Abstract
Objective
To investigate the mechanism of Tojapride, a Chinese herbal formula extract, on strengthening the barrier function of esophageal epithelium in rats with reflux esophagitis (RE).
Methods
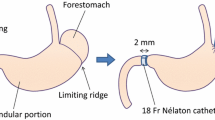
Ten out of 85 SD rats were randomly selected as the sham group (n10), and 75 rats were developed a reflux esophagitis model (RE) by the esophageal and duodenal side-to-side anastomosis. Fifty successful modeling rats were divided into different medicated groups through a random number table including the model, low-, medium-, and high-dose of Tojapride as well as omeprazole groups (n10). Three doses of Tojapride [5.73, 11.46, 22.92 g/(kg•d)] and omeprazole [4.17 mg/(kg•d)] were administrated intragastrically twice daily for 3 weeks. And the rats in the sham and model groups were administered 10 mL/kg distilled water. Gastric fluid was collected and the supernatant was kept to measure for volume, pH value and acidity. Esophageal tissues were isolated to monitor the morphological changes through hematoxylin-eosin (HE) staining, and esophageal epithelial ultrastructure was observed by transmission electron microscopy. The expressions of nuclear factor kappa-light-chain-enhancer of activated B cells p65 (NF-KBp65), κB kinase beta (IKKß), occludin, and zonula occludens-1 (ZO-1) in the esophageal tissues were measured by immunohistochemistry and Western blot, respectively.
Results
The gastric pH value in the model group was significantly lower than the sham group (P<0.05). Compared with the model group, gastric pH value in the omeprazole and medium-dose of Tojapride groups were significantly higher (P<0.05). A large area of ulceration was found on the esophageal mucosa from the model rats, while varying degrees of congestion and partially visible erosion was observed in the remaining groups. Remarkable increase in cell gap width and decrease in desmosome count was seen in RE rats and the effect was reversed by Tojapride treatment. Compared with the sham group, the IKKß levels were significantly higher in the model group (P<0.05). However, the IKKß levels were down-regulated after treatment by all doses of Tojapride (P<0.01 or P<0.05). The occluding and ZO-1 levels decreased in the model group compared with the sham group (Ps0.01 or Ps0.05), while both indices were significantly up-regulated in the Tojapride-treated groups (P<0.01 or P<0.05).
Conclusions
Tojapride could improve the pathological conditions of esophageal epithelium in RE rats. The underlying mechanisms may involve in down-regulating the IKKß expression and elevating ZO-1 and occludin expression, thereby alleviating the inflammation of the esophagus and strengthening the barrier function of the esophageal epithelium.
Similar content being viewed by others
References
Kandulski A, Malfertheiner P. Gastroesophageal reflux disease— from reflux episodes to mucosal inflammation. Nat Rev Gastroenterol Hepatol 2011;9:15–22.
Kinekawa F, Kubo F, Matsuda K, Kobayashi M, Furuta Y, Fujita Y, et al. Esophageal function worsens with long duration of diabetes. J Gastroenterol 2008;43:338–344.
Souza RF, Huo X, Mittal V, Schuler CM, Carmack SW, Zhang HY, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology 2009;137:1776–1784.
Gweon TG, Park JH, Kim BW, Choi YK, Kim JS, Park SM, et al. Additive effects of rebamipide plus proton pump inhibitors on the expression of tight junction proteins in a rat model of gastro-esophageal reflux disease. Gut Liver 2018;12:46–50.
Mönkemüller K, Wex T, Kuester D, Fry LC, Kandulski A, Kropf S, et al. Role of tight junction proteins in gastroesophageal reflux disease. BMC Gastroenterol 2012;12:128–140.
Oshima T, Gedda K, Koseki J, Chen X, Husmark J, Watari J, et al. Establishment of esophageal-like non-keratinized stratified epithelium using normal human bronchial epithelial cells. Am J Physiol Cell Physiol 2011;300:1422–1429.
Oshima T, Sasaki M, Kataoka H, Miwa H, Takeuchi T, Joh T. Wip1 protects hydrogenperoxide-induced colonic epithelial barrier dysfunction. Cell Mol Life Sci 2007;64:3139–3147.
Hashimoto K, Oshima T, Tomita T, Kim Y, Matsumoto T, Joh T, et al. Oxidative stress induces gastric epithelial permeability through claudin-3. Biochem Biophys Res Commun 2008;376:154–157.
Neumann H, Mönkemüller K, Fry LC, Dombrowski F, Kuester D, Beyer M, et al. Intercellular space volume is mainly increased in the basal layer of esophageal squamous epithelium in patients with GERD. Dig Dis Sci 2010;56:1404–1411.
