Abstract
Background
Prevalence of smoking is high among patients receiving care in safety-net settings, and there is a need to better understand patient factors associated with smoking cessation and receipt of cessation services.
Objective
To identify patient factors associated with smoking cessation attempts and receipt of cessation counseling and pharmacotherapy in a large safety-net health system.
Design
We conducted a retrospective cohort analysis using EHR data in a safety-net system in San Francisco, CA.
Participants
We included 7384 adult current smokers who had at least three unique primary care encounters with documented smoking status between August 2019 and April 2022.
Main measures
We assessed four outcomes using multivariate generalized estimating equation models: (1) any cessation attempt, indicating a transition in smoking status from “current smoker” to “former smoker”; (2) sustained cessation, defined as transition in smoking status from current smoker to former smokers for two or more consecutive visits; (3) receipt of smoking cessation counseling from healthcare providers; and (4) receipt of pharmacotherapy.
Key Results
Of 7384 current adult smokers, 17.6% had made any cessation attempt, and of those 66.5% had sustained cessation. Most patients (81.1%) received counseling and 41.8% received pharmacotherapy. Factors associated with lower odds of any cessation attempt included being aged 45–64, non-Hispanic black, and experiencing homelessness. The factor associated with lower odds of sustained cessation was being male. Factors associated with lower odds of receiving counseling were being insured by Medicaid or being uninsured. Factors associated with lower odds of receiving pharmacotherapy included speaking languages other than English, being male, and identifying as racial and ethnic minorities.
Conclusions
Health system interventions could close the gap in access to smoking cessation services for unhoused and racial/ethnic minority patients in safety-net settings, thereby increasing cessation among these populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Cigarette smoking prevalence among adults in the United States (US) has been declining, with a prevalence of 20.9% in 2005 to 11.5% in 2021.1,2 Despite this improvement, smoking is concentrated among priority populations.2 In 2021, smoking prevalence was higher among low-income adults (18.3%) and those uninsured (20.0%) or insured by Medicaid (21.5%) compared to their counterparts. 2
Tobacco use remains the leading preventable cause of morbidity and mortality, contributing to over 60% of annual healthcare costs covered by Medicare and Medicaid.3 A 1% reduction of smoking prevalence is associated with $2.5 billion in annual Medicaid savings.4 Safety-net health systems are the primary source of low or no-cost healthcare for low-income populations. Improving access to smoking cessation care in safety-net settings can reduce tobacco-related health disparities.5 Cessation interventions that have included engagement with quitline or in-person tobacco treatment have shown cost savings for safety-net practices6 and patients insured by Medicaid.7
Within health systems, healthcare providers can help people who smoke to quit by using guideline-recommended 5As for smoking cessation (Ask, Advise, Assess, Assist, and Arrange) and pharmacotherapy.8 While most providers Ask, Advise, and Assess for tobacco use, the proportion of providers assisting with quit attempts and arranging for follow-up is much lower.9 Digital interventions including reminders in the electronic health record (EHR) have increased provider delivery of 5As.10 Moreover, medical teams can use the EHR to receive automatic reminders for tobacco screening,11 refer for smoking cessation services (e.g., behavioral counseling and pharmacotherapy),12 and monitor receipt of services.13,14
Starting in 2009, the federal government put into effect the Meaningful Use criteria, where healthcare systems that had implemented an EHR could receive annual incentive payments from the Centers for Medicare and Medicaid if they met tobacco screening and referral targets.15 The implementation of the Meaningful Use EHR guideline for tobacco screening and treatment was associated with an increase in receipt of cessation services among patients who smoked in some health systems.16,17,18
However, only a few studies used the EHR to assess patient characteristics associated with cessation behaviors and receipt of cessation services in safety-net settings.9,17,19,20 The results varied depending on the clinical setting and patient population. A study using 2014–2016 EHR data from safety-net clinics in the Oregon Community Health Information Network showed that Medicare patients were less likely to receive counseling and racial and ethnic minorities were less likely to have cessation medications prescribed.17 In an EHR-based study from the San Francisco Health Network, a network of safety-net clinics in San Francisco, California, uninsured or patients insured by Medicaid were less likely to receive cessation counseling.19 In the same setting, patients who were older, were insured by Medicaid or uninsured, and had limited English proficiency had a lower likelihood of quit attempts.20
These studies were done before the COVID-19 pandemic when most cessation services were provided in-person. However, since the pandemic, health systems, including the San Francisco Health Network, have transitioned to providing tobacco treatment using telehealth models of care.21 In this study, we extend our prior work19,20 by describing previously unexplored patient factors associated with receipt of cessation services, quit attempts, and sustained cessation during the pandemic. Social determinants of health like housing are linked with tobacco use,22 and we were able to obtain information on housing status for the present analysis. Our study has two objectives: (1) describe the proportion of smoking cessation attempts, sustained cessation, and receipt of cessation services (counseling and pharmacotherapy) among adult smokers in primary care clinics within the San Francisco Health Network; and (2) identify patient factors associated with those outcomes. We hypothesized that unhoused populations would be less likely to have any cessation and sustained cessation attempts compared to housed populations.
