Abstract
Summary
The efficacy of generic teriparatide in improving BMD at lumbar spine in patients with osteoporosis was similar to that of alendronate. It provided a new choice for osteoporosis treatment in Chinese population.
Introduction
To determine whether the efficacy of generic teriparatide is noninferior to alendronate for Chinese postmenopausal women with osteoporosis.
Methods
Eligible patients were randomly assigned (2:1) in a 48-week, open-label design to receive 20 µg sc daily teriparatide or 70 mg oral weekly alendronate. Primary outcome was percentage change in BMD at the lumbar spine from baseline to 48 weeks and was assessed for non-inferiority. The same outcome was further assessed for superiority as a secondary endpoint.
Results
Three hundred ninety-one and 196 participants were randomly assigned to the teriparatide or alendronate group, of whom 379 and 194 receiving at least one dose of teriparatide and alendronate treatment were eligible for the efficacy analysis. Teriparatide was non-inferior to alendronate for BMD change at lumbar spine (treatment difference: 0.7%, 95% CI: − 0.3 to 1.7%), which excluded the predefined non-inferiority margin of − 1.5%. However, teriparatide was not statistically superior to alendronate in improving BMD at lumbar spine (P = 0.169). At 48 weeks, changes in BMD at total hip were − 1.0% and 2.2% in teriparatide and alendronate group, respectively (P < 0.001). The incidence of new fracture showed no statistical difference between groups (P = 0.128). Serum P1NP and β-CTX levels significantly increased in the teriparatide group and markedly decreased in alendronate group (all P < 0.001 vs baseline). The adverse events (AEs) and serious AEs were more common in the teriparatide group than in the alendronate group, which were mainly teriparatide-related hypercalcemia, elevated alkaline phosphatase or parathyroid hormone, dizziness, and arthralgia.
Conclusions
Teriparatide was not inferior to alendronate in increasing BMD at lumbar spine in Chinese postmenopausal women, and they achieved these effects through different mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the global population is aging, osteoporosis and fragility fracture have become public health concerns because of its considerable morbidity, excess mortality, and great risk of disability. As a country with the largest aging population in the world, China is facing great challenges from osteoporosis and bone fracture [1,2,3], followed by a great medication burden on the costs of anti-osteoporotic treatment. Although several anti-osteoporosis agents have been approved for treatment of osteoporosis in China, their high costs as original products place a heavy burden not only on individual patients, but also on the healthcare systems [4].
Recently, the domestic generic recombinant human parathyroid hormone (1–34) (teriparatide) has been developed and its safety and preliminary efficacy are confirmed in the phase I and phase II clinical trials. Given its lower price, the domestic generic teriparatide will represent a more affordable treatment option for patients and healthcare systems, thus increasing patients’ access to treatment.
Bisphosphonate therapy is the current standard therapeutic drugs for the prevention and treatment of osteoporosis. Several studies have demonstrated that alendronate is effective in inhibiting bone resorption, increasing bone mineral density (BMD) and reducing fracture risk in postmenopausal women with osteoporosis [5]. Once-daily teriparatide can stimulate bone formation, increases bone mass, and reduces the risk of vertebral and nonvertebral fractures [6]. However, no randomized, controlled trials involving Chinese postmenopausal women with osteoporosis have compared the effects of teriparatide with bisphosphonate.
Here, we conducted this prospective phase III non-inferiority study of the efficacy and safety between domestic generic teriparatide and alendronate in postmenopausal women with osteoporosis in China.
Methods
Study design and participants
This was an open-label, phase III, randomized controlled trial conducted at hospitals with clinical pharmacology research qualification in China from June 2014 to April 2016. This study covered 19 large hospitals from different regions of East, South, West, and North China. Baseline characteristics of participants recruited in each center were shown in supplementary Table 1.
