Abstract
Summary
This study reported the incidence of validated adult distal radius fractures in Oslo, Norway, in 2019. The incidence has been reduced over the last 20 years. However, it is still high compared to other regions in Norway and some of the other Nordic countries.
Purpose
We aimed to report the incidence of distal radius fractures in Oslo in 2019 and compare it to the incidence rates in 1998/1999.
Methods
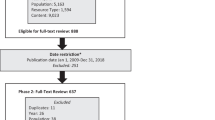
Patients aged ≥ 20 years resident in Oslo sustaining a distal radius fracture in 2019 were identified by electronic diagnosis registers, patient protocols, and/or radiology registers. The diagnosis was verified using medical records and/or radiology descriptions. We used the same method as the previous study from Oslo, making the comparison over time more accurate. The age-adjusted incidence rates and the age-standardized incidence rate ratio (IRR) were calculated.
Results
The absolute number of fractures decreased from 1490 in 1998/1999 to 1395 in 2019. The IRR for women and men in the age group ≥ 20 years in 2019 compared to 1998/1999 was 0.77 (95% CI 0.71–0.84) and 0.77 (95% CI 0.66–0.90), respectively. The IRR for women and men in the age group ≥ 50 years in 2019 compared to 1998/1999 was 0.78 (95% CI 0.71–0.86) and 0.78 (95% CI 0.63–0.97), respectively. For the population in Oslo with Asian background compared to Norwegian background in the age group ≥ 50 years, the IRR in 2019 was 0.57 (95% CI 0.40–0.80) for women and 0.77 (95% CI 0.44–1.37) for men.
Conclusions
The incidence of distal radius fractures in Oslo has decreased over the last 20 years. It is still, however, higher than in other areas of Norway and in some of the other Nordic countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fracture of the distal radius is the most frequent fracture in adults [1]. It is often the first fracture indicating osteoporosis in the middle aged and elderly and may be a warning of more fractures to come [2,3,4,5]. Distal radius fracture is an increasing economic burden to society due to an ageing population and more complex treatment [6,7,8,9]. For patients ≥ 50 years, the distal radius fracture may serve as a sentinel fracture for secondary fracture prevention. Fracture epidemiology may aid in allocating health recourses.
The incidence of distal radius fractures in Oslo, Norway, was studied in 1979 and in 1998/1999. There was no significant change in the incidence of adult distal radius fractures between 1979 and 1998/1999. However, the overall incidence of distal radius fractures in Oslo has been higher than in other European countries [10, 11]. There is little research on the incidence of distal radius fractures in developing countries, and the global variation in the incidence is difficult to interpret given methodological variations in sampling frames and fracture identification [12]. However, from Nordic countries that are similar to Norway, like Sweden, Finland, and Denmark, recent studies have demonstrated lower incidence than the previous studies from Oslo [13,14,15]. Similar results were found in a study from the neighboring county of Oslo, in 2011 [16].
The aim of this study was to investigate if there has been a change in the age-standardized incidence rate ratios (IRR) of distal radius fractures over the last two decades in women and men age ≥ 20 years in Oslo. We also studied the IRR in those ≥ 50 years and the IRR in one of the largest groups of immigrants in Oslo, people with Asian origin.
Materials and methods
Study population
We included patients sustaining a distal radius fracture between January 1 and December 31, 2019, aged ≥ 20 years and Oslo residents according to the National Population Register. Data on the “standard population” as well as immigration status were retrieved from Statistics Norway [17].
Variables
Distal radius fractures with or without a fracture of the distal part of ulna were included: the International Classification of Diseases 10th Revision (ICD-10)-codes S52.5, S52.6. Date of birth, gender, the patient’s geographical region of origin, date of first visit to a clinic with the fracture, and fracture side were recorded. A bilateral fracture was counted as two fractures. If a patient had two different distal radius fractures within the observation period, it was recorded as two fractures. If patients were seeking medical attention in an outpatient clinic and then referred to a hospital department for the same fracture, they were only recorded once. The patients’ geographical country of origin was defined as the person’s country of birth or the country of birth of the person’s parents or grandparents. Asian origin included all countries in Asia and Turkey.