METHODS
Study Design and Data Source
We conducted a retrospective cohort study between August 2019 and April 2022 using EHR data from adult patients in 12 primary care clinics within the San Francisco Health Network, a network of primary care clinics that serve San Francisco’s diverse low-income populations. The population includes residents who are low- or very low–income including those experiencing homelessness, and who represent the age, sex, and racial/ethnic diversity of people living in San Francisco. Three clinics were academic primary care practices in a safety-net hospital; the remaining clinics were community-based clinics in San Francisco. At each clinic visit, medical assistants screen patients for current smoking, and document smoking status in EHR as “current smoker,” “former smoker,” or “never smoker.” Medical assistants refer all current smokers to cessation resources (e.g., quitline, or on-site referrals to the medical team), and document referrals within EHR. The medical team, including health care providers and behavioral health care staff, provides tobacco treatment and documents provision of smoking cessation counseling and/or pharmacotherapy during clinical encounters. We extracted data using Structured Query Language (SQL) from the EHR on any patient of the 12 clinics who had at least three unique primary care encounters with documented smoking status between April 2019 and April 2022. The index visit was the first encounter closest to the study’s start date in April 2019. This study was approved by the University of California, San Francisco Committee on Human Research (#18–26,398).
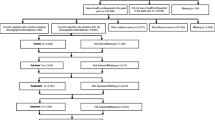
Ascertainment of Study Cohort
We included adult patients who were aged 18 or over and had at least three unique primary care encounters with documented smoking status. We identified current smokers based on their recorded smoking status at the index visit. Patients could have at minimum three visits and up to nine visits with a documented smoking status throughout the study duration.
Outcome Variables
The two binary smoking cessation outcomes were (1) any cessation attempt, defined as a transition in smoking status from “current smoker” at the index visit to “former smoker” at any of the subsequent visits, and (2) sustained cessation, defined as transition in smoking status from current smoker at the index visit to former smokers for two or more consecutive visits until the end of the study. The two binary cessation services outcomes for current smokers were (1) receipt of smoking cessation counseling from one or more members of the medical team (i.e., health care provider, medical assistant, or behavioral health staff) at any visit, and (2) receipt of pharmacotherapy including nicotine replacement therapy (NRT) and/or non-NRT at any visit.
Independent Variables
We assessed independent variables at the patients’ index visit including patient demographics (age [18–44, 45–64, 65 +],19,20 sex [male vs. female], race/ethnicity [non-Hispanic White [NHW], Hispanic, non-Hispanic Black [NHB], non-Hispanic Asian [NHA], and non-Hispanic other [NHO]], and primary language), social determinants of health (health insurance and housing status [experiencing homelessness or housed]), and comorbidity burden (number of smoking-related comorbidities [0, 1, 2, ≥ 3] including heart failure, chronic obstructive pulmonary disease, kidney disease, coronary artery disease, depression, diabetes, HIV, hyperlipidemia, and hypertension). We identified comorbidities using ICD-10 codes.20 We included intensity of primary care (number of visits during the study period) in the models exploring cessation outcomes.
Statistical Analysis
First, we used bivariate analysis χ2 tests to examine the association of independent and cluster variables with each outcome. Then, to determine factors associated with each outcome, we conducted four separate generalized estimating equation (GEE) logistic models, accounting for clustering within the two clinic types (academic vs. community) with an exchangeable structure in each model. We clustered by clinic because patient populations seeking care in academic and community clinics had different demographic characteristics that might be relevant to tobacco use.20 The four models estimating the odds of any cessation attempt (model 1), sustained cessation (model 2), receipt of any cessation counseling (model 3), and receipt of pharmacotherapy (model 4) controlled for independent variables from the index visit. Models 1, 3, and 4 were conducted among all current smokers and model 2 was conducted among current smokers who had any cessation attempt. We did not include receipt of cessation services as variables in the models of any cessation attempt or sustained cessation because these services were provided only to patients who were current smokers. Including them in the models would erroneously suggest that current smokers who received cessation services were less likely to quit smoking. To account for time-lapsed between visits, we included average time between visits as a variable in the model for sustained cessation and found no association between sustained cessation and length of time between visits. We chose not to include this variable in the sustained cessation model. All analyses were performed using SAS V.9.4 (SAS Institute, Cary, NC, USA). Estimates were considered to be statistically significant if the two-tailed p < 0.05.