Ambulatory postmenopausal women aged 45–85 years old were eligible for enrollment if they had a BMD T-score of − 2.5 or less at the lumbar spine, total hip, or femoral neck or a BMD T-score of − 1.0 or less at either of the above sites with a history of one or more fragility fractures at the vertebra, hip, proximal humerus, or distal radius [7]. Participants were excluded if they had evidence of hyperparathyroidism, hereditary bone diseases or secondary osteoporosis, history of malignancy or radiation therapy, significant cardiopulmonary, hepatic or renal diseases, poorly controlled diabetes or hypertension, gastrointestinal disorders contraindicating alendronate, mental diseases, or cognitive impairment. Participants with treatment history of bisphosphonates within recent 1.5 years before enrolment, or estrogens, selective estrogen receptor modulators within 6 months before enrolment, or calcitonin, glucocorticoids, or vitamin K2 within 3 months before enrolment were also excluded from this study. Additional exclusion criteria included allergy to study drugs or their metabolites, inability to stand or sit upright for at least 30 min.
The study was approved by ethics committee of clinical pharmacology center of Peking Union Medical College Hospital (PUMCH) and all other participating units. All participants provided written informed consents before any study-specific procedure.
Randomization and treatment
Participants were randomly assigned (2:1) to receive subcutaneous injection of 20ug teriparatide (Suzhou Jinmeng Biotechnology Co., Ltd.) daily or oral 70 mg alendronate sodium (Hangzhou MSD Pharmaceutical Co., Ltd.) weekly. The randomization of participants was not stratified. An interactive web response system (IWRS) was implemented for random allocation at 19 study centers. All participants were supplemented with calcium 500 mg plus Vitamin D3 200 IU (General Electric Pharmaceutical Co., Ltd.) daily. The treatment course was 48 weeks. Participants and investigators were aware of treatment assignment, but BMD assessors, imaging radiologists, and laboratory staff performing biochemical assay were unaware of patients' treatment groups.
Procedures
Areal BMD of the posterior-anterior lumbar spine, total hip, and femoral neck was measured at baseline, 24 weeks, and 48 weeks of treatments by dual-energy X-ray absorptiometry (DXA) using a Hologic (Hologic, Bedford, MA) or Lunar (GE Healthcare, Madison, WI) equipment. All scans of an individual subject were performed on the same densitometer. Quality control measurements were performed daily with a Hologic or Lunar anthropomorphic spine phantom. DXA scan data were submitted to a central imaging vendor (PUMCH) for blinded analyses. The least significant change (LSC) in BMD measured at lumbar spine was used to evaluate effects on BMD. LSC for lumbar spine obtained at PUMCH was 1.93%.
New incident vertebral fractures were assessed by Genant semi-quantitative grading [8] of lateral X-ray images of spine collected before and after 48-week treatment. The other new fractures were confirmed by medical history and X-ray images during the treatment.
Fasting morning blood samples were obtained at each visit and stored at − 80 °C for batch analyses performed in the central laboratory (PUMCH). Serum procollagen type 1 N-terminal propeptide (P1NP), a marker of bone formation, was measured via electro-chemiluminescent immunoassay (Roche Diagnostics) with inter-and intra-assay coefficients of variation (CVs) of 10% and 8%, respectively. Serum β-C-terminal telopeptide of type 1 collagen (β-CTX), a marker of bone resorption, was measured via a fully automated electro-chemiluminescent immunoassay (Roche Diagnostics) with an inter-assay CV of < 5%. The limit of detection for serum β-CTX was 0.01 ng/mL and the reportable range was 0.01 to 5.99 ng/ml. For each marker, all blood samples from a participant were analyzed together in the same assay run. Bone turnover markers (BTMs) of patients were measured at baseline, 12, 24, and 48 weeks of treatment. Serum levels of calcium, phosphorus, alkaline phosphatase (ALP), alanine aminotransferase (ALT), and creatinine (Cr) were measured by automatic biochemical analyzer.
Data on adverse events (AEs), serious AEs (SAEs), and concomitant medications were collected at each study visit. AEs and SAEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA). At the time of reporting, a physician determined whether AEs were related to the study drug.
