiert als exzellente oder gute Ergebnisse nach dem Mayo Elbow Performance Score, betrug 95,1 %, bei einer durchschnittlichen Nachbeobachtungszeit von 36 Monaten. Im Verlauf des Follow-up wurden 6 Patienten (9,7 %) chirurgisch behandelt. Bei 19 Patienten (30,6 %) traten Komplikationen auf, die nicht zu einer Operation führten.
Schlussfolgerung
Die Daten dieser Arbeit zeigen, dass die meisten Patienten nach konservativer Behandlung von Koronoidfrakturen zufriedenstellende Ergebnisse erzielen. Die konzentrische Reposition des Gelenks, der klinische Ausschluss auch leichter Subluxationen, eine systematische frühfunktionelle Nachbehandlung und eine engmaschige röntgenologische Überwachung scheinen obligatorisch zu sein. Die Evidenzlage ist nach wie vor gering, und die Schlussfolgerungen dieser Arbeit sind mit Vorsicht zu betrachten, da bislang keine prospektiven randomisierten kontrollierten Studien verfügbar sind.
Evidenzlevel
IV, therapeutisch
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronoid process acts as an important anterior buttress in the elbow joint, preventing its posterior dislocation [4, 5, 15, 19]. Understanding the responsible pathomechanisms and clinically adequate treatment of bony coronoid fractures has become the center of biomechanical and clinical research during recent years [17]. The coronoid may be fractured both in combination with other bony lesions and in insolation. When considering coronoid fractures caused by rotational moments, two distinctive fracture morphologies may result, depending on the principal vector of the torque: Terrible triad injuries (TTI) are the mechanistic result of a rotational moment directed posterolaterally (PLRI; [3]). They comprise the triad of a radial head fracture, a coronoid fracture, and commonly a posterolateral elbow joint dislocation, resulting in a concomitant injury of the collateral ligaments in most cases [3]. The tip of the coronoid is usually affected, and the fracture line is often located far radially [12]. A varus posteromedial rotational injury mechanism (PMRI), however, leads to the associated fracture of the anteromedial facet (AMF) as a sole bony lesion [17]. The AMF is particularly vulnerable to fracture, with approximately 60% of its area not underpinned by the ulnar metaphysis [6]. Fractures of the coronoid’s base are commonly not amenable to conservative treatment. Depending on the size of the fragment, coronoid fractures may be severely unstable. This is also due to the frequent accompaniment of the lateral ulnar collateral ligament (LUCL; [7, 21, 22]). The medial collateral ligament (MCL) is also frequently avulsed [9, 18]. Concerning treatment, early adequate fracture management is essential, otherwise rotational instability may lead to rapidly progressive osteoarthritis (OA). However, this does not mean that adequate treatment must necessarily be surgical. There may be a general awareness among elbow surgeons that conservative treatment is possible in principle—but how this can occur, and which fraction of the entire patient pool is eligible, is the subject of this paper: A qualitative synthesis of possible indications, treatment protocols, functional outcomes, and associated risks has not been made to date.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were applied [14].
Inclusion criteria
Our search included:
-
1.
All study designs
-
2.
All levels of evidence
-
3.
Studies published in the English or German language
-
4.
Studies published since the beginning of the available literature
-
5.
Outcome data provided on conservatively treated coronoid fractures
Exclusion criteria
The search excluded:
-
1.
Cadaveric studies
-
2.
Biomechanical studies
-
3.
Anatomical descriptive studies
Search strategy
We searched Medline using the PubMed interface with the search terms and Boolean operators “(coronoid) AND (fracture) AND ((conservative) OR (nonoperative) OR (nonsurgically))”; the search was completed on 8 February 2022.
Study selection
The titles and abstracts of the retrieved studies were independently scanned by two reviewers (FL and TL). If necessary, the full text was checked for consistency with the inclusion criteria. In the case of disagreement, a third reviewer (LPM) was consulted to reach consensus.
