Abstract
Purpose
The purpose of this study was to investigate the morphological characteristics of the aortic valve and identify factors associated with the progression of aortic valve stenosis (AS) in osteoporosis patients.
Methods
In this single-center prospective cohort study, we recruited 10 patients (mean age: 75 ± 7 years, 90% female) who were taking anti-resorptive medicines at the outpatient clinic of University of Miyazaki Hospital, Japan. Baseline assessments, including transthoracic echocardiogram, blood sampling, and dual energy X-ray absorptiometry, were performed. Follow-up assessments were conducted at 6, 12, 18, and 24 months.
Results
During the 2-year follow-up, three patients with aortic valve peak flow velocity (AV PFV) ≥2 m/s at baseline developed moderate AS, which is defined as AV PFV ≥3 m/s. However, seven patients with AV PFV <2 m/s did not exhibit any progression of AS. There were significant variations in terms of bone mineral density, T-score values, and biomarkers associated with bone turnover (i.e., bone alkaline phosphatase, tartrate-resistance acid phosphatase-5b) among the enrolled patients, but none of these factors were found to be associated with the progression of AS. All patients exhibited low vitamin D status, with a median level of 16.1 ng/mL (25th percentile, 9.7 ng/mL; 75th percentile, 23 ng/mL). The baseline levels of AV PFV values were negatively correlated with 25-hydroxyvitamin D levels, determined by univariate linear regression analysis (beta coefficient = -0.756, 95% confidence interval, -0.136 ̶ -0.023, p = 0.011).
Conclusion
Our data suggest that low vitamin D status might be a potential risk factor for the progression of AS in osteoporosis patients undergoing treatment with anti-resorptive medicines.
Summary
Elderly patients with osteoporosis patients exhibited a subset of aortic valve stenosis. Our data suggest that the baseline aortic valve peak flow velocity predicts the progression of aortic valve stenosis, and there might be an association between the progression and the co-existing low vitamin D status in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative calcified aortic valve stenosis (AS) is the most prevalent form of valvular heart disease [1]. Its prevalence in the elderly population (>75 years) is reported to be 12.4% [1], and it increases with age, with an average prevalence rate of 0.2% in the 50–59-old cohort and 9.8% in the 80–89-year-old cohort [2]. The pathogenesis of AS suggests an active biological process characterized by the deposition of lipid into the intima cusps and subsequent lipid oxidation, which triggers an inflammatory response and exacerbates oxidative stress. This sets in motion a self-perpetuating cycle leading to progressive valve calcification [3,4,5].
Mild-to-moderate and severe AS have been incidentally observed in 26% (142/550) [6] and 3.2% (73/2274) [7] of patients with osteoporotic hip fractures, respectively. The imbalance between bone resorption and formation has been suggested to play a role in AS progression [8,9,10]. However, the effectiveness of pharmacological interventions targeting the osteogenic pathways in the time course of AS is yet to be proven [4, 11,12,13,14]. Low vitamin D status may have multiple adverse health consequences, such as skeletal fragility, muscle weakness, and effect on non-skeletal morbidities, including cardiovascular diseases [15, 16]. Based on this, we hypothesized that the progression of AS is associated with bone and mineral metabolism, and it may be influenced by the individual’s vitamin D status. We conducted a pilot study to investigate the temporal changes in aortic valve morphology and parameters related to bone and mineral metabolism. Additionally, our objective was to determine the factors associated with the progression of AS in osteoporosis patients who were receiving anti-resorptive medicines.
