Abstract
Background
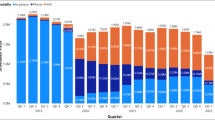
The Veterans Health Administration increased synchronous telemedicine (video and telephone visits) in primary care in response to the COVID-19 pandemic.
Objective
Our objective was to determine veteran use patterns of in-person and telemedicine primary care when all modalities were available.
Design
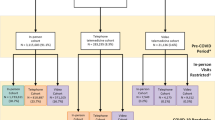
A retrospective cohort analysis. We performed a latent class analysis of primary care visits over a 1-year period to identify veteran subgroup (i.e., class) membership based on amount of primary care use and modality used. Then, we used multinomial logistic regression with a categorical outcome to identify patient characteristics associated with class identification.
Participants
A random national sample consisting of 564,580 primary care empaneled veterans in June 2021.
Main Measures
Latent class membership.
Key Results
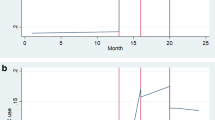
We identified three latent classes: those with few primary care visits that were predominantly telephone-based (45%), intermediate number of visits of all modalities (50%), and many visits of all modalities (5%). In an adjusted model, characteristics associated with the “few” visits class, compared to the intermediate class, were older age, male sex, White race, further driving distance to primary care, higher Gagne, optimal internet speed, and unmarried status (OR 1.002, 1.52, 1.13, 1.004, 1.04, 1.05, 1.06, respectively; p < .05). Characteristics associated with membership in the “many” visits class, compared to the intermediate class, were Hispanic race, higher JEN Frailty Index and Gagne (OR 1.12, 1.11, 1.02, respectively; p < .05), and higher comorbidity by Care Assessment Need score quartile (Q2 1.73, Q3 2.80, Q4 4.12; p < 0.05).
Conclusions
Veterans accessing primary care in-person or via telemedicine do so primarily in three ways: (1) few visits, predominantly telephone; (2) intermediate visits, all modalities, (3) many visits, all modalities. We found no groups of veterans receiving a majority of primary care through video.


Similar content being viewed by others
References
Reddy A, Gunnink E, Deeds SA, Hagan SL, Heyworth L, Mattras TF, Nelson KM. A rapid mobilization of 'virtual' primary care services in response to COVID-19 at Veterans Health Administration. Healthc (Amst). 2020;8(4):100464.
SteelFisher GK, McMurtry CL, Caporello H, Lubell KM, Koonin LM, Neri AJ, Ben-Porath EN, Mehrotra A, McGowan E, Espino LC, Barnett ML. Video Telemedicine Experiences In COVID-19 Were Positive, But Physicians And Patients Prefer In-Person Care For The Future. Health Aff (Millwood). 2023;42(4):575-584.
Ferguson JM, Wray CM, Jacobs J, Greene L, Wagner TH, Odden MC, Freese J, Van Campen J, Asch SM, Heyworth L, Zulman DM. Variation in initial and continued use of primary, mental health, and specialty video care among veterans. Health Serv Res. 2023;58(2):402-414.
Bhatia R, et al. Older adults' perspectives on primary care telemedicine during the COVID‐19 pandemic. J Am Geriatr Soc. 2022;70(12):3480-3492.
Weller, B. E., Bowen, N. K., & Faubert, S. J. Latent class analysis: a guide to best practice. J Black Psychol. 2020;46(4):287–311.
Hebert PL, Liu CF, Wong ES, Hernandez SE, Batten A, Lo S, Lemon JM, Conrad DA, Grembowski D, Nelson K, Fihn SD. Patient-centered medical home initiative produced modest economic results for Veterans Health Administration, 2010-12. Health Aff (Millwood). 2014;33(6):980-7.
Department of Veterans Affairs Office of Information Technology. Decision Support System 3.0 User Guide. November 2023. Available at: https://www.va.gov/vdl/documents/Financial_Admin/Decision_Supp_Sys_(DSS)/ecx_3_ug.pdf. Accessed March 12, 2024.
Nelson K, Schwartz G, Hernandez S, Simonetti J, Curtis I, Fihn SD. The association between neighborhood environment and mortality: results from a national study of veterans. J Gen Intern Med. 2017;32(4):416–422.
O’Shea AMJ, Baum A, Haraldsson B, et al. Association of adequacy of broadband internet service with access to primary care in the veterans health administration before and during the COVID-19 pandemic. JAMA Netw Open. 2022;5(10):e2236524.
Kinosian B, Wieland D, Gu X, et al. Validation of the JEN frailty index in the National Long-Term Care Survey community population: identifying functionally impaired older adults from claims data. BMC Health Serv Res. 2018; 18:908.
Sun JW, Rogers JR, Her Q, et al. Adaptation and validation of the combined comorbidity score for ICD-10-CM. Med Care. 2017;55(12):1046–1051.
Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–759.
Fihn, Stephan., Box, Tami., Care Assessment Need (CAN) Score and the Patient Care Assessment System (PCAS): Tools for Care Management. Veterans Health Administration Office of Informatics and Analytics. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/713-notes.pdf. June 27, 2013. Accessed October 17, 2023.
Holliday R, Kinney AR, Smith AA, Forster JE, Liu S, Monteith LL, Brenner LA. A latent class analysis to identify subgroups of VHA using homeless veterans at greater risk for suicide mortality. J Affect Disord. 2022 Oct 15;315:162-167.
Sinha P, Calfee CS, Delucchi KL. Practitioner's guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49(1):e63-e79.
Meijer E, Gebhardt WA, van Laar C, Chavannes NH, van den Putte B. Identified or conflicted: a latent class and regression tree analysis explaining how identity constructs cluster within smokers. BMC Psychol. 2022;10(1):231.