Ma J, Altomare A, Guarino M, Cicala M, Rieder F, Fiocchi C, et al. HCl-induced and ATP-dependent upregulation of TRPV1 receptor expression and cytokine production by human esophageal epithelial cells. Am J Physiol Gastrointest Liver Physiol 2012;303:635–645.
Weijenborg PW, Smout AJ, Verseijden C, van Veen HA, Verheij J, de Jonge WJ, et al. Hypersensitivity to acid is associated with impaired esophageal mucosal integrity in patients with gastroesophageal reflux disease with and without esophagitis. Am J Physiol Gastrointest Liver Physiol 2014;307:323–329.
Orlando RC. The integrity of the esophageal mucosa. Balance between offensive and defensive mechanisms. Best Pract Res Clin Gastroenterol 2010;24:873–882.
Woodland P, Al-Zinaty M, Yazaki E, Sifrim D. In vivo evaluation of acid-induced changes in oesophageal mucosa integrity and sensitivity in non-erosive reflux disease. Gut 2013;62:1256–1261.
Rieder F, Biancani P, Harnett K, Yerian L, Falk GW. Inflammatory mediators in gastroesophageal reflux disease: impact on esophageal motility, fibrosis, and carcinogenesis. Am J Physiol Gastrointest Liver Physiol 2010;298:571–581.
Kang JW, Lee SM. Protective effects of chlorogenic acid against experimental reflux esophagitis in rats. Biomol Ther 2014;22:420–425.
Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2012;108:308–328.
Zeng YQ, Dai Z, Lu F, Lu L, Lu X, Chen C, et al. Emodin via colonic irrigation modulates gut microbiota and reduces uremic toxins in rats with chronic kidney disease. Oncotarget 2016;7:17468–17478.
Jang Y, Kim TK, Shim WS. Naringin exhibits in vivo prokinetic activity via activation of ghrelin receptor in gastrointestinal motility dysfunction rats. Pharmacology 2013;92:191–197.
Jang Y, Kim SW, Oh J, Hong GS, Seo EK, Oh U, et al. Ghrelin receptor is activated by naringin and naringenin, constituents of a prokinetic agent Poncirus fructus. J Ethnopharm 2013;148:459–465.
Tang XD, Wu HM, Shan Y, Wang ZB, Shao Y, Hu CY. Tongjiang Granule impact the function of gastric emptying in experimental animals. Chin J Experiment Tradit Med Formul (Chin) 2006;12:24–26.
Li BS, Li ZH, Tang XD, Zhang LY, Zhao YP, Bian LP, et al. A randomized, controlled, double-blinded and double-dummy trial of the effect of Tongjiang Granule on the nonerosive reflux disease of and Gan-Wei incoordination syndrome. Chin J Integr Med 2011;17:339–345.
Fang Y, Chen H, Hu Y, Djukic Z, Tevebaugh W, Shaheen NJ, et al. Gastroesophageal reflux activates the NF-κB pathway and impairs esophageal barrier function in mice. Am J Physiol Gastrointest Liver Physiol 2013;305:58–65.
Okabe S, Takinami Y, Iwata K, Yanagawa T. Mucosal protective effect of leminoprazole on reflux esophagitis induced in rats. Japn J Pharmacol 1995;69:317–323.
Altomare A, Guarino MP, Cocca S, Emerenziani S, Cicala M. Gastroesophageal reflux disease: update on inflammation and symptom perception. World J Gastroenterol 2013;19:6523–6528.
Chen X, Oshima T, Shan J, Fukui T, Miwa H, et al. Bile salts disrupt human esophageal squamous epithelial barrier function by modulating tight junction proteins. AJP Gastrointest Liver Physiol 2012;303:G199–G208.
Boeckxstaens GE, Rohof W. Pathophysiology of gastroesophageal reflux disease. Gastroenterol Clin North Am 2014;43:15–25.
Liu Y, Nusrat A, Schnell FJ, Reaves TA, Walsh S, Pochet M, et al. Human junction adhesion molecule regulates tight junction resealing in epithelia. J Cell Sci 2000;113:2363–2374.
Jovov B, van Itallie CM, Shaheen NJ, Carson JL, Gambling TM, Anderson JM, et al. Claudin-18: a dominant tight junction protein in Barrett’s esophagus and likely contributor to its acid resistance. Am J Physiol Gastrointest Liver Physiol 2007;293:1106–1113.
Chatzipanteli K, Yanagawa Y, Marcillo AE, Kraydieh S, Yezierski RP, Dietrich WD. Posttraumatic hypothermia reduces polymorphonuclear leukocyte accumulation following spinal cord injury in rats. J Neurotrauma 2000;17:321–332.
Chen LF, Greene WC. Shaping the nuclear action of NF-kappaB. Nat Rev Mol Cell Biol 2004;5:392–401.