Methods
Study protocol
In this single-center prospective cohort study conducted at the outpatient clinic of University of Miyazaki Hospital, Japan between November 20, 2017, and March 31, 2020, the inclusion criteria were as follows: i) Japanese osteoporosis patients regardless of etiology, ii) age ≥50 years for both sexes, and iii) patients who were already taking or had recently started anti-resorptive therapy (bisphosphonate or denosumab). The exclusion criteria were: i) scheduled aortic valve replacement within 6 months, and ii) undergoing regular hemodialysis for end-stage renal disease. A total of 10 patients with osteoporosis were recruited by an orthopedist (T.F.), who was unaware of any prior diagnosis of valvular heart disease at the time of enrollment. Clinical history and medication details were obtained from the patients’ medical records. All patients underwent echocardiography, blood sampling, and dual energy X-ray absorptiometry (DXA) at baseline and at 6, 12, 18, and 24 months of follow-up. Hypertension was defined as having a systolic blood pressure of ≥140 mmHg, a diastolic blood pressure of ≥90 mmHg, or taking any antihypertensive medications. Diabetes mellitus was defined as having a fasting plasma glucose level of ≥126 mg/dL, a 2-hour postprandial glucose of ≥200 mg/dL, or taking any medication for diabetes mellitus. Dyslipidemia was defined as having a fasting plasma total cholesterol level of ≥220 mg/dL and/or triglyceride level of ≥150 mg/dL, or taking any medication for dyslipidemia. Blood pressure measurements were taken with the patient in a seated position at the hospital. Primary osteoporosis was diagnosed when no other disease-causing low mineral density, apart from osteoporosis, was observed, and the results of bone assessment met the required criteria [17]. Secondary osteoporosis was defined as the presence of low bone mass with accompanying endocrine disorders, such as hyperthyroidism, hyperparathyroidism, or diabetes mellitus; rheumatoid arthritis; or drug-induced osteoporosis caused by medications such as glucocorticoids, thyroid hormones, or hypogonadism-inducing agents [18]. The orthopedist (T.F.) routinely adjusted the type and dosage of osteoporosis drugs (Online Resource 1).
Laboratory measurements
Serum albumin, calcium, phosphate, and creatinine levels were immediately measured using a fully automated clinical chemistry analyzer (TBA-2000FR, Canon Medical Systems Corporation, Tochigi, Japan). For further analysis, serum/plasma was separated by centrifugation at 3,000 rpm for 20 minutes, frozen at −80 °C, and stored on-site without undergoing a freeze–thaw cycle. The following biomarkers were measured: brain natriuretic peptide (BNP) (CLIA, Abbott), which serves as a marker of heart failure; bone alkaline phosphatase (BAP) (CLEIA, Beckman Coulter, Inc), a marker of bone formation; tartrate resistance acid phosphatase (TRACP)-5b (EIA, NITTO BOSEKI Co., Ltd), a marker of bone resorption; fibroblast growth factor (FGF)-23 (C-terminal, Sandwich ELISA, Cat. No. Bl-20702, BIOMEDICA); intact parathyroid hormone (iPTH) (ECLIA, Roche Diagnostic); osteoprotegerin (OPG) (ELISA, Cat. No. K1011, Immunodiagnostik AG); receptor activator of nuclear factor kappa B ligand (RANKL) (free soluble, Sandwich ELISA, Cat. No. Bl-20462, BIOMEDICA); 25-hydroxyvitamin D [25(OH)D, Sandwich ELISA, Fujirebio Inc.]; and 1,25-dihydroxyvitamin D [1,25(OH)2D, radioimmunoassay, Immunodiagnostic Systems, Ltd.]. The estimated glomerular filtration rate (eGFR) was calculated using the following formula: eGFR (mL/min/1.73 m2) = 194 × (serum Cr)−1.094 × (age)−0.287 (× 0.739, when female) [19].
Echocardiography
All study echocardiograms were performed by dedicated ultra-sonographers using the following equipment: Aplio 400 (Canon Medical Systems, Tochigi, Japan), EPIQ7G (Philips Healthcare, Amsterdam, Netherland), and iE33 (Philips Healthcare, Amsterdam, Netherland). A standardized protocol, in accordance with international guidelines [20, 21], was used for the echocardiographic examinations. The left ventricular mass index was measured and indexed to the body surface area using the equation provided by Devereux et al. [22]. The antegrade systolic velocity across the aortic valve was measured using continuous-wave Doppler ultrasound [20]. The aortic valve area was assessed on two-dimensional echocardiograms using the continuity equation. The mean pressure gradient was calculated using pulse and continuous-wave Doppler assessment of the aortic valve. AS severity was categorized based on standard definitions for peak velocity (mild: 2.0–2.9 m/s, moderate: 3.0–3.9 m/s, severe: ≥4.0 m/s) or mean gradient (mild: <20 mm Hg, moderate: 20–39 mm Hg, severe: ≥40 mm Hg) [23].
