Abstract
Purpose
This study aimed to illustrate the possibility of an unfavorable response to treatment with the anabolic agent romosozumab for patients with severe osteoporosis and to discuss explanations for treatment failure.
Methods
Dual-energy x-ray absorptiometry (DXA) including vertebral fracture assessment (VFA) and X-rays of the thoracolumbar spine was used to assess bone mineral density (BMD) and the presence of vertebral fractures before and after treatment with romosozumab.
Results
Our patient developed a decrease in the BMD of the hip, two incident new vertebral fractures, and worsening of one prevalent vertebral fracture during 1 year treatment with romosozumab. We have not detected non-adherence, there was no pretreatment with anti-resorptives, and we observed no signs of secondary osteoporosis and/or comorbidities.
Conclusion
As the number of patients treated with romosozumab is rising, it becomes more likely that more patients will be found with new fractures and/or an unfavorable BMD response. Probably, the unfavorable response is a (bad) chance finding, but we think it is crucial for clinicians and patients to exclude nonadherence, new comorbidities and pretreatment with anti-resorptives as explanation in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An 83-year-old woman presented at the fracture liaison service of our outpatient clinic 3 months after a fracture of the distal radius following a fall from standing height. Her wrist fracture healed with conservative treatment. History revealed chronic back pain and a period of weight loss for which she had visited an internal medicine specialist, who did not find an explanation for that, based on, amongst other data, a CT-scan of the abdomen.
At additional questioning she reported her menarche at 15 years of age and her menopause around her 50th birthday. Dietary calcium intake was adequate and she used to exercise at a regular basis (tennis, walking, cycling) for at least 30 min a day. She never smoked, did not use alcohol, and her family history mentioned a first degree relative with a hip fracture (father, at 80 years of age who was diagnosed with bone cancer).
Her medical history included dyslipidemia and a vitamin B12 deficiency. She used omeprazole, rosuvastatin, and temporarily buprenorphine (transdermal) and oxazepam for her back pain.
At physical examination, her height was 159 cm (prior 168 cm), weight 55 kg (body mass index 21.8 kg/m2), and examination of her back showed a severe thoracolumbar scoliosis and thoracic kyphosis without local vertebral (pressure) pain. Examination of her heart, lungs, abdomen, and lymph nodes was normal.
A dual-energy x-ray absorptiometry (DXA) including vertebral fracture assessment (VFA) and X-rays of the thoracolumbar spine (due to difficult interpretation of VFA alone, as a result of the severe scoliosis and osteopenia) was conducted. They showed osteoporosis of the lumbar spine and total hip (T-scores, respectively, − 3.2 and − 3.1) (Table 1) and vertebral fractures (Th12 Genant grade 3, L1 Genant grade 1; Fig. 1) without signs of pathologic fractures. T-scores of fracture-free vertebrae L2, L3, and L4 were respectively − 3.8, − 4.1, and − 3.0.
X-rays of the thoracolumbar before and after treatment with romosozumab. Thoracic spine before (1a) and after (1b) treatment with romosozumab. Lumbar spine before (2a) and after (2b) treatment with romosozumab. Thoracolumbar scoliosis (3). * = fracture Th8. ° = fracture Th9. † = fracture Th12. ‡ = fracture L1. § = Fracture L4
Blood tests showed an erythrocyte sedimentation rate (ESR) of 17 mm/h (normal < 30), no monoclonal protein, normal blood count, kidney function, liver enzymes, alkaline phosphatase, HbA1c, calcium, phosphate, (para)thyroid hormone concentrations, celiac screen, 25-hydroxyvitamin-D, and B12. Carboxy-terminal collagen crosslinks (CTX, a marker for bone resorption) and procollagen type I N-terminal propeptide (P1NP, a marker for bone formation) were in the normal range for postmenopausal women (Table 1). Urinary calcium excretion was normal. Thus, no underlying secondary causes were identified.