Study outcomes
The primary endpoint of the study was confirmation of non-inferiority of teriparatide to alendronate for the mean percentage change in BMD at the lumbar spine from baseline to 48 weeks. Secondary efficacy end point was superiority test comparing teriparatide and alendronate for the mean percentage change in BMD at the lumbar spine from baseline to 48 weeks, which was evaluated only if noninferiority was demonstrated. Additional end points included the mean percentage changes in BMD at the lumbar spine from baseline to 24 weeks; the mean percentage changes in BMD at total hip from baseline to 24 and 48 weeks; changes in BTMs of P1NP and β-CTX from baseline to 12, 24, and 48 weeks; and the incidence of fracture within 48 weeks of treatment.
Statistical analysis
The primary hypothesis of this study was that the efficacy of teriparatide was not inferior to alendronate for the mean percentage change in lumbar spine BMD at week 48 from baseline. The secondary hypothesis was that superiority of teriparatide for the mean percentage change in lumbar spine BMD at week 48 from baseline. Based on the previous studies comparing alendronate with placebo [9,10,11,12], and the experience of the clinicians who developed the study protocol, it was assumed that the mean change of alendronate treatment at week 48 on the lumbar spine relative to placebo in postmenopausal women was 4.0 ± 3.0%, a sample size of 324 and 162 in the teriparatide and alendronate groups would provide 80% power to detect non-inferiority of teriparatide to alendronate, with a one-sided significance level of 0.025 and non-inferiority margin of − 1.5%. Considering the actual possible shedding of 15%, 382 and 191 patients in the teriparatide and alendronate groups were included in this study. Based on the calculated sample size, the statistical power for the secondary endpoint was 90% to detect a significant superiority of teriparatide for the mean percentage change in lumbar spine BMD at week 48 from baseline.
The efficacy analysis was conducted on the basis of the full analysis set (FAS) and the per-protocol set (PPS). The FAS included all patients who received at least one dose of medication, and the PPS included the patients in the FAS who had no major protocol deviations and received at least 80% of the planned teriparatide or alendronate doses during 48 weeks of treatment. All baseline demographic data was analyzed on the basis of FAS. The data of each visit were described as mean ± SD if normally distributed. Changes in BMD between baseline and each visit were analyzed with repeated measures analysis of variance. The percentage change from baseline in BMD was compared between groups using a linear mixed-effects model with fixed effects for baseline BMD, centers, machine type, and interaction between center and group as covariates. Sensitivity analyses for missing data for percentage change from baseline in BMD at lumbar spine were performed by a repeated measure mixed-effects model. Descriptive statistics of BTMs were expressed as median (interquartile range). The treatment difference of BTMs at each visit was analyzed using Wilcoxon rank sum test. The counting data were presented as frequency (composition ratio). The intergroup comparisons of the incidences of fractures from baseline to 48 weeks were analyzed by Fisher’s exact test.
The safety was evaluated on the safety analysis set (SAS), which included patients who received at least one dose of teriparatide or alendronate. Fisher’s exact test was used to compare the incidence of AEs between groups.
The statistical analyses were carried out using SAS version 9.4 (SAS Institute, Cary, NC, USA) statistical software. P values < 0.05 were considered statistically significant.
Results
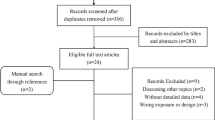
Of 1146 women who were screened for the study, 559 women were not eligible or were unwilling to participate. Five hundred eighty-seven subjects enrolled in the study were randomly assigned to receive teriparatide (391 subjects) or alendronate (196 subjects) treatment. Five hundred thirteen (87.4%) completed 48 weeks of follow-up, of whom 328 were in the teriparatide group and 185 in the alendronate group. Three hundred seventy-nine in the teriparatide group and 194 in the alendronate group received at least one dose of treatment and were included in the FAS and SAS (Fig. 1). Except for BMD at lumbar spine, there were no differences in baseline characteristics between those who withdrew from the study and completed the study (Supplementary Table 2).
No significant differences were found between these two groups in baseline demographics and clinical characteristics, such as age, height, weight, menopause time, history of osteoporotic fracture, BMD, and BTMs (Table 1).