Data extraction
The data of the publications suitable for inclusion were extracted into prefabricated tables, considering title, number of patients, mean age, mean follow-up, gender, fracture characteristics, indication prerequisites, conservative treatment protocol, range of motion (ROM), outcome scores, complications, and rates of conversion to operative treatment. The primary objective was to determine indications, treatment protocols, and associated functional outcomes and complications.
Results
Study selection
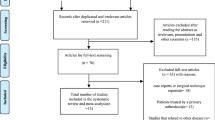
The initial search covered 56 publications. After the exclusion of abstracts not fitting the inclusion criteria, 12 full texts were assessed for eligibility. This decision-making process is shown in Fig. 1. Seven of these publications had to be excluded for reasons outlined in the PRISMA-adapted flow diagram. Insufficient outcome data refer to a purely narrative description of the outcome; insufficient individual data indicate that, based on the study data, it was not possible to relate the outcome to the conservatively treated patients exclusively. Thus, five articles were included [1, 2, 8, 16, 24].
Study characteristics
The basic information of the studies is summarized in Table 1. A total of 62 patients with an average age of 44 (17–76) years were enrolled. The average follow-up period was 36 (12–90) months, 61% of the patients were male. Three studies reported on isolated coronoid fractures; in the remaining two studies, the radial head was also involved in the sense of a TTI in all patients. Coronoid fractures have been inconsistently classified according to Regan–Morrey or the more recent O’Driscoll classification [17, 20]. In no case was a conservatively treated type 3 fracture (Regan–Morrey) or its O’Driscoll equivalent, a basal fracture of the coronoid, reported. If there was an additional fracture of the radial head, it was always classified according to Mason (Fig. 2; [13]).
Exemplary terrible triad injury treated conservatively at Cologne University Hospital. a Radial head fracture Mason type I, dislocation < 2 mm, joint step < 2 mm. b Tip fracture of the coronoid, no joint subluxation. c The transverse tip fracture of the coronoid runs far radially and does not involve the anteromedial facet
Indication algorithms
Indication algorithms in terms of the requirements of each study to be considered for a conservative treatment concept are listed in Table 2. Common to all studies was joint congruency on imaging, particularly humeroulnar congruency. In cases involving the radial head (TTI), the forearm rotation also factored into the indication [2, 16].
Treatment protocols
The different treatment concepts can be traced with reference to Table 3. Common to most studies is close radiological follow-up to detect clinical inapparent incongruities at an early stage, mobilization in the sense of timely functional aftercare, and a form of immobilization at rest and at night.
Functional outcomes and complications
Functional outcomes and complication are shown in Table 4. The average values for flexion and extension at the last follow-up appointment were 136° and 4°, respectively. The average values for pronation and supination at the last follow-up appointment were 76° and 79°, respectively. The MEPS averaged 94 points. In 44 patients the MEPS corresponded to an excellent result, in 15 patients to a good result, in two patients to a satisfactory result, and in one patient to a poor result. Defining excellent and good results using the MEPS as successful treatment, 95.1% of patients were treated successfully. The average DASH score was 7.3 points. Six patients (9.7%) required surgery during the follow-up period: in four cases due to stiffness (surgical arthrolysis) and in two cases due to recurrent instability. In total, 19 patients (30.6%) experienced complications, which, however, did not result in surgery.
Discussion
Fractures of the coronoid need to be treated adequately, otherwise they may lead to chronic instability with associated rapidly progressive osteoarthritis. The current literature indicates the standard procedure both for isolated fractures of the AMF and for TTI to be surgical; however, this is still debatable [2, 10, 16]. This systematic review demonstrates that conservative treatment of coronoid fractures caused by rotational moments (PLRI, TTI, PMRI, AMF fracture) is feasible given strict indication criteria and a clear treatment plan.