Data collection and validation
The patient data were collected from the outpatient clinics and hospitals in Oslo treating distal radius fractures; Oslo University Hospital, Akershus University Hospital, Diakonhjemmet Hospital, and Volvat Medical Centre (the three hospitals are public, while Volvat is a private clinic). Patient administrative systems with electronic diagnosis registers at each hospital/clinic were used to identify all patients with the ICD-10 codes S52.X or S62.8 in the study period. At Volvat Medical Centre, the ICD-10 code M79.6 and the International Classification of Primary Care, 2nd edition (ICPC-2) – codes L74, L76, and L11 were used to identify the patients in addition to S52.X and S62.8 as Volvat used both systems. To verify the diagnosis of distal radius fracture, the clinical charts and radiology descriptions from all identified patients were retrieved. In ambiguous cases, the radiographs were examined by the first author. At the largest site, Oslo University Hospital’s, which treats the vast majority of the patients [11], lists of all patients with a radiograph or CT scan of the wrist or forearm in the period were used to identify additional patients not identified in the electronic diagnosis registers.
Ethics
The study was approved by Regional Committee for Medical and Health Research Ethics (REK 2018/2559) and by the Data Protection Officer at Oslo University Hospital (19/03873). A request to waive informed consent was approved.
Statistical analyses
Categorical data were analyzed using Fisher’s exact test and by the Pearson chi-square test. A p value < 0.05 was considered statistically significant. The age- and sex-specific incidence rates for 2019 were calculated and compared to 1998/1999 and 1979. The age-adjusted incidence rates in 2019 and 1998/1999 were calculated using a direct standardized method, and the 2019 Oslo population [17] was used as the standard population. Both the whole-year incidence and the summer incidence were reported to compare with the numbers from 1998/1999. The summer incidence was calculated using the fractures occurring in the 6 months from April to September and multiplied by two, giving a hypothetical number of fractures for a year without winter.
Within-stratum Mantel–Haenszel weights were used to find the age-standardized IRR with 95% confidence interval (CI) to compare the incidence rates between the different periods and different country of origin.
STATA SE (Version 17, Stata Inc. North Station, TX, USA) was used for all of the data analyses.
Results
In total, we identified 1395 distal radius fractures in patients ≥ 20 years of age in 2019 of which 995 (71%) fractures occurred in patients ≥ 50 years. There were 1372 patients as 11 patients had two different episodes with a distal radius fracture and 12 patients sustained bilateral fractures during the study period. There were 75% (n = 1048) women, and the median age was 62 for women (range 20–98) and 51 for men (range 20–95) (p < 0.001). There were 759 (54%) left-sided fractures, 612 (44%) right-sided fractures, and 12 were bilateral fractures. Ninety percent (n = 1247) of the patients were treated at the outpatient clinic at Oslo University Hospital, and 1136 (91%) were found to have a correct diagnosis code, while 111 (9%) were captured either by a control code or by the examination of radiology descriptions.
Total incidence and incidence in patients ≥ 50 years
The age-adjusted incidence rates per 10,000 observation years for women ≥ 20 years were 48.3 (95% CI 45.4–51.2) in 1998/1999 compared to 37.6 (95% CI 35.3–39.9) in 2019 with the corresponding figures in men being 17.0 (95% CI 15.1–18.8) in 1998/1999 and 13.3 (95% CI 11.9–14.7) in 2019 (Table 1). The age-standardized IRR for women and men in the age group ≥ 20 years in 2019 was 0.77 (95% CI 0.71–0.84) and 0.77 (95% CI 0.66–0.90) compared to 1998/1999. The total number of fractures was 1490 in 1998/1999 and 1395 in 2019.
In women, the incidence increased sharply from age 50 to 54 with a more moderate increase from age 60 to 64. In 1998/1999 [11], the exponential increase continued up to the 65 years group (Fig. 1). In men, the incidence increased almost linear by age, but except for the youngest, the incidence in each age group was lower compared to women (Fig. 2).
The age-adjusted incidence rates per 10,000 observation years for women ≥ 50 years were 101.9 (95% CI 95.0–108.8) in 1998/1999 compared to 80.4 (95% CI 74.9–85.9) in 2019 with the corresponding figures in men being 24.6 (95% CI 20.7–28.4) in 1998/1999 and 19.9 (95% CI 17.0–22.8) in 2019.
The age-standardized IRR for women and men in the age group ≥ 50 years in 2019 was 0.78 (95% CI 0.71–0.86) and 0.78 (95% CI 0.63–0.97) compared to 1998/1999.