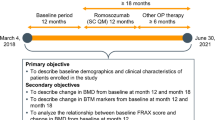
We concluded a high fracture risk in an 83-year-old lady with low bone mineral density (BMD) in the osteoporotic range and multiple fractures including vertebral fractures. Risk factors for the low BMD were her low body weight and her positive family history. Also, the use of proton pomp inhibitors might be related to lower BMD [1]. Further laboratory examination did not reveal secondary causes of the low BMD. Her 10-year probability for a major osteoporotic fracture was 45% and 38% for a hip fracture, calculated using Fracture Risk Assessment Tool (FRAX). Because of the very high fracture risk, the preferred treatment was an anabolic drug and she started treatment with romosozumab subcutaneous injections for 1 year [2].
During treatment with romosozumab, our patient did not experience any physical trauma, nor an episode of new backpain or other symptoms related to a possible secondary cause of her osteoporosis. Her height and weight remained stable. During evaluation after 1 year of treatment, our patient confirmed that she had taken her monthly (two) injections.
We evaluated the spine and BMD using both DXA, VFA and X-rays of the thoracolumbar spine. Unexpectedly, new vertebral fractures were present of the thoracic and lumbar spine (Th8 Genant grade 2, Th9 Genant grade 3, L4 Genant grade 1), increased collapse of fracture L1 (now Genant grade 2), and a stable fracture of Th12 (Genant grade 3) (Fig. 1). Moreover, we found a decrease in BMD of both the total hip (8.4%) and the femoral neck (4.8%) and a minimal increase of the BMD of the spine (2.2%) (Table 1). The imaging of the two lumbar spine measurements is more difficult to interpret, due to the severe thoracolumbar scoliosis of the patient, which might also have interfered with the measured bone area.
Repeated blood tests again showed no signs of a secondary cause, with an ESR of 16 mm/h (normal < 30), no monoclonal protein, normal blood count, kidney function, liver enzymes, alkaline phosphatase, calcium, phosphate, and (para)thyroid hormone concentrations.
Following completion of treatment with romosozumab, our patient was administered zoledronic acid in November 2022.
Discussion
We presented an 83-year-old women with a very high fracture risk who demonstrated a decrease in the BMD of the hip, incident new vertebral fractures, and worsening of prevalent vertebral fractures during romosozumab treatment.
This was highly unexpected based on previous results of romosozumab in RCTs. These demonstrate, on a group level, a large mean increase in BMD of the spine and of the hip, and a reduction in incidence of vertebral fractures, compared to placebo and alendronate as active comparators [3, 4].
The most important question is why did this patient not show the expected response to romosozumab regarding BMD and fracture prevention? There are several potential explanations:
-
1)
Non adherence to therapy. Although lack of adherence is quite common in the field of osteoporosis, not only with bisphosphonates but also with parenteral drugs [5], we have two arguments against this:
-
a)
patient confirms that she has used all her medication over 12 months and delivery of romosozumab was confirmed by the pharmacy. In The Netherlands, romosozumab is supplied by a central pharmacy (Apotheek Zorg) who is also responsible for patient instruction (done by trained nurses) and follow-up phone calls including motivational interviews every 3 months, to assess side-effects and adherence. Earlier, this has been shown to increase the two-year persistence in patients treated with teriparatide [6].
-
b)
the pattern of changes in bone markers, with an early rise after 2 months in P1NP and a decrease over time in CTX, reflect the changes observed in RCTs with romosozumab [3, 4].
-
a)
-
2)
Another illness or comorbidity during the 1-year treatment with romosozumab. We have seen the patient again after 12 months treatment with romosozumab at our outpatient clinic. Nor history nor physical examination nor the repeated laboratory tests revealed a new cause of secondary osteoporosis.
-
3)
Pretreatment with anti-resorptive osteoporotic drugs: it is well known that the effects of anabolic drugs, including romosozumab, can be blunted after pretreatment with anti-resorptives [7, 8]. However, this patient was not pre-treated with any antiresorptive drug.
-
4)
Misfortune, due to the combination of the high-risk for fracture patient profile and the fact that to date no anti-osteoporotic drug can provide 100% fracture reduction. In the ARCH and FRAME trial data at 12 months, the mean increase in BMD at the lumbar spine was 13.7% and 13.1%, respectively, and total hip 6.2% and 6.0% [3, 4]. However, in 1.1% of patients, romosozumab treatment did not result in an increase in BMD and 0.5–4% experienced a new vertebral fracture as our patient, with the highest percentage in high-risk for fracture patients in the ARCH trail [3, 4]. Of this patient subgroup, only half received fewer than six doses of romosozumab [4]. Real-world data from two Japanese cohort studies reported 3% and 5.7% of patients who suffered new fractures during treatment with romosozumab, of which 1.3% and 1.9% a vertebral fracture [9, 10]. A recent retrospective study regarding 92 romosozumab non-responder patients found an absent early rise in P1NP to be a predictor of nonresponse at month 12 [11]. Our patient however did show an early threefold rise in P1NP.