RESULTS
The analytic sample included 7384 adult patients who were current smokers. We excluded 71 patients with incomplete information for the outcome and independent variables. Of the 7384 adult patients who were current smokers, 1302 (17.6%) made any cessation attempt. Of those who made any cessation attempt, 866 (66.5%) made a sustained cessation attempt.
Sample Characteristics and Factors Associated with Cessation Outcomes
Patients who were younger, identified as Hispanic/Latino, were non-English speaking, had Healthy San Francisco/Healthy Workers coverage, and were housed were more likely to make any cessation attempt (Table 1). In multivariable analysis, being Hispanic (adjusted odds ratio [AOR] 1.53, 95% confidence interval [CI] 1.26–1.86) and number of visits (AOR 1.28, 95%CI 1.24–1.32) were associated with higher odds of making any cessation attempt (Table 2). Factors associated with lower odds of any cessation attempt included older age (45–64 years) (AOR 0.75, 95%CI 0.64–0.87), being NHB (AOR 0.82, 95%CI 0.68–0.97), and experiencing homelessness (AOR 0.53, 95%CI 0.45–0.63). Being male was associated with lower odds of sustained cessation (AOR 0.75, 95%CI 0.58–0.96; Table 2), while number of visits (AOR 1.11, 95%CI 1.04–1.19) was associated with higher odds.
Sample Characteristics and Factors Associated with Receipt of Cessation Services
Most patients who were current smokers received counseling or pharmacotherapy during one or more of their encounters. Among all encounters with counseling, 67% were offered by medical assistants, 0.3% by behavioral health providers, and 33% by healthcare providers (data not shown). Of the 7384 current smokers, 5985 (81.1%) received any counseling and 3088 (41.8%) received pharmacotherapy (Table 3). For receipt of both cessation services, statistically significant differences were found for similar characteristics, except for homelessness status which was not associated with receipt of counseling (Table 3). In multivariable analyses, factors associated with receipt of any counseling and pharmacotherapy were older age (45–64 years) (AOR 1.35, 95%CI 1.17–1.56) and having more comorbidities (Table 4). Factors associated with lower odds of receiving any cessation counseling included having Medicaid (AOR 0.79, 95%CI 0.66–0.95), being uninsured/self-paid (AOR 0.70, 95%CI 0.49–0.99), and having commercial/other insurances (AOR 0.58, 95%CI 0.34–0.98) compared to having “Healthy San Francisco and Healthy Workers.” In contrast, factors associated with higher odds of receiving pharmacotherapy included having Medicare (AOR 1.31, 95%CI 1.12–1.52) and Medicaid (AOR 1.32, 95%CI 1.10–1.60). Being male (AOR 0.87, 95%CI 0.78–0.96), speaking a language other than English (AOR 0.66, 95% CI 0.56–0.77), and being NHA (AOR 0.61, 95%CI 0.51–0.73), NHB (AOR 0.7, 95%CI 0.7–0.90), and NHO (AOR 0.77, 95%CI 0.64–0.93) were factors associated with lower odds of receiving pharmacotherapy.
DISCUSSION
In this retrospective study of patients seeking primary care in a safety-net health system, we found that 17.6% of patients who smoked attempted to quit smoking, and of those who attempted to quit, 66.5% were able to sustain their quit attempt across two or more visits. Most patients who smoked received cessation counseling, and about half received pharmacotherapy. Quit attempt rates were higher than the spontaneous population-level quitting rate of 5%, but lower than the 30–40% quitting rate observed in 8–12-week clinical trials of behavioral counseling and pharmacotherapy.23
In a previous study conducted between 2016 and 2019 in the San Francisco Health Network that examined smoking status across three primary care visits, 26.5% of patients attempted any cessation attempt, and 34% of those who attempted to quit smoking had sustained cessation.20 In a related cross-sectional study with a similar population focusing on four safety-net clinics, 17.6% had made any cessation attempt.19 The difference in any cessation attempts may be due to unmeasured factors like change in patient population between studies, and the increase in any sustained attempts may be due to following patients over longer periods of time.19,20 The present study showed a higher rate of sustained cessation with a stricter measure, a marker of long-term quitting,24 and highlighted that most patients were receiving at least one cessation intervention during one or more routine primary care visits. Patients who had a greater number of visits were more likely to make a quit attempt and achieve sustained abstinence.