Changes in BMD and incidence of fracture after the treatment
After 24 weeks of treatment, the BMD at lumbar spine and total hip increased 3.0% (95% CI: 2.5–3.5%) and − 1.2% (95% CI: − 1.6 to − 0.8%) in the teriparatide group and 3.2% (95% CI: 2.8–3.8%) and 1.6% (95% CI: 1.1–2.1%) in the alendronate group (all P < 0.001 vs baseline) (Fig. 2). Between-group comparisons showed no difference in BMD changes at lumbar spine (P = 0.438) while significant difference at total hip (P < 0.001). After 48 weeks of treatment, BMD at lumbar spine increased 5.2% (95% CI: 4.6–5.8%) from baseline in the teriparatide group and 4.4% (95% CI: 3.7–5.0%) in the alendronate group. The treatment difference was 0.7% (95% CI: − 0.3 to 1.7%, P = 0.169), which excluded the predefined non-inferiority margin of − 1.5%, indicating that the effect of teriparatide treatment was not inferior to alendronate. The superiority test showed that BMD change at lumbar spine between groups did not reach statistical significance (P = 0.169). Nevertheless, the PPS analysis showed a greater BMD increase at lumbar spine in the teriparatide group than in the alendronate group (P = 0.033). Furthermore, sensitivity analyses for missing data for lumbar spine BMD also showed a significantly greater change in the teriparatide group than in the alendronate group at 48 weeks (P = 0.020). BMD at total hip increased − 1.0% (95% CI: − 1.5 to − 0.5%) in the teriparatide group (P = 0.001) and 2.2% (1.6–2.8%) in the alendronate group (both P < 0.001 vs baseline), with a treatment difference of − 3.1% (95% CI: − 3.9 to − 2.3%) (P < 0.001). At 48 weeks of treatment, BMD gains greater than LSC at lumbar spine were 63.43% in the teriparatide group and 63.93% in the alendronate group, with no significant difference between the two groups (P = 0.925).
The incidence of new fractures during 48 weeks of treatment was 1.1% (4/377) in the teriparatide group and 2.6% (5/194) in the alendronate group. No statistically significant difference was observed between these two groups (P = 0.128).
Changes in BTMs after the treatment
Serum levels of P1NP and β-CTX were significantly elevated after 12-, 24- and 48-week treatment of teriparatide (P < 0.001 vs baseline). However, serum levels of P1NP and β-CTX significantly declined after 12-, 24- and 48-week treatment of alendronate (P < 0.001 vs baseline), which indicated that teriparatide increased BMD through stimulating bone formation while alendronate increased BMD through reducing bone resorption (Fig. 3).
Adverse events
The overall incidence of any AEs was significantly higher in the teriparatide group than the alendronate group (76.52%% vs. 63.92%%, P = 0.002). Drug-related AEs adjudicated by the investigators was 47.76% (181/379) and 26.29% (51/194) in the teriparatide and alendronate groups, respectively, and statistically significant difference was observed between these two groups (P < 0.001). Serious AEs were reported in 36 subjects (9.50%) in teriparatide group and 9 subjects (4.64%) in alendronate group (P = 0.048). AEs leading to discontinuation of the study occurred in 9 subjects (2.37%) of the teriparatide group, which was more than the alendronate group (1 subject, 0.52%), but not statistically significant (P = 0.176). One subject in the teriparatide group died during the study period due to serious trauma caused by traffic accident; the investigator ruled out causal relationship to the study drug.
AEs occurring at an incidence of 5% or above were as follows: elevated ALP (15.04%), hypercalcemia (10.03%), dizziness (8.18%), respiratory tract infection (7.92%), hypercholesterolemia (7.65%), hypertriglyceridemia (6.07%), arthralgia (5.54%), and back pain (5.28%) in the teriparatide group and hypercholesterolemia (8.76%), elevated parathyroid hormone (8.25%), hypertriglyceridemia (7.22%), and upper respiratory tract infection (6.19%) in the alendronate group (Table 2). The incidences of elevated alkaline phosphatase (15.04% vs. 1.03%) and hypercalcemia (10.03% vs. 1.03%) were significantly higher in the teriparatide group than the alendronate group (both P < 0.001), which was considered as closely related to the pharmacological action of teriparatide. The adherence in the teriparatide and alendronate groups were 88.73 ± 24.28% and 96.54 ± 14.93%, respectively, with a significant difference between these two groups (P < 0.001), which may be due to the fact that once-weekly oral administration is more acceptable than once-daily subcutaneous injection.