DXA
DXA is the standard technique employed in clinical practice for measuring bone mineral density (BMD) in units of g/cm2, which is crucial for assessing fracture risk. Scans were obtained for the posterior–anterior lumbar spine (L2–L4) and hip, following the standard practice in Japan [24,25,26] and the guidelines [17]. BMD measurements were conducted using the Discovery A DXA system (Hologic, MA, USA). T-scores were calculated using young Japanese females as the reference population [17].
Endpoints
The primary endpoint of this study was to evaluate the morphological changes of the aortic valve, as assessed by AV PFV, mean pressure gradient, and aortic valve area index at the 24-month follow-up. The progression of AS was defined as a change in AS severity to moderate AS, indicated by a peak velocity greater than 3.0 m/s and a mean gradient higher than 20 mmHg. In cases where a patient did not attend the 24-month visit, either the 12- or 18- month visit was used as the final visit for analysis. The secondary endpoint aimed to explore the parameters associated with the progression of AS.
Statistical analyses
All statistical analyses were performed using SPSS software, version 29 (IBM Corp., Armonk, NY, USA). Data were presented as means ± standard deviations for continuous variables, and as medians with interquartile range (Q1 ̶ Q3). Categorical variables were expressed as the number of patients. Spaghetti graphs were used to visualize the measurements of baseline, 6-, 12-, 18-, and 24-month follow-up for each patient. Furthermore, univariate linear regression analysis was conducted to examine the association between 25(OH)D levels and AV PFV values at baseline. The coefficient (β) and 95% confidence interval (CI) were calculated. A p-value <0.05 was statistically significant.
Results
Patients’ characteristics
The baseline characteristics of the patients are presented in Table 1. Among the ten patients, nine were menopausal women. Eight patients had comorbidities, with hypertension being the most prevalent disorder (6/10, 60%). Eight patients were using bisphosphonates, while two were using denosumab as anti-resorptive therapy. At baseline, seven patients were using activated vitamin D3 analogs (6 with eldecalcitol and 1 with alfacalcidol) in combination with bisphosphonates (see Online Resource 1). Two patients received native vitamin D and calcium supplement when administered denosumab [27]. Daily calcium intake was not assessed. The laboratory and DXA results at baseline are listed in Table 2. All patients exhibited low vitamin D status, with plasma 25(OH)D levels below 30 ng/mL, and 6 of them had levels below 20 ng/mL. Four patients had a T-score of ≤-2.5 at the lumbar spine, two at the total hip, and two at the femoral neck. The main echocardiographic values at baseline are presented in Table 3. All patients had a tricuspid aortic valve, and mitral valve calcification was not observed in any patient. The left ventricular ejection fraction was preserved.
Primary endpoint
Figure 1 presents spaghetti graphs illustrating the individual values of AV PFV (A), mean pressure gradient (B), aortic valve area index (C), and left ventricular ejection fraction (D) over the 24-month follow-up period. At baseline, 7 cases had AV PFV <2.0 m/s, while 3 cases had ≥2.0 m/s (n = 2 with mild AS; n = 1 with moderate AS). The cases with AV PFV ≥2 m/s developed moderate AS. Absolute change in AV PFV (m/s) during the first 12 months of follow-up was 0.44, 0.44, and 0.18 for cases 1, 4, and 7, respectively. Over the 24 months of follow-up, these values were 0.11, 0.70, and 0.43 for the same cases, respectively. Case 1 exhibited the highest AV PFV and mean pressure gradient, and the lowest aortic valve area, and ultimately a reduction in left ventricular ejection fraction from 68% to 50% during the course of follow-up. Among the seven cases with AV PFV <2 m/s at baseline, no progression of AS was observed.