Vageli DP, Prasad ML, Sasaki CT. Gastro-duodenal fluid induced nuclear factor-κ appaB activation and early pre-malignant alterations in murine hypopharyngeal mucosa. Oncotarget 2016;7:5892–5908.
Green NH, Huang Q, Corfe BM, Bury JP, MacNeil S. NF-kappaB is activated in oesophageal fibroblasts in response to a paracrine signal generated by acid-exposed primary oesophageal squamous cells. Int J Exp Pathol 2011;92:345–356.
Chen X, Oshima T, Shan J, Fukui H, Watari J, Miwa H. Bile salts disrupt human esophageal squamous epithelial barrier function by modulating tight junction proteins. Am J Physiol Gastrointest Liver Physiol 2012;303:199–208.
Al-Sadi R, Ye D, Dokladny K, Ma TY. Mechanism of IL-1 ß -induced increase in intestinal epithelial tight junction permeability. J Immunol 2008;180:5653–5661.
Al-Sadi R, Ye D, Said HM, Ma TY. IL-1 ß-induced increase in intestinal epithelial tight junction permeability is mediated by MEKK-1 activation of canonical NF- κB pathway. Am J Pathol 2010;177:2310–2322.
AlSadi RM, Ma TY. IL-1 ß causes an increase in intestinal epithelial tight junction permeability. J Immunol 2007;178:4641–4649.
Suzuki T, Yoshinaga N, Tanabe S. Interleukin-6 (IL-6) regulates claudin-2 expression and tight junction permeability in intestinal epithelium. J Biol Chem 2011;286:31263–31271.
Aveleira CA, Lin CM, Abcouwer SF, Ambr’osio AF, Antonetti DA. TNF-α signals through PKC ζ /NF-κB to alter the tight junction complex and increase retinal endothelial cell permeability. Diabetes 2010;59:2872–2882.
Umeda K, Ikenouchi J, Katahira-Tayama S, Furuse K, Sasaki H, Nakayama M, et al. ZO-1 and ZO-2 independently determine where claudins are polymerized in tight-junction strand formation. Cell 2006;126:741–754.
O’Riordan J, AbdelLatif MM, Mcnamara D, Narayanasamy R, Byrne P, Keeling PW, et al. Nuclear factor-kappa B induced cytokine expression along the metaplasia-dysplasia-adenocarcinoma sequence in the esophagus. Gastroenterol 2003;124:A636.
O’Riordan JM, Abdel-latif MM, Ravi N, McNamara D, Byrne PJ, McDonald GS, et al. Proinflammatory cytokine and nuclear factor kappa-B expression along the inflammation metaplasia dysplasia adenocarcinoma sequence in the esophagus. Am J Gastroenterol 2005;100:1257–1264.
Huo X, Zhang X, Yu C, Zhang Q, Cheng E, Wang DH, et al. In esophageal squamous cells exposed to acidic bile salt medium, omeprazole inhibits IL-8 expression through effects on nuclear factor-κB and activator protein-1. Gut 2014;63:1042–1052.
Huo X, Zhang X, Yu C, Cheng E, Zhang Q, Dunbar KB, et al. Aspirin prevents NF-κB activation and CDX2 expression stimulated by acid and bile salts in oesophageal squamous cells of patients with Barrett’s oesophagus. Gut 2017;67:606–615.
Souza RF, Bayeh L, Spechler SJ, Tambar UK, Bruick RK. A new paradigm for GERD pathogenesis. Not acid injury, but cytokine-mediated inflammation driven by HIF-2α: a potential role for targeting HIF-2α to prevent and treat reflux esophagitis. Curr Opin Pharmacol 2017;37:93–99.
Huo X, Agoston AT, Dunbar KB, Cipher DJ, Zhang X, Yu C, et al. Hypoxia-inducible factor-2alpha plays a role in mediating oesophagitis in GORD. Gut 2017;66:1542–1554.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author Contributions|Tang XD and Wang FY designed the study; Yin XL and Zhong L participated in the paper design and preparation; Zhang J, Chen ZY, Duan YZ, JI HJ and Shi XS mainly performed the experiments; Che H, and Tian YX carried out the animal study
Ma XX and Lu L participated in the experimental design and data analysis; Lin CY and Zhao YP were involved in discussion of experiment and preparing the manuscript. All authors read and approved the final manuscript for publication.
Supported by Natural Science Foundation of China (No.81503560), “Ten Diseases and Ten Drugs” Program and the Cultivation Research of Biological Medicine and Life Science Innovation of Beijing Municipal Science and Technology Commission (No. Z141100002214012, Z161100000116046)
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Yin, Xl., Zhong, L., Lin, Cy. et al. Tojapride Reverses Esophageal Epithelial Inflammatory Responses on Reflux Esophagitis Model Rats. Chin. J. Integr. Med. 27, 604–612 (2021). https://doi.org/10.1007/s11655-019-3027-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-019-3027-5