Discussion
In this prospective controlled study, we demonstrated that subcutaneous injection of teriparatide was noninferior to oral alendronate in improving BMD at lumbar spine in postmenopausal women with osteoporosis; moreover, teriparatide showed a trend toward superiority for increasing lumbar spine BMD as well as greater reductions in fracture risks, compared with alendronate during 48 weeks treatment. Teriparatide significantly increased BTMs while alendronate decreased BTMs, indicating the two treatments promote BMD through different mechanisms.
As this study showed, BMD at lumbar spine increased 5.2% after 48-week treatment of teriparatide, which was not inferior to the efficacy of alendronate, but did not meet statistical superiority in FAS analysis. Several randomized trials comparing the efficacy of teriparatide and bisphosphonates found considerably greater BMD increases at lumbar spine in the teriparatide group than in the bisphosphonates group [6, 13, 14]. However, we did not draw this conclusion from this study. Also, a retrospective study suggested that 12 months of teriparatide treatment could lead to a significant 9.7% increase of lumbar spine BMD [15]. A multicenter study assessed the safety and efficacy of teriparatide 20 µg in Japanese men and women with osteoporosis at high risk of fracture and found teriparatide significantly increased lumbar spine BMD by 10.04% at 12 months of treatment [16]. Another study indicated that lumbar spine BMD had increased by 8.1% at 12 months of teriparatide treatment [17]. In the current study, the increase of BMD at lumbar spine with teriparatide treatment was lower relative to the above studies; this was probably because domestic teriparatide was a biosimilar to Forteo®, and the treatment period was relative short. However, if we take PPS into account, there did indeed a statistical greater BMD increase at lumbar spine in the teriparatide group than in the alendronate group (P = 0.033); thereby, longer follow-up or larger sample size was needed to further evaluate its clinical efficacy. Meanwhile, we did not observe the total hip BMD increase in the teriparatide group, and the difference with several previous studies also seemed to be related to the shorter treatment time [18,19,20]. Nevertheless, a study by Susan et al. [21] had found a decrease of 0.5% in total hip BMD at 6 months of teriparatide treatment; also, another study had indicated a slight reduction in total hip BMD of 12 months of teriparatide treatment [22], which were generally in line with the findings in our study. This may be explained by the fact that teriparatide increases bone turnover, then expands the cortical bone remodeling space and replaces older mineralized bone with newer, but not yet fully mineralized bone tissue, thus resulting in a transient decrease in BMD values of cortical bone [23]. The gains of BMD at the proximal femur often require 18–24 months of teriparatide administration [19]; therefore, changes in femoral neck BMD assessed by DXA may not accurately reflect the changes in bone structure or strength that occur with teriparatide in our study.
Osteoporosis occurred as a result of an imbalance between bone resorption and bone formation, with bone breakdown exceeding bone building. Teriparatide had dual, time-dependent effects on bone resorption and bone formation, and intermittent teriparatide could directly increase osteoblasts activity and indirectly increase bone resorption [24, 25]. In this study, teriparatide significantly increased P1NP level, which exceeded the increase of β-CTX, suggesting that bone formation was first stimulated by PTH treatment, and followed by bone resorption. Furthermore, BTMs of P1NP and β-CTX remained in markedly elevated levels, though lower than peak values, at 48 weeks of teriparatide treatment, indicating that bone formation was ongoing increased with teriparatide treatment. In contrast, alendronate has been shown to increase BMD by inhibiting bone resorption. A study assessed the progressive effects of teriparatide and bisphosphonate (zoledronic acid) on bone remodeling and material properties in postmenopausal women with osteoporosis and suggested that teriparatide stimulated new bone formation and produced a mineralized bone matrix with a stable mean mineral content [26], and zoledronic acid slowed bone turnover and prolonged secondary mineralization and produced a highly mineralized bone matrix [26], which revealed that the underlying mechanisms of teriparatide and bisphosphonates increasing BMD were fundamentally different.