In our case, the first three explanations did not seem to contribute to the decrease in BMD of the hip and the development and worsening of vertebral fractures during treatment. The fourth explanation cannot be excluded as a contributor. Another point is the scoliosis; the vertebral fractures were difficult to score, but DXA measurement of the hips was reliable and detected unexpected bone loss.
To conclude, based on the data of this patient, non-adherence was unlikely, and we excluded new comorbidities and pretreatment with anti-resorptives. This suggests that our patient had back luck and was one of the small number of patients with new fractures and a decrease in BMD during romosozumab treatment. Since the number of patients treated with romosozumab is rising, due to chance, it becomes more likely that more patients will be found with new fractures and/or an unfavorable BMD response. However, it should be highlighted that it is crucial to exclude nonadherence, new comorbidities, and pretreatment with anti-resorptives as explanation in these patients.
References
Andersen BN, Johansen PB, Abrahamsen B (2016) Proton pump inhibitors and osteoporosis. Curr Opin Rheumatol 28:420–5
Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N et al (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M et al (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377(15):1417–1427
Cosman F, Crittenden DB, Ferrari S, Khan A, Lane NE et al (2018) FRAME study: the foundation effect of building bone with 1 year of romosozumab leads to continued lower fracture risk after transition to denosumab. J Bone Miner Res 33(7):1219–1226
Modi A, Sajjan S, Insinga R, Weaver J, Lewiecki EM et al (2017) Frequency of discontinuation of injectable osteoporosis therapies in US patients over 2 years. Osteoporos Int 28(4):1355–1363
Van Maren MA, Wyers CE, Driessen JHM, Visser JV, De Vries F et al (2019) Two-year persistence with teriparatide improved significantly after introduction of an educational and motivational support program. Osteoporos Int 30(9):1837–1844
Cosman F, Kendler DL, Langdahl BL, Leder BZ, Lewiecki EM et al (2022) Romosozumab and antiresorptive treatment: the importance of treatment sequence. Osteoporos Int 33(6):1243–1256
Ebina K, Etani Y, Tsuboi H, Nagayama Y, Kashii M et al (2022) Effects of prior osteoporosis treatment on the treatment response of romosozumab followed by denosumab in patients with postmenopausal osteoporosis. Osteoporos Int 33(8):1807–1813
Kobayakawa T, Suzuki T, Nakano M, Saito M, Miyazaki A et al (2021) Real-world effects and adverse events of romosozumab in Japanese osteoporotic patients: a prospective cohort study. Bone Rep 16(14):101068
Inose H, Ariga A, Motoyoshi T, Fukushima K, Tomizawa S et al (2022) The real-world effect of 12 months of romosozumab treatment on patients with osteoporosis with a high risk of fracture and factors predicting the rate of bone mass increase: a multicenter retrospective study. JBMR Plus 6(7):e10637
Tominaga A, Wada K, Okazaki K, Nishi H, Terayama Y et al (2023) Nonresponder considerations for romosozumab treatment. Calcif Tissue Int 113:157–165
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The corresponding author (AF Marsman) confirms on behalf of all authors that all three criteria of the authorship criteria and contributions were met.
Informed consent
Informed consent was obtained from the patient included in this case-report.
Conflict of interest
AF Marsman and BP Teunissen declare no conflict of interest. RT de Jongh has received speaker honorarium from Amgen and has a contract with Takeda as site principal investigator in a pharmacy-initiated study (SHP634-401). WF Lems has received speaker honoraria and is a member of advisory boards of Amgen, UCB, and Kyowa.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marsman, A.F., de Jongh, R.T., Teunissen, B.P. et al. Bone loss and new vertebral fractures during treatment with romosozumab: a case-report. Arch Osteoporos 19, 10 (2024). https://doi.org/10.1007/s11657-024-01367-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-024-01367-6