In the year prior to and during the time of COVID-19 pandemic, the SFHN implemented several quality improvement initiatives to support tobacco treatment efforts,21 including a tobacco coordinator who trained clinic staff on how to outreach to patients who smoked, use tobacco registries, implement practice changes in delivering tobacco treatment, and document these interventions in the EHR.21 The SFHN also had a robust IT infrastructure that helped transition the health system from an in-person model of healthcare delivery to telehealth model, including for tobacco treatment.21 These initiatives may have played a role in increasing patients’ receipt of tobacco treatment, and in turn, their attempts to quit smoking.
Our study highlighted several patient groups that could benefit from expanded and intensive tobacco treatment efforts. People experiencing homelessness had a lower likelihood of any cessation attempts. People experiencing homelessness have high rates of tobacco use, with a prevalence of 70%, but rates of successful cessation are low.22,25 In our study, we found that compared to housed individuals, fewer people who were homeless were making any cessation attempts and there was no association with sustained cessation. Our findings suggest that once an attempt is initiated, people experiencing homelessness were no different in sustaining that attempt compared to those who were housed. Therefore, there may be a role for interventions within EHR to increase motivation to quit.26
Our study found that male patients were less likely to sustain their cessation compared to women. Men have been shown to have higher nicotine dependence than women,27 which is a known barrier to cessation.28,29 NHB patients were less likely to make any attempts compared to NHW patients.30 Despite smoking at lower rates, NHB patients who smoke have higher levels of nicotine dependence. They are less likely to quit successfully despite making more quit attempts than White smokers.31 They may also experience barriers to receiving tobacco treatment,32 which we observed in our study and could explain their lower cessation attempt rate. Tobacco retail density tends to be higher in communities where NHB populations reside; the increased availability of tobacco products may influence cessation rates. EHR reminders, although potentially contributing to provider fatigue,33 and tobacco registries that systematically address equity gaps may mitigate racial/ethnic disparities in access to tobacco treatment,21 may in turn increase cessation attempts.
Patients who were insured by Medicare and Medicaid were more likely to receive cessation pharmacotherapy—a covered benefit—than those covered through Healthy San Francisco where there may have been coverage gaps. In contrast, patients covered through Healthy San Francisco/Healthy Workers were more likely to receive counseling than those on Medicaid. While these findings are consistent with those in our prior study,19 they are paradoxical as we expect that Medicaid and Medicare would similarly cover counseling and pharmacotherapy interventions. We speculate that certain omitted variable correlated with one of the cessation services and health insurance coverage affected the direction of this relationship. One of the omitted variables could be providers’ awareness of services covered; most providers may be aware that insurance covers pharmacotherapy but may be less aware that counseling is also a covered benefit. The mechanism of the relationship between health insurance coverage and the receipt of different cessation services warrants further investigation. There may be a need for provider education on the newer recommendations for varenicline34 and/or combination NRT for cessation pharmacotherapy.34
Racial/ethnic minorities and non-English speaking patients had lower odds of receiving pharmacotherapy. Racial and ethnic minorities tend to have lower rates of pharmacotherapy prescribed than White patients35 due to competing priorities among patients and providers, low rates of provider adherence to tobacco treatment guidelines, and implicit bias around adherence to pharmacotherapy among providers of non-White patients.35 These barriers may be addressed by creating equity or care gap reminders within the EHR to encourage practice changes around tobacco treatment. Providing education to patients on the benefits of tobacco treatment in a culturally and linguistically concordant manner may also dispel some of the misconceptions around the use of cessation medications among racial/ethnic minority groups.36,37
Consistent with our previous studies,19,20 medical assistants delivered counseling at higher rates than behavioral health and healthcare providers. This is normative in team-based care settings where the ownership of providing tobacco treatment is distributed among the medical team. However, our results also suggest that while medical assistants may provide the initial referral to treatment, behavioral health and healthcare providers’ support could be enlisted for subpopulation of patients highlighted in this analysis who may benefit from intensive treatments.