Fracture was the most severe complication of osteoporosis. In this study, the incidence of new fracture was 1.1% in the teriparatide group, which was only one half of that in the alendronate group (2.6%), but without significant difference between the two groups. Due to the relative shorter observational period, it was difficult to observe the true effects of teriparatide and alendronate treatment on fracture in this study. Large sample clinical study confirmed teriparatide significantly reduced the risk of new vertebral fracture for patients with all endpoint BMD values, and increases in lumbar spine BMD accounted for 30–41% of the vertebral fracture risk reduction with teriparatide treatment [27]. Data from 4 real-world observational studies showed that teriparatide treatment led to significant reductions in rates of clinical vertebral fracture, non-vertebral fracture, and clinical fractures in patients [28]. A systematic review and meta-analysis of the efficacy of teriparatide in hip fractures in women and men with osteoporosis was conducted, which showed an odds ratio for hip fractures of 0.44 (P < 0.05) in patients treated with teriparatide than controls [29]. Therefore, we speculate that teriparatide treatment for a longer period will not only be useful to increase lumbar and hip BMD, but also be of benefit to reducing the risk of vertebral and non-vertebral fractures.
The AEs and serious AEs were more common in the teriparatide group than in the alendronate group. As expected, hypercalcemia and elevated ALP were closely correlated to teriparatide treatment, which would be more frequent in the teriparatide group than in the alendronate group. Also, the frequency of dizziness was significantly higher in the teriparatide group than in the alendronate group, which was consistent with previous studies [30, 31]. This may be related to orthostatic hypotension caused by teriparatide treatment[32]. Except for one patient who died in a traffic accident in the teriparatide group, all serious AEs were gradually relieved during teriparatide treatment. No participants dropped out of the study because of the AEs. However, considering the relatively more common AEs and serious AEs in teriparatide group, it was necessary to closely monitor the teriparatide-related adverse events in its clinical application.
There were several clinical significances of this study. This was the first prospective randomized study to compare the efficacy of domestic generic teriparatide and alendronate in Chinese postmenopausal women with osteoporosis. Studies revealed that teriparatide could significantly increase BMD of lumbar spine, which was not inferior to alendronate. The changes of BTMs fully elucidated the anabolic effects of teriparatide, which was completely different from the mechanism of inhibiting bone resorption of alendronate. The overall safety of domestic teriparatide treatment was well. However, limitations of the study included an open-label design, the relatively short-term observational period, lack of data on BMD changes at femoral neck, and two distinct types of DXA equipment which may lead to bias of results of BMD. The limitations of this study included that it was a relatively short-term follow-up study and the effects of treatment on incidence of fracture were difficult to observe. Also, the lack of blinding in study medication may lead to the relatively higher drop-out rate in the teriparatide group (Fig. 1) due to the inconvenience of daily subcutaneous injection of teriparatide. This high dropout rate might affect study outcomes. Additionally, since BMD was measured using two distinct types of DXA equipment in each study center, the skills of operators and the scanning techniques might have differed across the institutions, which may lead to bias of results of BMD.
In summary, in postmenopausal women with osteoporosis, domestic generic teriparatide could improve BMD at lumbar spine, and the clinical efficacy was non-inferior to alendronate. It provided a new choice for the treatment of postmenopausal osteoporosis in Chinese population, but the clinical research with longer time and larger sample was worth continuing.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Code availability
Not applicable.