Overall, 62 patients with an average follow-up of 36 months and an average age of 44 years were included, 61% of whom were male. Of these patients, 41 had an isolated coronoid fracture, in 21 others the radial head was additionally fractured. The average MEPS was 94.1 points. A recent systematic review demonstrated that the mean MEPS of 114 surgically treated patients with isolated fractures of the AMF was 91.5 points [10]. Of course, the blunt comparison of the patient population considered in this study with that of surgically treated patients is impermissible, as the latter are usually highly unstable, do not have a congruent joint, and would therefore not be considered for primary conservative care. Accordingly, only a small fraction of patients with such fractures may be treated without surgery [23]. However, despite differences in the details of indication criteria and treatment protocols, the authors of the included studies generally seem to agree that concentric joint reduction and clinical exclusion of instability may be a prerequisite and, coupled with adequate early functional follow-up, may be the key to successful conservative treatment of coronoid fractures. Nevertheless, there is no consensus recommendation on how a concentric joint reduction should be defined: Is a joint step of < 2 mm to be considered concentric? How severe may the humeroulnar (especially TTI) or humeroradial (especially AMF fractures) gapping be? Early functional follow-up is often suggested as a fixed term, but by definition there is no binding guideline regarding the timeline that early functional follow-up can, may, and should be referred to. Most studies refer to mobilization within the first 14 days, and initial immobilization may often not be required because if instability has necessitated it, surgical treatment would be preferable [23]. In addition, early functional follow-up should be supplemented by close-meshed radiological monitoring to promptly detect instabilities that develop during treatment. Naturally, it would be desirable to provide a simple threshold value above which a fracture of the coronoid would necessarily require surgical treatment. However, this is challenging in practice due to the high interindividual variability of the coronoid anatomy, the thickness of the cartilage cover (the thicker the cartilage cover, the more likely it is to underestimate the actual stability-providing effect of a fracture fragment on CT), and the morphology and localization of the fracture line (fractures of the anteromedial facet cause greater instabilities than comparable fractures of the coronoid tip). A study conducted by Syed et al. had to be ruled out for inclusion due to the insufficient individual data on patients treated nonoperatively [23]. Nevertheless, the authors demonstrated that AMF fractures > 6.5 mm were clinically likely to be unstable and therefore frequently required surgical intervention [23]. This might serve as a guideline value. In case of doubt, it may be useful to give more weight to clinical examination than to diagnostic imaging in the decision-making process. If there is still uncertainty, remaining instabilities are expected to be more dramatic than a slight operative overtreatment—therefore, a high sensitivity (detecting all coronoid fractions requiring surgical intervention) should be preferred to a high specificity in case of doubt [23]. It should be noted that the clinical exclusion of instability in dynamic testing is not trivial. Chan et al. used fluoroscopic varus stress testing to detect PMRI [1]. Limiting factors include the patient’s pain in the acute situation, the variability of force application by the examiner, or the influence of interindividual muscle tension. In exceptional cases, subtype 3 fractures of the AMF—which involve the sublime tubercle, and thus the insertion site of the anterior bundle of the medial collateral ligament—may also be successfully treated conservatively, provided they are barely displaced, as shown for a patient in the study by Chan et al. [1] Likewise, in the study by Foruria et al., a patient with a subtype 3 fracture of the AMF was treated conservatively; however, no individual data are available regarding this patient, making it impossible to comment on the success of treatment in this individual case [8]. The evidence is too weak to make a statement here, but the involvement of the medial collateral ligament in combination with the fracture of the AMF should be considered critically and remain a case-by-case decision. Basal fractures of the coronoid are generally not considered for conservative therapy since they influence the statics of the elbow joint excessively. In TTI caused by a posterolateral rotational moment, the tip of the coronoid is usually involved, and the fracture line thus runs far radially in the frontal plane. Closkey et al. demonstrated that fractures of the coronoid tip involving less than 50% of the height of the coronoid have little biomechanical impact on elbow joint stability [4]. Thus, in most cases, the coronoid fracture is not the limiting factor; rather, it is the extent of rupture of both collateral ligaments and the morphology of the radial head fracture that matters. Therefore, to consider fully conservative therapy for TTI, an indication for surgery should be ruled out regarding the isolated radial head fracture. Mason type I fractures may generally be treated conservatively; for Mason type II fractures, treatment is critically debated, but a systematic review demonstrated that results of both treatment modalities, conservative and operative, are comparable [11].