Blalock DV, Maciejewski ML, Zulman DM, Smith VA, Grubber J, Rosland AM, Weidenbacher HJ, Greene L, Zullig LL, Whitson HE, Hastings SN, Hung A. Subgroups of high-risk veterans affairs patients based on social determinants of health predict risk of future hospitalization. Med Care. 2021;59(5):410-417.
Zhang Z, Abarda A, Contractor AA, Wang J, Dayton CM. Exploring heterogeneity in clinical trials with latent class analysis. Ann Transl Med. 2018;6(7):119. https://doi.org/10.21037/atm.2018.01.24.
Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology (Sunnyvale, Calif.). 2016;6(2) :227.
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2023.
Linzer DA, Lewis JB. poLCA: an R package for polytomous variable latent class analysis. J Stat Softw. 2011;42(10):1-29.
Crook RL, Iftikhar H, Moore S, Lowdon P, Modarres P, Message S. A comparison of in-person versus telephone consultations for outpatient hospital care. Future Healthc J. 2022;9(2):154-160. https://doi.org/10.7861/fhj.2022-0006.
Juergens N, Huang J, Gopalan A, Muelly E, Reed M. The association between video or telephone telemedicine visit type and orders in primary care. BMC Med Inform Decis Mak. 2022;22(1):302. https://doi.org/10.1186/s12911-022-02040-z.
US Department of Veterans Affairs. Virtual Health Resource Centers. Available at: https://connectedcare.va.gov/virtual-health-resource-centers. Accessed March 8, 2024.
US Department of Veterans Affairs. Veteran Community Care Eligibility. August 30, 2019. Available at: https://www.va.gov/COMMUNITYCARE/docs/pubfiles/factsheets/VA-FS_CC-Eligibility.pdf. Accessed March 8, 2024.
US Department of Veterans Affairs. Community Care. November 13, 2023. Available at: https://www.va.gov/COMMUNITYCARE/#:~:text=Community%20Care%20Overview,and%20circumstances%20of%20individual%20Veterans. Accessed March 12, 2024.
Schneider C, Aubert CE, Del Giovane C, Donzé JD, Gastens V, Bauer DC, Blum MR, Dalleur O, Henrard S, Knol W, O'Mahony D, Curtin D, Lee SJ, Aujesky D, Rodondi N, Feller M. Comparison of 6 mortality risk scores for prediction of 1-year mortality risk in older adults with multimorbidity. JAMA Netw Open. 2022;5(7):e2223911.
Dev S, Gonzalez AA, Coffing J, Slaven JE, Dev S, Taylor S, Ballard C, Hastings SN, Bravata DM. Validating administratively derived frailty scores for use in Veterans Health Administration emergency departments. Acad Emerg Med. 2023;30(4):349-358.
Siegel M, Critchfield-Jain I, Boykin M, Owens A, Muratore R, Nunn T, Oh J. Racial/ethnic disparities in state-level COVID-19 vaccination rates and their association with structural racism. J Racial Ethn Health Disparities. 2022;9(6):2361-2374.
Javed Z, Haisum Maqsood M, Yahya T, Amin Z, Acquah I, Valero-Elizondo J, Andrieni J, Dubey P, Jackson RK, Daffin MA, Cainzos-Achirica M, Hyder AA, Nasir K. Race, Racism, and Cardiovascular Health: Applying a Social Determinants of Health Framework to Racial/Ethnic Disparities in Cardiovascular Disease. Circ Cardiovasc Qual Outcomes. 2022 Jan;15(1):e007917.
Clinical Resource Hubs. Department of Veterans Affairs. https://www.patientcare.va.gov/primarycare/CRH.asp. Accessed October 17, 2023.
Kobe EA, Lewinski AA, Jeffreys AS, Smith VA, Coffman CJ, Danus SM, Sidoli E, Greck BD, Horne L, Saxon DR, Shook S, Aguirre LE, Esquibel MG, Evenson C, Elizagaray C, Nelson V, Zeek A, Weppner WG, Scodellaro S, Perdew CJ, Jackson GL, Steinhauser K, Bosworth HB, Edelman D, Crowley MJ. Implementation of an intensive telehealth intervention for rural patients with clinic-refractory diabetes. J Gen Intern Med. 2022;37(12):3080-3088.
Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood). 2021;40(3):487-495.
Samuels-Kalow M, Jaffe T, Zachrison K. Digital disparities: designing telemedicine systems with a health equity aim. Emerg Med J. 2021;38(6):474-476.
Fortney JC, Burgess JF Jr, Bosworth HB, Booth BM, Kaboli PJ. A re-conceptualization of access for 21st century healthcare. J Gen Intern Med. 2011;26 Suppl 2(Suppl 2):639-47.
US Department of Health and Human Services. COVID-19 Public Health Emergency. December 15, 2023. Available at: https://www.hhs.gov/coronavirus/covid-19-public-health-emergency/index.html#:~:text=The%20federal%20Public%20Health%20Emergency,remains%20a%20public%20health%20priority. Accessed March 8, 2024.
Wong ES, Wang V, Liu CF, Hebert PL, Maciejewski ML. Do veterans health administration enrollees generalize to other populations? Med Care Res Rev. 2016;73(4):493-507.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations: Research included in this article was presented as a poster at the North American Primary Care Research Group 2023 Annual Meeting on November 1, 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Staloff, J., Gunnink, E., Rojas, J. et al. Identifying Patterns of Primary Care In-Person and Telemedicine Use in the Veterans Health Administration: A Latent Class Analysis. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-024-08751-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-024-08751-5