Incidence in immigrants
The largest immigrant group from outside Europe is the people originating from Asia, representing 5% (n = 73) of the patients ≥ 20 years in 2019 compared to 3% (n = 40) in 1998/1999 (p = 0.001). Distal radius fractures in patients originating from Norway, i.e., born in Norway and both parents born in Norway represented 73% (n = 1020) in 2019 compared to 87% (n = 1302) in 1998/1999 (p < 0.001).
In both women and men, the age-adjusted incidence rates for the age group ≥ 50 years was lower in those originating from Asia compared to the majority population in Oslo (Table 2). In 2019, the age-standardized IRR of a distal radius fracture in the population in Oslo originating from Asia for the age group ≥ 50 years was 0.57 (95% CI 0.40–0.80) for women and 0.77 (95% CI 0.44–1.37) for men compared to the population in Oslo originating from Norway in the same age group. More than 99% of the patients ≥ 50 years with Asian origin included in our study were first-generation immigrants.
The age-adjusted incidence rates vary between the different groups of immigrants for the age group > 50 years in Oslo (Table 3).
Discussion
We found a decrease in the number of distal radius fractures in 2019 compared to 1998/1999. In both women and men, the age-standardized IRR was decreased by more than 20% in 2019 compared to 1998/1999 for all adults and for those over 50 years of age.
Comparison of incidence by region and country
For patients ≥ 50 years, we have compared the age-adjusted incidence rates with other Nordic countries and other Norwegian regions (Table 2).
Studies from Sweden [13] and Finland [14] showed a lower incidence in women. A study from Denmark back in 2010 showed a higher incidence in women than in Oslo in 2019 [15]. The incidence rate in Oslo’s neighboring county Akershus in a study from 2011 [16] was lower than in the present study. A study from the Southern part of Norway in 2004/2005 showed a slightly lower incidence in women, but not in men compared to Oslo in 2019 [18]. The incidence of distal radius fractures is higher in urban than in rural areas [19], and demographic differences between Oslo and other regions in Norway could have an impact here, since Oslo is a large city, and both Akershus and the Southern part of Norway consist of small cities, suburbs, and farmland. More women are living alone in Oslo than other places in Norway [17]. Living alone is linked to a higher incidence of fractures [20]. Slippery streets and less daylight during the winter contribute too many of the falls causing fracture [21]. Summer incidence could make a better comparison to other countries without the impact of snow and ice. The age-adjusted summer incidence for women and men in Oslo was found to be lower than the incidence during a whole year. The other Nordic countries also have winters with snow and ice though, so the high total incidence cannot be explained by these conditions only.
How can we explain the decreasing incidence?
There may be several reasons for the decrease in incidence. A contribution may be that the climate has been warmer and the winters have been shorter during the last 30 years [22].
A study looking at causes for the declining hip fracture incidence in Norway between 1999 and 2019 found that increased physical activity, reduced smoking, reduced use of benzodiazepine, and increased osteoporotic treatment were all parts of the explanation [23]. Most of these factors may also have contributed to the reduced incidence in distal radius fractures.
During the last 20 years, there has been an increased focus on osteoporosis and prevention on falls in the older age groups. Fracture Liaison Service, a nurse-driven program, where patients above 50 years of age with a fracture are offered screening for osteoporosis, was implemented at Oslo University Hospital in 2015 [24]. However, the distal radius fracture is often the first osteoporotic fracture in patients above 50 years of age, especially in women, so secondary fracture prevention may not have the same effect compared to other type of fractures since treatment seldom is given before the patient has a fracture [2].
In 2015, a program of preventing falls in the elderly was started in some of the districts of Oslo and has since expanded to almost all the districts [25]. Falls in the elderly are an important risk factor for fractures [26], and thus preventing falls could have an impact on the decreased incidence.
The elderly population is more active [17] and healthier than in earlier years, which could improve both bone mass and neuromuscular control. This could work both ways. Active elderly people with more neuromuscular control and faster walking speed have a higher risk of distal radius fracture than more fragile elderly who lack the reaction time to stretching out the hand to stop a fall or loss of balance. Fragile elderlies are more likely to land on their hip or shoulder [27, 28].
Some studies have shown that the incidence of other types of osteoporotic fractures such as ankle, hip, proximal humerus, and knee fractures in the elderly increased until the mid-90 s and then stabilized [29,30,31,32]. The prevention of falls and osteoporosis had not been widely implemented at that time, so there are other and largely unknown factors for this stabilization of the incidence.