Spaghetti graphs displaying the changes in aortic valve peak flow velocity (AV PFV) (A), mean pressure gradient (PG) (B), aortic valve area index (AVAI) (C), and left ventricular ejection fraction (LVEF) (D) over the 24-month follow-up period in 10 osteoporosis patients. In the figure, case 1 is represented by a red circle and line, case 4 by a blue circle and line, and case 7 by a green triangle and line
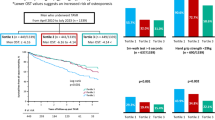
Secondary endpoint
Figure 2 presents spaghetti graphs displaying individual values of BNP (A), eGFR (B), BAP (C), TRACP-5b (D), albumin-corrected calcium (E), phosphate (F), FGF-23 (G), iPTH (H), 25(OH)D (I), and 1,25(OH)2D (J) over the 24-month follow-up period. There were significant variations in terms of AS progression and biomarkers associated with bone turnover among the enrolled patients. Case 1 experienced overt heart failure accompanied by an elevation in BNP levels during the observation periods. This patient exhibited increased FGF-23 levels, followed by elevations in BAP and TRACP-5b levels after switching to daily teriparatide administration. Meanwhile, the plasma 25(OH)D levels consistently decreased over the 24-month period. Figure 3 demonstrates a negative relationship between plasma 25(OH)D levels and AV PFV values at baseline, indicating that higher AV PFV values were associated with decreased plasma 25(OH)D levels (β = -0.756, 95% CI, -0.136 ̶ -0.023, p = 0.011).
Spaghetti graphs depicting the changes in brain natriuretic peptide (BNP) (A), estimated glomerular filtration rate (eGFR) (B), bone alkaline phosphatase (BAP) (C), tartrate resistance acid phosphatase (TRACP)-5b (D), albumin-corrected calcium (E), phosphate (F), fibroblast growth factor (FGF)-23 (G), intact parathyroid hormone (iPTH) (H), 25-hydroxyvitamin D (25(OH)D) (I), and 1,25-dihydroxyvimatin D (1,25(OH)2D) (J) over the 24-month follow-up period in 10 osteoporosis patients. In the figure, case 1 is represented by a red circle and line, case 4 by a blue circle and line, and case 7 by a green triangle and line. The clinical events of case 1 are indicated at the specified time in panel A
Discussion
This exploratory study provides the first-time demonstration of the temporal changes in aortic valve morphology and parameters of bone and mineral metabolism in osteoporosis patients receiving anti-resorptive therapy such as bisphosphonates or desunomab. Our data provide support for the notion that the pre-existing aortic valve calcification is a predisposing factor for the progression of AS [28, 29]. Additionally, our findings suggest a potential association between low vitamin D status and aortic valve progression. Mineralization plays a central role in the progression of aortic valve calcification at some point [4, 14]. In this study, measurements of BMD, T-score values, BNP, BAP, TRACP-5b, FGF-23, RANKL, OPG, or 1,25(OH)2D levels were found to be insensitive in terms of predicting the progression of AS over the 24-month follow-up period (data not shown). Low vitamin D status contributes to bone loss by stimulating PTH production [30]. 25(OH)D levels are measured to assess vitamin D status adequacy [31]. In this study, all patients included exhibited low vitamin D status. Importantly, the severity of AS, as assessed by AV PFV, could be predicted by the levels of 25(OH)D at baseline. Deficient levels of vitamin D have been implicated in stimulating pro-inflammatory factors and pathways, promoting osteogenic differentiation, and enhancing metalloproteinase activity, ultimately leading to vascular calcification [32]. It is postulated that co-existing vitamin D status may determine the extent of aortic valve calcification. The serum level of 1,25(OH)2D is tightly regulated by PTH, and it reflects both endogenous production and the effect of activated vitamin D3 analogs in this study [16, 33]. The relationship between serum calcium levels and the progression of AS has not been conclusively established [34, 35]. However, calcium supplementation, with or without native vitamin D, has been associated with a higher incidence of future aortic valve replacement in elderly patients with mild to moderate AS [35]. Among the patients in this study, one out of three (case 7) who were taking activated vitamin D3 analog experienced AS progression along with an increase in serum calcium levels exceeding 10.5 mg/dL [36]. The decreased iPTH levels and increased 1,25(OH)2D levels suggest excessive administration of activated vitamin D3 analog. Further research is needed to determine whether activated vitamin D3 analogs have an additive risk in AS progression. The natural history of AS typically involves a prolonged asymptomatic period, but symptoms develop, initially presenting as exertional dyspnea, and progressing to heart failure [4]. The elevated levels of BNP and FGF-23 suggest a potential link between osteoporosis and the worsening of heart failure [37, 38]. Furthermore, FGF-23, derived from osteocytes, has been shown to have effects on the deterioration of left ventricular function and the acceleration of valvular calcification [39, 40]. The current report raises the possibility that assessment of aortic valve morphology and circulating 25(OH)D should be performed prior to initiation of osteoporosis treatment. It is plausible that clinicians should consider that osteoporosis patients with mild to moderate AS may experience further progression when they have low vitamin D status. This information can help personalize the follow-up period of echocardiogram and aid in determining the need for valve intervention.