References
Gao C, Xu Y, Li L et al (2019) Prevalence of osteoporotic vertebral fracture among community-dwelling elderly in Shanghai. Chin Med J (Engl) 132:1749–1751. https://doi.org/10.1097/cm9.0000000000000332
Wang L, Yu W, Yin X et al (2021) Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open 4:e2121106. https://doi.org/10.1001/jamanetworkopen.2021.21106
Zhang C, Feng J, Wang S et al (2020) Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLoS Med 17:e1003180. https://doi.org/10.1371/journal.pmed.1003180
Jiang B, Zhou RJ, Feng XL (2022) The impact of the reference pricing policy in China on drug procurement and cost. Health Policy Plan 37:73–99. https://doi.org/10.1093/heapol/czab012
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393:364–376. https://doi.org/10.1016/s0140-6736(18)32112-3
Yuan F, Peng W, Yang C, Zheng J (2019) Teriparatide versus bisphosphonates for treatment of postmenopausal osteoporosis: A meta-analysis. Int J Surg 66:1–11. https://doi.org/10.1016/j.ijsu.2019.03.004
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 UPDATE. Endocr Pract 26:1–46. https://doi.org/10.4158/gl-2020-0524suppl
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Liberman UA, Weiss SR, Bröll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW Jr, Dequeker J, Favus M (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med 333:1437–1443. https://doi.org/10.1056/nejm199511303332201
Orwoll E, Ettinger M, Weiss S et al (2000) Alendronate for the treatment of osteoporosis in men. N Engl J Med 343:604–610. https://doi.org/10.1056/nejm200008313430902
Kung AW, Yeung SS, Chu LW (2000) The efficacy and tolerability of alendronate in postmenopausal osteoporotic Chinese women: a randomized placebo-controlled study. Calcif Tissue Int 67:286–290. https://doi.org/10.1007/s0022330001142
Yan Y, Wang W, Zhu H, Li M, Liu J, Luo B, Xie H, Zhang G, Li F (2009) The efficacy and tolerability of once-weekly alendronate 70 mg on bone mineral density and bone turnover markers in postmenopausal Chinese women with osteoporosis. J Bone Miner Metab 27:471–478. https://doi.org/10.1007/s00774-009-0057-7
Panico A, Lupoli GA, Marciello F, Lupoli R, Cacciapuoti M, Martinelli A, Granieri L, Iacono D, Lupoli G (2011) Teriparatide vs alendronate as a treatment for osteoporosis: changes in biochemical markers of bone turnover, BMD and quality of life. Med Sci Monit 17:Cr442-448. https://doi.org/10.12659/msm.881905
Body JJ, Gaich GA, Scheele WH et al (2002) A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1–34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 87:4528–4535. https://doi.org/10.1210/jc.2002-020334
Niimi R, Kono T, Nishihara A, Hasegawa M, Kono T, Sudo A (2016) The Relationship of BMD Increases Between the First 12 Months and the Latter 12 Months by Daily Teriparatide Treatment. Calcif Tissue Int 99:282–288. https://doi.org/10.1007/s00223-016-0151-5
Miyauchi A, Matsumoto T, Sugimoto T, Tsujimoto M, Warner MR, Nakamura T (2010) Effects of teriparatide on bone mineral density and bone turnover markers in Japanese subjects with osteoporosis at high risk of fracture in a 24-month clinical study: 12-month, randomized, placebo-controlled, double-blind and 12-month open-label phases. Bone 47:493–502. https://doi.org/10.1016/j.bone.2010.05.022
Cohen A, Shiau S, Nair N et al (2020) Effect of teriparatide on bone remodeling and density in premenopausal idiopathic osteoporosis: a phase II trial. J Clin Endocrinol Metab 105.https://doi.org/10.1210/clinem/dgaa489
Eastell R, Mitlak BH, Wang Y, Hu M, Fitzpatrick LA, Black DM (2019) Bone turnover markers to explain changes in lumbar spine BMD with abaloparatide and teriparatide: results from ACTIVE. Osteoporos Int 30:667–673. https://doi.org/10.1007/s00198-018-04819-1
Finkelstein JS, Wyland JJ, Lee H, Neer RM (2010) Effects of teriparatide, alendronate, or both in women with postmenopausal osteoporosis. J Clin Endocrinol Metab 95:1838–1845. https://doi.org/10.1210/jc.2009-1703