Influence from immigration
The proportion of immigrants in Oslo from countries outside Europe and North America has increased from about 1% in 1979 to 13% in 1999 and up to 21% of the population in 2019 [17]. The largest group of these immigrants comes from Asia. In our study, people with Asian background ≥ 50 years had a lower incidence than people with Norwegian background. Thus, the increased number of people with different geographic region of origin in Oslo can contribute to the lower incidence in 2019 compared to 1998/1999. However, the incidence of the part of the population with Norwegian background was similar to the incidence of the total population in Oslo.
A recent study from Sweden showed that the rates of distal radius fractures of patients ≥ 20 years were marginally lower in immigrants of both first- and second-generation than native Swedes [33]. The rates of osteoporotic fractures in patients ≥ 50 years, however, were lower among first-generation immigrants compared to Swedish natives, while the rates in second-generation immigrants were similar [34, 35]. This could indicate that environmental factors contribute more to fragility fracture rates than ethnicity.
Strengths and limitations
This study has some limitations: We cannot be sure if or how many patients could potentially have received treatment from hospitals outside Oslo. However, we believe that most of these patients would have been registered during follow-up, since almost all patients with a distal radius fracture would need one or more follow-up appointments for new radiology and/or remove the cast. Another limitation is that we did not examine all the radiographs at Volvat Medical Centre, Diakonhjemmet, and Akershus University Hospital. However, supposing that an equal proportion of fractures were misclassified as at Oslo University Hospital, this would give us an increase in the total number of fractures by 13 from 1395 to 1408, which is around 1% of the total number. However, by including other diagnosis codes than S52.5 and S52.6, we believe we have reduced this problem.
A strength of this study is that we scrutinized the medical records to verify the fractures as well as all relevant radiographs and CT scans at Oslo University Hospital who treated 90% of the patients in our study. This means that very few fractures were lost due to wrong diagnoses. Many studies reporting incidence rates use electronic diagnosis registers as their only data source. This may lead to a lower reliability because it relies on the physicians to report the correct diagnosis. In our study, 9% of the patients with a distal radius fracture treated at Oslo University Hospital did not have the correct electronic diagnosis code (S52.5, S52.6). Using radiographic examinations and medical records in addition to electronic diagnosis codes to verify the diagnosis makes the incidence rates more reliable. In addition, we used the same method as the previous studies from Oslo [10, 11], making the comparison over the decades more accurate. This implies that our findings are real, and not an expression of lost data.
Conclusion
The incidence of distal radius fractures has decreased in Oslo over the last 20 years in all adults and more pronounced in those ≥ 50 years. The incidence in Oslo is still higher than in other regions of Norway and in some of the other Nordic countries.
Data availability
Due to protection of privacy under General Data Protection Regulation and Norwegian law, the individual-level data can only be made available after approval by the Regional Committee for Medical and Health Research Ethics.
References
Bergh C et al (2020) Fracture incidence in adults in relation to age and gender: a study of 27,169 fractures in the Swedish Fracture Register in a well-defined catchment area. PLoS ONE 15(12):e0244291
Ahmed LA et al (2013) Progressively increasing fracture risk with advancing age after initial incident fragility fracture: the Tromsø study. J Bone Miner Res 28(10):2214–2221
Morin SN et al (2021) Long-term risk of subsequent major osteoporotic fracture and hip fracture in men and women: a population-based observational study with a 25-year follow-up. Osteoporos Int 32(12):2525–2532
Johnson NA et al (2017) Risk of hip fracture following a wrist fracture-a meta-analysis. Injury 48(2):399–405
Crandall CJ et al (2015) Wrist fracture and risk of subsequent fracture: findings from the women’s health initiative study. J Bone Miner Res 30(11):2086–2095
Wilcke MK, Hammarberg H, Adolphson PY (2013) Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop 84(3):292–296
Mattila VM et al (2011) Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma 71(4):939–42 (discussion 942–3)
Hernlund E et al (2013) Osteoporosis in the European Union medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1):136