This study has several limitations. Firstly, the sample size was very small, and this may limit the generalizability of the findings. Additionally, there is a possibility of selection bias, which could have influenced the prevalence of AS in the study population. The assessment of AS severity relied on echocardiography, which is subjected to measurement errors, and hemodynamic parameters such as peak velocity, mean pressure gradient, aortic valve area can be influenced by factors like left ventricular function, aortic compliance, and presence of hypertension [41, 42]. Another limitation is that we did not measure bone remodeling markers such as carboxyterminal cross-linked telopeptide type 1 collagen and N-terminal propeptide of type 1 procollagen in this study [43]. Furthermore, the potential contribution of genetic predisposition, such as variation in the vitamin D receptor genotype [44], and variation in response to activated vitamin D3 analogs [45], warrant further investigation in relation with AS progression. It is also important to note that the impact of the duration of low vitamin D status prior to enrollment on the progression of valvular calcification remained to be determined. However, it is plausible that sustained low vitamin D status may have contributed to the progression of AS, and investigating whether vitamin D status can be modified as a risk factor presents a challenge.
In conclusion, our findings indicate that low vitamin D status might be a potential risk factor for AS progression.
Data availability
The original contributions presented in the study are included in the article/supplementary materials. Further inquiries can be directed to the corresponding author.
References
Osnabrugge RLJ, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, LeReun CM, Bogers AJJC, Piazza N, Kappetein AP (2013) Aortic Stenosis in the Elderly: Disease Prevalence and Number of Candidates for Transcatheter Aortic Valve Replacement: A Meta-Analysis and Modeling Study. Journal of the American College of Cardiology 62:1002–1012
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K (2013) The evolving epidemiology of valvular aortic stenosis. the Tromsø study. Heart 99:396–400
Marquis-Gravel G, Redfors B, Leon MB, Généreux P (2016) Medical Treatment of Aortic Stenosis. Circulation 134:1766–1784
Otto CM, Prendergast B (2014) Aortic-valve stenosis--from patients at risk to severe valve obstruction. N Engl J Med 371:744–756
Pawade TA, Newby DE, Dweck MR (2015) Calcification in Aortic Stenosis: The Skeleton Key. J Am Coll Cardiol 66:561–577
Furugen M, Watanabe N, Nishino S, Kimura T, Ashikaga K, Kuriyama N, Shibata Y (2021) Impact of osteogenic activity on degenerative aortic valve disease in patients with osteoporotic hip fracture. J Cardiol 78:423–430
Rostagno C, Cartei A, Rubbieri G, Ceccofiglio A, Civinini R, Curcio M, Polidori G, Boccaccini A (2022) Hip Fracture Surgery in Severe Aortic Stenosis: A Study of Factors Affecting Mortality. Clin Interv Aging 17:1163–1171
Hekimian G, Boutten A, Flamant M et al (2013) Progression of aortic valve stenosis is associated with bone remodelling and secondary hyperparathyroidism in elderly patients—the COFRASA study. European Heart Journal 34:1915–1922
Cannata-Andia JB, Roman-Garcia P, Hruska K (2011) The connections between vascular calcification and bone health. Nephrol Dial Transplant. England, pp 3429–3436
Massera D, Buzkova P, Bortnick AE, Owens DS, Mao S, Li D, De Boer IH, Kestenbaum BR, Budoff MJ, Kizer JR (2021) Bone mineral density and long-term progression of aortic valve and mitral annular calcification: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis 335:126–134
Pawade TA, Doris MK, Bing R et al (2021) Effect of Denosumab or Alendronic Acid on the Progression of Aortic Stenosis: A Double-Blind Randomized Controlled Trial. Circulation 143:2418–2427