Our study had limitations. First, EHR smoking status was based on self-report, potentially resulting in classification errors. Self-report measurements of smoking status have high sensitivity and specificity compared to biochemical validation;38 we expect the misclassification rate to be low.13,20 Second, nicotine dependence measures were not included in the EHR, highlighting a potential gap in EHR measurements of tobacco use status, which may impact practice changes in prescribing pharmacotherapy. Third, cessation behaviors and service receipt in SFHN may vary from that in other safety-net systems in other geographic areas; therefore, our results may lack external generalizability. Fourth, all the outcomes of interest in the four models were not relatively rare (> 10%), so the AORs in our results might have led to an overestimation of the association strength.39 Fifth, because EHR data reflect data captured from clinical encounters, we can only ascertain if and when quitting took place. We are unable to determine whether a lack of transition from current to past smoking was because of lack of motivation to quit or a failed quit attempt. Sixth, we were unable to assess delivery of cessation services between telehealth and in-person encounters, warranting further research to analyze patient characteristics across different methods of delivery.
CONCLUSION
This study identified subpopulations that could benefit from tailored intensive cessation interventions during primary care. The EHR is a good tool to assess provision of guideline-recommended tobacco treatment to meet performance-based incentive programs for healthcare systems. It is also an effective tool to identify tobacco-related disparities in healthcare settings, allowing healthcare providers and health systems to tailor tobacco treatment to those groups that have the highest gaps in receipt of cessation services. The EHR has the potential to expand collection of social determinants of health metrics, which could provide a deeper understanding of the context of tobacco use and the extent to which tobacco treatment services are reaching disproportionately impacted populations.
References
Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current Cigarette Smoking Among Adults - United States, 2005-2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205-11.
Cornelius ME, Loretan CG, Jamal A, et al. Tobacco product use among adults - United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(18):475-83.
Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: an update. Am J Prev Med. 2015;48(3):326-33.
Glantz SA. Estimation of 1-year changes in Medicaid expenditures associated with reducing cigarette smoking prevalence by 1%. JAMA Netw Open. 2019;2(4):e192307.
Krist AH, Davidson KW, Mangione CM, et al. Interventions for tobacco smoking cessation in adults, including pregnant persons. JAMA. 2021;325(3):265.
Drouin O, Sato R, Drehmer JE, et al. Cost-effectiveness of a smoking cessation intervention for parents in pediatric primary care. JAMA Netw Open. 2021;4(4):e213927.
Mundt MP, Baker TB, Fraser DL, Smith SS, Piper ME, Fiore MC. Paying low-income smokers to quit? The cost-effectiveness of incentivizing tobacco quit line engagement for Medicaid recipients who smoke. Value Health. 2019;22(2):177-84.
Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update US Public Health Service Clinical Practice Guideline executive summary. Respir Care. 2008;53(9):1217-22.
Vijayaraghavan M, Yuan P, Gregorich S, et al. Disparities in receipt of 5As for smoking cessation in diverse primary care and HIV clinics. Prev Med Rep. 2017;6:80-7.
Satterfield JM, Gregorich SE, Kalkhoran S, et al. Computer-facilitated 5A’s for smoking cessation: a randomized trial of technology to promote provider adherence. Am J Prev Med. 2018;55(1):35-43.
Bae J, Ford EW, Kharrazi HHK, Huerta TR. Electronic medical record reminders and smoking cessation activities in primary care. Addict Behav. 2018;77:203-9.
Schindler-Ruwisch JM, Abroms LC, Bernstein SL, Heminger CL. A content analysis of electronic health record (EHR) functionality to support tobacco treatment. Transl Behav Med. 2017;7(2):148-56.
Gubner NR, Williams DD, Chen E, et al. Recent cessation attempts and receipt of cessation services among a diverse primary care population – a mixed methods study. Prev Med Rep. 2019;15:100907.
Bae J, Ford EW, Huerta TR. The electronic medical record’s role in support of smoking cessation activities. Nicotine Tobacco Res. 2016;18(5):1019-24.
Blumenthal D, Tavenner M. The “Meaningful Use” regulation for electronic health records. N Engl J Med. 2010;363(6):501-4.
Tan ASL, Young-Wolff KC, Carter-Harris L, Salloum RG, Banerjee SC. Disparities in the receipt of tobacco treatment counseling within the US context of the Affordable Care Act and Meaningful Use implementation. Nicotine Tob Res. 2018;20(12):1474-80.
