Abstract
Background/Aims
At present, the dilation of esophageal intercellular spaces (ICS) is considered an early morphologic marker of acid damage in patients with GERD. Nevertheless, previous electron microscopic (EM) studies had focused only on the suprabasal layer of squamous epithelium or did not nearly specify which layer of squamous epithelium was studied. Therefore, we aimed to assess the volumetric amount of the ICS in all layers of SE in patients with GERD.
Methods
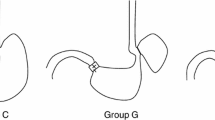
In this study, 48 patients were prospectively included (NERD = 18, ERD = 17; Barrett′s esophagus = 5, controls = 8). All patients with ERD and NERD had typical reflux symptoms, as assessed by a valid GERD questionnaire. ICS volume was assessed by electron microscopy in the superficial, prickle cell, and basal layers of esophageal squamous epithelium using the method of Weibel.
Results
ERD was associated with increased ICS volume in the basal layer (LA-A, p = 0.038; LA-B, p = 0.005) and prickle cell layer (LA-A, p = 0.006; LA-B, p = 0.007) as compared to controls. Comparisons between NERD and ERD patients revealed more dilated ICS in the basal layer (LA-B, p = 0.007), prickle cell layer (LA-A, p = 0.008; LA-B, p = 0.001) and superficial layer (LA-B, p = 0.018) in patients with ERD.
Conclusions
Not only the diameter but also the volume of the ICS is increased in patients with GERD. Furthermore, the dilation of ICS is present in all three layers of the SE, being more pronounced in the basal layer. These findings support the concept that the impairment of the esophagus begins in the deeper parts of the esophageal epithelium.







Similar content being viewed by others
References
Wahlqvist P, Reilly MC, Barkun A. Systematic review: the impact of gastro-oesophageal reflux disease on work productivity. Aliment Pharmacol Ther. 2006;24:259–272.
Spechler SJ. Epidemiology and natural history of gastro-oesophageal reflux disease. Digestion. 1992;51:24–29.
Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920.
Wienbeck M, Barnert J. Epidemiology of reflux disease and reflux esophagitis. Scand J Gastroenterol. 1989;156:7–13.
Vieth M, Peitz U, Labenz J, et al. What parameters are relevant for the histological diagnosis of gastroesophageal reflux disease without Barrett’s mucosa? Dig Dis. 2004;22:196–201.
Caviglia R, Ribolsi M, Gentile M, et al. Dilated intercellular spaces and acid reflux at the distal and proximal oesophagus in patients with non-erosive gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2007;25:629–636.
De Hertogh G, Ectors N, Van Eyken P, et al. Review article: the nature of oesophageal injury in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2006;24:17–26.
Calabrese C, Fabbri A, Bortolotti M, et al. Dilated intercellular spaces as a marker of oesophageal damage: comparative results in gastro-oesophageal reflux disease with or without bile reflux. Aliment Pharmacol Ther. 2003;18:525–532.
Ravelli AM, Villanacci V, Ruzzenenti N, et al. Dilated intercellular spaces: a major morphological feature of esophagitis. J Pediatr Gastroenterol Nutr. 2006;42:510–515.
Hopwood D, Logan KR, Bouchier IA. The electron microscopy of normal human oesophageal epithelium. Virchows Arch B Cell Pathol. 1978;26:345–358.
Lynn RB. Mechanisms of esophageal pain. Am J Med. 1992;92:11–19.
Tobey NA, Hosseini SS, Argote CM, et al. Dilated intercellular spaces and shunt permeability in nonerosive acid-damaged esophageal epithelium. Am J Gastroenterol. 2004;99:13–22.
Farré R, De Vos R, Geboes K, et al. Critical role of stress in increased oesophageal mucosa permeability and dilated intercellular spaces. Gut. 2007;56:1191–1197.
Shaw MJ, Talley NJ, Beebe TJ, et al. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:52–57.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180.
Sampliner RE. Practice parameters committee of the American College of Gastroenterology. Am J Gastroenterol. 2002;97:1888–1895.
Ismail-Beigi F, Horton PF, Pope CE. Histological consequences of gastroesophageal reflux in man. Gastroenterology. 1970;58:163–174.
Weibel ER, Kistler GS, Scherle WF. Practical stereological methods for morphometric cytology. J Cell Biol. 1966;30:23–38.
Weibel ER, Hsia CC, Ochs M. How much is there really? Why stereology is essential in lung morphometry. J Appl Physiol. 2007;102:459–467.
Solcia E, Villani L, Luinetti O, et al. Altered intercellular glycoconjugates and dilated intercellular spaces of esophageal epithelium in reflux disease. Virchows Arch. 2000;436:207–216.
Caviglia R, Ribolsi M, Maggiano N, et al. Dilated intercellular spaces of esophageal epithelium in nonerosive reflux disease patients with physiological esophageal acid exposure. Am J Gastroenterol. 2005;100:543–548.
Hopwood D, Milne G, Logan KR. Electron microscopic changes in human oesophageal epithelium in oesophagitis. J Pathol. 1979;129:161–167.
Barlow WJ, Orlando RC. The pathogenesis of heartburn in nonerosive reflux disease: a unifying hypothesis. Gastroenterology. 2005;128:771–778.
Tobey NA, Carson JL, Alkiek RA, et al. Dilated intercellular spaces: a morphological feature of acid reflux–damaged human esophageal epithelium. Gastroenterology. 1996;111:1200–1205.
Calabrese C, Bortolotti M, Fabbri A, et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am J Gastroenterol. 2005;100:537–542.
Guillem PG. How to make a Barrett esophagus: pathophysiology of columnar metaplasia of the esophagus. Dig Dis Sci. 2005;50:415–424.
Labenz J, Nocon M, Lind T, et al. Prospective follow-up data from the ProGERD study suggest that GERD is not a categorial disease. Am J Gastroenterol. 2006;101:2457–2462.
Souza RF, Huo X, Mittal V, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology. 2009;137:1776–1784.
Richardson KL, Jarett L, Finke EH. Embedding in epoxy resins for ultrathin sectioning in electron microscopy. Stain Technol. 1960;35:313–323.
Nyengaard JR, Gundersen HJG. The isector: a simple and direct method for generating isotropic, uniform random sections from small specimens. J Microsc. 1992;165:427–431.
Tobey NA, Gambling TM, Vanegas XC, et al. Physicochemical basis for dilated intercellular spaces in non-erosive acid-damaged rabbit esophageal epithelium. Dis Esophagus. 2008;21:757–764.
Alvaro-Villegas JC, Sobrino-Cossío S, Hernández-Guerrero A, et al. Dilated intercellular spaces in subtypes of gastroesophagic reflux disease. Rev Esp Enferm Dig. 2010;102:302–307.
Acknowledgments
We thank the endoscopy team for their technical assistance. The study was supported by the NBL-3 program of the “Bundesministerium für Forschung und Technik” (01ZZ0407/PFG1) and the “LOM-Program” of the Medical Faculty of the Otto-von-Guericke University Magdeburg.
Conflicts of interest
None of the authors has any conflicts of interest related to this work to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neumann, H., Mönkemüller, K., Fry, L.C. et al. Intercellular Space Volume Is Mainly Increased in the Basal Layer of Esophageal Squamous Epithelium in Patients with GERD. Dig Dis Sci 56, 1404–1411 (2011). https://doi.org/10.1007/s10620-010-1458-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1458-0