Aksoy O, Cam A, Goel SS et al (2012) Do Bisphosphonates Slow the Progression of Aortic Stenosis? Journal of the American College of Cardiology 59:1452–1459
Diederichsen ACP, Lindholt JS, Möller S et al (2022) Vitamin K2 and D in Patients With Aortic Valve Calcification: A Randomized Double-Blinded Clinical Trial. Circulation 145:1387–1397
Alushi B, Curini L, Christopher MR, Grubitzch H, Landmesser U, Amedei A, Lauten A (2020) Calcific Aortic Valve Disease-Natural History and Future Therapeutic Strategies. Front Pharmacol 11:685
Binkley N, Krueger D (2008) Evaluation and correction of low vitamin D status. Curr Osteoporos Rep 6:95–99
Thacher TD, Clarke BL (2011) Vitamin D insufficiency. Mayo Clin Proc 86:50–60
Soen S, Fukunaga M, Sugimoto T et al (2013) Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 31:247–257
Mirza F, Canalis E (2015) Management of endocrine disease: Secondary osteoporosis: pathophysiology and management. Eur J Endocrinol 173:R131–R151
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Baumgartner H, Hung J, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, Lancellotti P, LeFevre M, Miller F, Otto CM (2017) Recommendations on the Echocardiographic Assessment of Aortic Valve Stenosis: A Focused Update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Journal of the American Society of Echocardiography 30:372–392
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC, Horton K, Ogunyankin KO, Palma RA, Velazquez EJ (2019) Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. Journal of the American Society of Echocardiography 32:1–64
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Otto CM, Nishimura RA, Bonow RO et al (2021) 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 77:e25–e197
Fujita Y, Iki M, Tamaki J et al (2012) Association between vitamin K intake from fermented soybeans, natto, and bone mineral density in elderly Japanese men: the Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) study. Osteoporos Int 23:705–714
Sugimoto T, Yoshimura T, Uzawa T (2021) Efficacy of once-weekly and twice-weekly injections of teriparatide by patient characteristics: A post hoc analysis of the TWICE study. Osteoporosis and Sarcopenia 7:11–16
Mori Y, Izumiyama T, Baba K, Mori N, Fujii H, Ishii T, Itoi E (2020) Evaluation of risk factors of vertebral fracture in Japanese female patients with glucocorticoid-induced osteoporosis. Journal of Orthopaedic Surgery and Research 15:290
Nakamura Y, Suzuki T, Kamimura M, Murakami K, Ikegami S, Uchiyama S, Kato H (2017) Vitamin D and calcium are required at the time of denosumab administration during osteoporosis treatment. Bone Res 5:17021
Nayeri A, Xu M, Farber-Eger E, Blair M, Saini I, Shamsa K, Fonarow G, Horwich T, Wells QS (2020) Initial changes in peak aortic jet velocity and mean gradient predict progression to severe aortic stenosis. Int J Cardiol Heart Vasc 30:100592
Willner N, Prosperi-Porta G, Lau L et al (2023) Aortic Stenosis Progression: A Systematic Review and Meta-Analysis. JACC Cardiovasc Imaging 16:314–328
Sai AJ, Walters RW, Fang X, Gallagher JC (2011) Relationship between vitamin D, parathyroid hormone, and bone health. J Clin Endocrinol Metab 96:E436–E446
Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GEH, Josse RG, Lips P, Morales-Torres J, Yoshimura N (2010) IOF position statement: vitamin D recommendations for older adults. Osteoporosis International 21:1151–1154
Wang J, Zhou JJ, Robertson GR, Lee VW (2018) Vitamin D in vascular calcification: a double-edged sword? Nutrients 10:652
Jiang Y, Tang H, Ma X et al (2019) Eldecalcitol increases bone mineral density in Chinese osteoporotic patients without vitamin D or calcium supplementation. Journal of Bone and Mineral Metabolism 37:1036–1047