During the follow-up period, six patients (9.7%) subsequently required surgical treatment. The indications were stiffness in four cases and instability in two cases. From these complications, the major area of conflict in the treatment of coronoid fractures becomes apparent: on the one hand, the danger of joint stiffening, and on the other hand, the at least equal danger of running into chronic instability. In total, there were 19 (30.6%) further complications, although these did not require surgical intervention. Among them, 18 arthritic changes, all classified as grade 1 according to Broberg and Morrey. Certainly, one major concern that this systematic review cannot answer is how these osteoarthritic changes affect elbow function in long-term follow-up. Based on these figures, however, surgical therapy might be beneficial, especially in young, active patients with high functional demands. An ulnar nerve neuropathy also remained untreated; not because there was no indication, however, but because the patient refused neurolysis and anterior transposition [16].
Limitations
Limitations of this work include the retrospective design of all studies included. Furthermore, the study represents a pure synthesis of the results after conservative coronoid fracture treatment and does not enable a comparison with a similar cohort of patients treated surgically. However, it should be noted once again that the patient population is different, and a direct comparison should therefore always be viewed critically. In the present work, not only isolated coronoid fractures were included, but also those caused by PLRI. This necessarily leads to the fracture of the radial head being yet another confounding factor. However, the aim of this work was merely to synthesize possible indication criteria for conservative therapy in the case of coronoid involvement. In so far as there is no definite indication for surgical treatment of the fracture of the radial head, the latter does not detract from conservative coronoid treatment. Nevertheless, this systematic review represents the first comprehensive synthesis on the conservative treatment of coronoid fractures caused by rotational moments.
Practical conclusion
-
The results of this work demonstrate that most patients achieve satisfactory results after treatment of conservative coronoid fracture due to rotational moments.
-
Concentric joint reduction, clinical and radiologic exclusion of even minor subluxations, systematic early functional follow-up, and close radiographic monitoring appear to be mandatory.
-
A rate of conversion to surgery of approximately 10% can be expected.
-
Approximately 30% of patients show mild osteoarthritis after an average follow-up of 3 years; the development of these alterations in the long-term follow-up remains pending.
-
The evidence is still scarce, and conclusions drawn from this review should be viewed with caution, since prospective randomized controlled trials are not available to date.
References
Chan K, Faber KJ, King GJW, Athwal GS (2016) Selected anteromedial coronoid fractures can be treated nonoperatively. J Shoulder Elbow Surg 25:1251–1257. https://doi.org/10.1016/j.jse.2016.02.025
Chan K, MacDermid JC, Faber KJ et al (2014) Can we treat select terrible triad injuries nonoperatively? Clin Orthop Relat Res 472:2092–2099. https://doi.org/10.1007/s11999-014-3518-9
Chen NC, Ring D (2015) Terrible triad injuries of the elbow. J Hand Surg Am 40:2297–2303. https://doi.org/10.1016/j.jhsa.2015.04.039
Closkey RF, Goode JR, Kirschenbaum D, Cody RP (2000) The role of the coronoid process in elbow stability: a biomechanical analysis of axial loading. J Bone Joint Surg Am 82:1749
Doornberg J, Ring D, Jupiter J (2004) Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin Orthop Relat Res 429:292–300. https://doi.org/10.1097/01.blo.0000142627.28396.cb