Hassellund S et al (2021) Surgical treatment is not cost-effective compared to nonoperative treatment for displaced distal radius fractures in patients 65 years and over. Bone Jt Open 2(12):1027–1034
Falch JA (1983) Epidemiology of fractures of the distal forearm in Oslo. Norway Acta Orthop Scand 54(2):291–295
Lofthus CM et al (2008) Epidemiology of distal forearm fractures in Oslo. Norway Osteoporos Int 19(6):781–786
MacIntyre NJ, Dewan N (2016) Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther 29(2):136–145
Ali M et al (2020) Incidence of distal radius fracture in a general population in southern Sweden in 2016 compared with 2001. Osteoporos Int 31(4):715–720
Flinkkilä T et al (2011) Epidemiology and seasonal variation of distal radius fractures in Oulu. Finland Osteoporos Int 22(8):2307–2312
Abrahamsen B, Jørgensen NR, Schwarz P (2015) Epidemiology of forearm fractures in adults in Denmark: national age- and gender-specific incidence rates, ratio of forearm to hip fractures, and extent of surgical fracture repair in inpatients and outpatients. Osteoporos Int 26(1):67–76
Solvang HW et al (2018) Epidemiology of distal radius fracture in Akershus, Norway, in 2010–2011. J Orthop Surg Res 13(1):199
Statistics Norway. Available from: www.ssb.no/en. Accessed 10 Apr 2024
Diamantopoulos AP et al (2012) The epidemiology of low- and high-energy distal radius fracture in middle-aged and elderly men and women in Southern Norway. PLoS ONE 7(8):e43367
Omsland TK et al (2011) More forearm fractures among urban than rural women: the NOREPOS study based on the Tromsø study and the HUNT study. J Bone Miner Res 26(4):850–856
Øyen J et al (2010) Low-energy distal radius fractures in middle-aged and elderly women-seasonal variations, prevalence of osteoporosis, and associates with fractures. Osteoporos Int 21(7):1247–1255
Al-Azzani W et al (2016) Epidemic of fractures during a period of snow and ice: has anything changed 33 years on? BMJ Open 6(9):e010582
The Norwegian Meteorological Institute. Available from: www.met.no/en. Accessed 10 Apr 2024
Kjeldgaard HK et al (2023) Explaining declining hip fracture rates in Norway: a population-based modelling study. Lancet Reg Health Eur 30:100643
Eisman JA et al (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046
Kommune O (2017) Pasientforløp etter fall og bruddskade. Available from: https://www.oslo.kommune.no/helse-og-omsorg/fag-og-kompetanse/samarbeidsutvalget/samhandlingsprosjekter-i-helsesektoren/pasientforlop-etter-fall-og-bruddskade/#gref. Accessed 10 Apr 2024
Aspray TJ, Hill TR (2019) Osteoporosis and the ageing skeleton. Subcell Biochem 91:453–476
Wu JC, Strickland CD, Chambers JS (2019) Wrist fractures and osteoporosis. Orthop Clin North Am 50(2):211–221
Vogt MT et al (2002) Distal radius fractures in older women: a 10-year follow-up study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc 50(1):97–103
Kannus P et al (2016) Declining incidence of fall-induced ankle fractures in elderly adults: Finnish statistics between 1970 and 2014. Arch Orthop Trauma Surg 136(9):1243–1246
Kannus P et al (2017) Stabilized incidence in proximal humeral fractures of elderly women: nationwide statistics from Finland in 1970–2015. J Gerontol A Biol Sci Med Sci 72(10):1390–1393
Kannus P et al (2016) Low-trauma knee fractures in older Finnish women between 1970 and 2013. Aging Clin Exp Res 28(4):665–668
Rosengren BE et al (2012) Secular trends in Swedish hip fractures 1987–2002: birth cohort and period effects. Epidemiology 23(4):623–630
Wändell P et al (2020) Distal forearm fractures in immigrant groups: a national Swedish study. Bone 138:115508
Wändell P et al (2021) Osteoporotic fractures among foreign-born individuals: a national Swedish study. Osteoporos Int 32(2):343–352
Wändell P et al (2021) Osteoporotic fractures in second-generation immigrants and Swedish natives. Osteoporos Int 32(7):1343–1350
Acknowledgements
Akershus University Hospital and Volvat Medical Centre for cooperation during collection of material for the article. Dr. Knut Melhuus and Dr. Martine Enger for making resources available at the Department of Orthopedic Emergency, Oslo University Hospital. Dr. Johan Hellund served as contact at the Department of Radiology and Nuclear Medicine, Oslo University Hospital. Raju Rimal at the University of Oslo for contributing with the statistics.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). Sophies Minde Ortopedi AS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oftebro, I., Skjaker, S.A., Fridheim, H.L. et al. Decrease in incidence of distal radius fractures in Oslo, Norway. Arch Osteoporos 19, 28 (2024). https://doi.org/10.1007/s11657-024-01383-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-024-01383-6