Hisamatsu T, Miura K, Fujiyoshi A, Kadota A, Miyagawa N, Satoh A, Zaid M, Yamamoto T, Horie M, Ueshima H (2018) Serum magnesium, phosphorus, and calcium levels and subclinical calcific aortic valve disease: A population-based study. Atherosclerosis 273:145–152
Kassis N, Hariri EH, Karrthik AK et al (2022) Supplemental calcium and vitamin D and long-term mortality in aortic stenosis. Heart 108:964
Tonon CR, Silva TAAL, Pereira FWL et al (2022) A Review of Current Clinical Concepts in the Pathophysiology, Etiology, Diagnosis, and Management of Hypercalcemia. Med Sci Monit 28:e935821
Katano S, Yano T, Tsukada T et al (2020) Clinical Risk Factors and Prognostic Impact of Osteoporosis in Patients With Chronic Heart Failure. Circ J 84:2224–2234
Koller L, Kleber ME, Brandenburg VM et al (2015) Fibroblast Growth Factor 23 Is an Independent and Specific Predictor of Mortality in Patients With Heart Failure and Reduced Ejection Fraction. Circ Heart Fail 8:1059–1067
Leifheit-Nestler M, Haffner D (2018) Paracrine Effects of FGF23 on the Heart. Front Endocrinol (Lausanne) 9:278
Yamada S, Giachelli CM (2017) Vascular calcification in CKD-MBD: Roles for phosphate, FGF23, and Klotho. Bone 100:87–93
Lindman BR, Sukul D, Dweck MR et al (2021) Evaluating Medical Therapy for Calcific Aortic Stenosis: JACC State-of-the-Art Review. Journal of the American College of Cardiology 78:2354–2376
Saikrishnan N, Kumar G, Sawaya FJ, Lerakis S, Yoganathan AP (2014) Accurate assessment of aortic stenosis: a review of diagnostic modalities and hemodynamics. Circulation 129:244–253
Shetty S, Kapoor N, Bondu JD, Thomas N, Paul TV (2016) Bone turnover markers: Emerging tool in the management of osteoporosis. Indian J Endocrinol Metab 20:846–852
Ortlepp JR, Hoffmann R, Ohme F, Lauscher J, Bleckmann F, Hanrath P (2001) The vitamin D receptor genotype predisposes to the development of calcific aortic valve stenosis. Heart 85:635–638
Ammar M, Heni S, Tira MS, Khalij Y, Hamdouni H, Amor D, Ksibi S, Omezzine A, Bouslama A (2022) Variability in response to vitamin D supplementation according to vitamin D metabolism related gene polymorphisms in healthy adults. Eur J Clin Nutr 1–6
Association WM (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Acknowledgments
The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
This study was supported by grants-in-aid for Scientific Research (C) (22K08128 to T.T.) from the Japan Society for the Promotion of Science, and Clinical Research from the University of Miyazaki Hospital.
Author information
Authors and Affiliations
Contributions
TT and TF designed the study and edited the manuscript. TF collected the data, and TT analyzed the data and performed the statistical analysis. YY, EC, MN and KK edited and provided critical revisions to the article. TT was primarily responsible for the manuscript’s final content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Toshihiro Tsuruda, Taro Funamoto, Chiyoko Suzuki, Yoshimasa Yamamura, Michikazu Nakai, Etsuo Chosa, and Koichi Kaikita declare that they have no conflict of interest.
Ethical approval
The study protocol conformed to the guidelines stipulated in Declaration of Helsinki [46] and was approved by the Human Investigation Review Committee of the University of Miyazaki (permission number 0-0207).
Informed consent
Written informed consent was obtained from each patient.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PPTX 46 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsuruda, T., Funamoto, T., Suzuki, C. et al. Increasing baseline aortic valve peak flow velocity is associated with progression of aortic valve stenosis in osteoporosis patients—a possible link to low vitamin D status. Arch Osteoporos 18, 129 (2023). https://doi.org/10.1007/s11657-023-01339-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01339-2