Tsai JN, Lee H, David NL, Eastell R, Leder BZ (2019) Combination denosumab and high dose teriparatide for postmenopausal osteoporosis (DATA-HD): a randomised, controlled phase 4 trial. Lancet Diabetes Endocrinol 7:767–775. https://doi.org/10.1016/s2213-8587(19)30255-4
Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, Blosch CM, Mathisen AL, Morris SA, Marriott TB (2007) Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med 146:326–339. https://doi.org/10.7326/0003-4819-146-5-200703060-00005
Finkelstein JS, Hayes A, Hunzelman JL, Wyland JJ, Lee H, Neer RM (2003) The effects of parathyroid hormone, alendronate, or both in men with osteoporosis. N Engl J Med 349:1216–1226. https://doi.org/10.1056/NEJMoa035725
McClung MR, San Martin J, Miller PD, Civitelli R, Bandeira F, Omizo M, Donley DW, Dalsky GP, Eriksen EF (2005) Opposite bone remodeling effects of teriparatide and alendronate in increasing bone mass. Arch Intern Med 165:1762–1768. https://doi.org/10.1001/archinte.165.15.1762
Tang CH (2020) Osteoporosis: from molecular mechanisms to therapies. Int J Mol Sci 21.https://doi.org/10.3390/ijms21030714
Isogai Y, Takao-Kawabata R, Takakura A, Sugimoto E, Nakazono O, Ikegaki I, Kuriyama H, Ishizuya T (2015) Early effects of single and low-frequency repeated administration of teriparatide, hPTH(1–34), on bone formation and resorption in ovariectomized rats. Calcif Tissue Int 97:412–420. https://doi.org/10.1007/s00223-015-0026-1
Dempster DW, Roschger P, Misof BM, Zhou H, Paschalis EP, Alam J, Ruff VA, Klaushofer K, Taylor KA (2016) Differential effects of teriparatide and zoledronic acid on bone mineralization density distribution at 6 and 24 months in the SHOTZ study. J Bone Miner Res 31:1527–1535. https://doi.org/10.1002/jbmr.2825
Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH (2006) Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res 21:1785–1790. https://doi.org/10.1359/jbmr.060802
Langdahl BL, Silverman S, Fujiwara S et al (2018) Real-world effectiveness of teriparatide on fracture reduction in patients with osteoporosis and comorbidities or risk factors for fractures: integrated analysis of 4 prospective observational studies. Bone 116:58–66. https://doi.org/10.1016/j.bone.2018.07.013
Díez-Pérez A, Marin F, Eriksen EF, Kendler DL, Krege JH, Delgado-Rodríguez M (2019) Effects of teriparatide on hip and upper limb fractures in patients with osteoporosis: a systematic review and meta-analysis. Bone 120:1–8. https://doi.org/10.1016/j.bone.2018.09.020
Kendler DL, Marin F, Zerbini CAF et al (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391:230–240. https://doi.org/10.1016/s0140-6736(17)32137-2
Neer RM, Arnaud CD, Zanchetta JR et al (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441. https://doi.org/10.1056/nejm200105103441904
Nickols GA, Nana AD, Nickols MA, DiPette DJ, Asimakis GK (1989) Hypotension and cardiac stimulation due to the parathyroid hormone-related protein, humoral hypercalcemia of malignancy factor. Endocrinology 125:834–841. https://doi.org/10.1210/endo-125-2-834
Acknowledgements
We thank the staff in the 19 hospitals of China for the study and the study volunteers for their participation. We thank department of radiology of PUMCH for quality control of DXA measurement in each center. We thank Shanghai Dean Medical Laboratory Co., Ltd, for assistance with the BTMs analysis. We thank professor Hao Yu and statistician Jinjin Cao of Biostatistics Department, School of Public Health, Nanjing Medical University, for the statistical analysis. Study drugs were supplied by Suzhou Jinmeng Biotechnology Co., Ltd.
Funding
This study was supported by Suzhou Jinmeng Biotechnology Co., Ltd, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, M., Zhang, Z., Xue, Q. et al. Efficacy of generic teriparatide and alendronate in Chinese postmenopausal women with osteoporosis: a prospective study. Arch Osteoporos 17, 103 (2022). https://doi.org/10.1007/s11657-022-01131-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01131-8