Bailey SR, Heintzman JD, Marino M, et al. Smoking-cessation assistance: Before and after stage 1 Meaningful Use implementation. Am J Prev Med. 2017;53(2):192-200.
Silfen SL, Farley SM, Shih SC, et al. Increases in smoking cessation interventions after a feedback and improvement initiative using electronic health records -- 19 community health centers, New York City, October 2010-March 2012. MMWR Morb Mortal Wkly Rep. 2014;63(41):921-4.
Gubner NR, Williams DD, Chen E, et al. Recent cessation attempts and receipt of cessation services among a diverse primary care population - a mixed methods study. Prev Med Rep. 2019;15:100907.
Suen LW, Rafferty H, Le T, et al. Factors associated with smoking cessation attempts in a public, safety-net primary care system. Prev Med Rep. 2022;26:101699.
Chung K, Rafferty H, Suen LW, Vijayaraghavan M. System-level quality improvement initiatives for tobacco use in a safety-net health system during the COVID-19 pandemic. J Prim Care Community Health. 2022;13:21501319221107984.
Baggett TP, Tobey ML, Rigotti NA. Tobacco use among homeless people--addressing the neglected addiction. N Engl J Med. 2013;369(3):201-4.
Fiore MC, Jaén C, Baker T, et al. Treating tobacco use and dependence: 2008 update. Clinical Practice Guideline. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 2008.
Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst. 1997;89(8):572-6.
Vijayaraghavan M, Elser H, Frazer K, Lindson N, Apollonio D. Interventions to reduce tobacco use in people experiencing homelessness. Cochrane Database Syst Rev. 2020;12:CD013413.
Carpenter MJ, Alberg AJ, Gray KM, Saladin ME. Motivating the unmotivated for health behavior change: a randomized trial of cessation induction for smokers. Clin Trials. 2010;7(2):157-66.
Shiffman S, Paton SM. Individual differences in smoking: gender and nicotine addiction. Nicotine Tob Res. 1999;1 Suppl 2:S153-7; discussion S65-6.
Baker TB, Piper ME, McCarthy DE, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tob Res. 2007;9 Suppl 4(Suppl 4):S555-70.
Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6 Suppl 3:S363-9.
Hooper MW, Larry R, Okuyemi K, et al. Culturally specific versus standard group cognitive behavioral therapy for smoking cessation among African Americans: an RCT protocol. BMC Psychol. 2013;1(1):15.
Bacio GA, Guzman IY, Shapiro JR, Ray LA. Differences in quit attempts between non-Hispanic Black and White daily smokers: the role of smoking motives. Addict Behav. 2014;39(12):1769-72.
Houston TK, Scarinci IC, Person SD, Greene PG. Patient smoking cessation advice by health care providers: the role of ethnicity, socioeconomic status, and health. Am J Public Health. 2005;95(6):1056-61.
McGreevey JD, 3rd, Mallozzi CP, Perkins RM, Shelov E, Schreiber R. Reducing alert burden in electronic health records: state of the art recommendations from four health systems. Appl Clin Inform. 2020;11(1):1-12.
Rigotti NA, Kruse GR, Livingstone-Banks J, Hartmann-Boyce J. Treatment of tobacco smoking: a review. JAMA. 2022;327(6):566-77.
Hooper MW, Payne M, Parkinson KA. Tobacco cessation pharmacotherapy use among racial/ethnic minorities in the United States: considerations for primary care. Fam Med Community Health. 2017;5(3):193-203.
Carpenter MJ, Ford ME, Cartmell K, Alberg AJ. Misperceptions of nicotine replacement therapy within racially and ethnically diverse smokers. J Natl Med Assoc. 2011;103(9-10):885-94.
Amodei N, Lamb RJ. Over-the-counter nicotine replacement therapy: can its impact on smoking cessation be enhanced? Psychol Addict Behav. 2008;22(4):472-85.
Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086-93.
Norton EC, Dowd BE, Maciejewski ML. Odds ratios-current best practice and use. JAMA. 2018;320(1):84-5.
Funding
Tobacco-Related Disease Research Program (28CP-0038) and Division of Cancer Prevention, National Cancer Institute (CA-113710).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gu, D., Rafferty, H. & Vijayaraghavan, M. Factors Associated with Smoking Cessation and the Receipt of Cessation Services in a Public, Safety-Net Primary Care System. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-024-08664-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-024-08664-3