Doornberg JN, de Jong IM, Lindenhovius ALC, Ring D (2007) The anteromedial facet of the coronoid process of the ulna. J Shoulder Elbow Surg 16:667–670. https://doi.org/10.1016/j.jse.2007.03.013
Doornberg JN, Ring D (2006) Coronoid fracture patterns. J Hand Surg Am 31:45–52. https://doi.org/10.1016/j.jhsa.2005.08.014
Foruria AM, Gutiérrez B, Cobos J et al (2019) Most coronoid fractures and fracture-dislocations with no radial head involvement can be treated nonsurgically with elbow immobilization. J Shoulder Elbow Surg 28:1395–1405. https://doi.org/10.1016/j.jse.2019.01.005
Klug A, Buschbeck S, Gramlich Y et al (2019) Good outcome using anatomically pre-formed buttress plates for anteromedial facet fractures of the coronoid—a retrospective study of twenty-four patients. Int Orthop 43:2817–2824. https://doi.org/10.1007/s00264-019-04354-6
Lanzerath F, Hackl M, Wegmann K et al (2020) The treatment of anteromedial coronoid facet fractures: a systematic review. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2020.09.008
Lanzerath F, Hackl M, Wegmann K et al (2020) The treatment of isolated Mason type II radial head fractures: a systematic review. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2020.10.011
Lanzerath F, Seybold D, Müller LP (2021) Isolierte Koronoidfrakturen – Osteosynthese und ligamentäre Stabilisierung. In: Müller LP, Loew M (eds) Ellenbogen. Springer, Berlin, Heidelberg, pp 31–47
Mason ML (1954) Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 42:123–132. https://doi.org/10.1002/bjs.18004217203
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Morrey BF, An K‑N (2005) Stability of the elbow: osseous constraints. J Shoulder Elbow Surg 14:S174–S178. https://doi.org/10.1016/j.jse.2004.09.031
Najd Mazhar F, Jafari D, Mirzaei A (2017) Evaluation of functional outcome after nonsurgical management of terrible triad injuries of the elbow. J Shoulder Elbow Surg 26:1342–1347. https://doi.org/10.1016/j.jse.2017.05.012
O’Driscoll SW, Jupiter JB, Cohen MS et al (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52:113–134
Park S‑M, Lee JS, Jung JY et al (2015) How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O’Driscoll classification and ligament injury. J Shoulder Elbow Surg 24:74–82. https://doi.org/10.1016/j.jse.2014.07.010
Pollock JW, Brownhill J, Ferreira L et al (2009) The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am 91:1448–1458. https://doi.org/10.2106/JBJS.H.00222
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354
Ring D, Doornberg JN (2007) Fracture of the anteromedial facet of the coronoid process: surgical technique. J Bone Joint Surg Am 89:267–283. https://doi.org/10.2106/JBJS.G.00059
Sanchez-Sotelo J, O’Driscoll SW, Morrey BF (2005) Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow Surg 14:60–64. https://doi.org/10.1016/j.jse.2004.04.012
Syed H, Cameron P, Phadnis J (2021) Management of anteromedial coronoid fractures according to a protocol focused on instability assessment provides good outcomes with infrequent need for coronoid fixation. J Shoulder Elbow Surg 30:894–905. https://doi.org/10.1016/j.jse.2020.07.038
Van Der Werf HJ, Guitton TG, Ring D (2010) Non-operatively treated fractures of the anteromedial facet of the coronoid process: a report of six cases. Shoulder Elbow 2:40–42. https://doi.org/10.1111/j.1758-5740.2009.00044.x
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
The manuscript has been read and approved by all authors. Each author believes that the manuscript represents honest work.
Corresponding author
Ethics declarations
Conflict of interest
F. Lanzerath, M. Hackl, K. Wegmann, L.P. Müller and T. Leschinger declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lanzerath, F., Hackl, M., Wegmann, K. et al. Conservative treatment of fractures involving the coronoid process. Obere Extremität 17, 180–188 (2022). https://doi.org/10.1007/s11678-022-00692-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-022-00692-x