Abstract
Background
Policy initiatives have attempted to reduce healthcare inequalities in the USA, but evidence on whether these initiatives have reduced racial and ethnic disparities in pain treatment in primary care is lacking.
Objective
To determine whether racial and ethnic disparities in medication prescribed for pain in primary care settings have diminished over a 21-year period from 1999 to 2019.
Design
An annual, representative cross-sectional probability sample of visits to US primary care physicians, taken from the National Ambulatory Medical Care Survey.
Patients
Pain-related visits to primary care physicians.
Main Measures
Prescriptions for opioid and non-opioid analgesics.
Key Results
Of 599,293 (16%) sampled visits, 94,422 were pain-related, representing a population-weighted estimate of 143 million visits made annually to primary care physicians for pain. Relative risk analysis controlling for insurance, pain type, and other potential confounds showed no difference in pain medication prescribed between Black and White patients (p = .121). However, White patients were 1.61 (95% CI 1.32–1.97) and Black patients 1.57 (95% CI 1.26–1.95) times more likely to be prescribed opioids than a more underrepresented group consisting of Asian, Native-Hawaiian/Pacific-Islander, and American-Indian/Alaska-Natives (ps < .001). Non-Hispanic/Latino patients were 1.32 (95% CI 1.18–1.45) times more likely to receive opioids for pain than Hispanic/Latino patients (p < .001). Penalized cubic spline regression found no substantive narrowing of disparities over time.
Conclusions
These findings suggest that additional intervention strategies, or better implementation of existing strategies, are needed to eliminate ethnic and racial disparities in pain treatment towards the goal of equitable healthcare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
A landmark Institute of Medicine (IOM) report commissioned by the US Congress over two decades ago documented inequities in healthcare1 and highlighted racial and ethnic disparities in pain treatment.2 Such disparities have been consistently demonstrated in the emergency department (ED) with Black, Asian, and Hispanic patients markedly less likely to receive opioid medication than White and non-Hispanic patients.3 Disparities in pain medication prescribed in primary care settings have also been examined, with such settings differing to the ED in immediacy of access, consultation time, perceived care quality and proportion of chronic pain patients.1 Black and Hispanic patients are also less likely than White patients to have a primary care provider and more commonly use the ED for pain treatment.4,5 Several national studies of primary care settings have found Hispanic patients to be less likely to be prescribed opioid analgesics6,7,8,9,10 or to receive lower dosages11 typically even after controlling for potential confounds such as insurance status, pain condition, and region. Similar findings have been reported for Black patients in some7,9 but not other8,11 studies, with limited research on racially underrepresented groups such as Asian, Native-Hawaiian/Pacific-Islander (NHPI), and American-Indian/Alaska-Natives (AIAN).
Despite broad political and regulatory initiatives12 for promoting equitable healthcare, such as the Affordable Care Act,13 it is unclear to what extent these have impacted inequities across racial and ethnic groups in pain care. One study7 of US national primary care data found that the lower rate of opioid prescriptions for back and abdominal pain in Hispanic and Black compared to non-Hispanic White patients was similar across data averaged within 2006–2010 and 2011–2015 time periods. However, there is no clear picture on the extent to which disparities have systematically changed over time since the commissioning of the IOM report on health inequalities in 19991 and which includes the period from 2016 when significant changes were made to opioid prescribing guidelines.14
The current study examines racial and ethnic disparities in pain medication prescribed in US primary care settings across a 21-year period from 1999 to the latest available patient data provided by the Centers for Disease Control in 2019. Based on previous findings, we hypothesize that White patients are more frequently prescribed opioids for pain than Black patients or an underrepresented group consisting of Asian, Native-Hawaiian/Pacific-Islander (NHPI), and American-Indian/Alaska-Natives (AIAN), and non-Hispanic/Latino patients are more frequently prescribed opioids than Hispanic/Latino patients. While disparities are expected to vary over the study period, no predictions are made on the direction of changes given a lack of previous data.
METHOD
Study Design and Setting
This study examines patient record data from the National Ambulatory Medical Care Survey (NAMCS) and is reported in accordance with STROBE guidelines (Appendix A). The NAMCS is an annual probability sample of patient visits to non-federally employed office-based physicians in the USA administered by the National Center for Health Statistics (NCHS). A detailed description of the sampling methods is available elsewhere.15 In brief, a multistage probability design is used, with ~ 1300 physicians randomly sampled from within geographical strata. The physician and/or supporting staff record data from ~ 30 randomly selected patient visits over a 1-week reporting period, which includes patient demographics, medications prescribed, and reasons for visit. Patients’ reasons for visit are recorded verbatim and subsequently reclassified by medical coders who assign up to three reason-for-visit classes using the NCHS standardized classification system.15 Coding accuracy is subject to independent quality control procedures and error rates are typically < 1%.15
Study Sample
Records for pain-related visits were identified from NAMCS datasets spanning 1999–2019, except for 2017 which is not yet released due to COVID-related processing delays. A visit was categorized as pain-related if the patient’s main reason-for-visit code matched any of the classification codes15 relating to pain (Appendix B). Data were combined across different annual survey waves as described in Appendix C.
Race and Ethnicity
Race and ethnicity are abstracted directly from patient medical records in the NAMCS and categorized based on National Institute of Health reporting standards. For ethnicity, two categories are used: Hispanic/Latino and not Hispanic/Latino. For race, five categories are used: White, Black/African-American, Asian, Native-Hawaiian/Pacific-Islander (NHPI), and American-Indian/Alaska-Native (AIAN). A NAMCS-recoded three-category variable of White, Black, and Other Race (Asian, NHPI, AIAN) is provided for analysis given prohibitively small sample sizes for NHPI and AIAN subgroups and is employed in the current study. Appendix D gives full definitions of race and ethnicity categories.
As missing data are high for race and ethnicity (25.5% and 22.7% in the current data), NAMCS provides imputed variables for each survey year (except for ethnicity in 1999–2002 surveys). Imputation involves a model-based sequential regression using key predictors described in detail elsewhere.15
Outcomes
Two binary outcomes were used: whether opioids were prescribed (yes/no), and (ii) whether non-opioid analgesics only were prescribed (yes/no). Opioids were indicated if any prescribed medication had a Multum16 class of 575860 (narcotic analgesics) or 5758191 (narcotic analgesic combinations). Non-opioid analgesics only were indicated if any medications matched classes 575861 (NSAIDs), 575862 (salicylates), or 5758278 (cox-2 inhibitors) and none matched an opioid class. If a patient’s medication matched class 575863 (general analgesic combinations), ingredient codes were examined to determine medication type.
Model Covariates
To assess the independent association of race and ethnicity with medication outcomes, we included several covariates commonly previously examined in studies of racial and ethnic disparities and that may influence opioid prescribing.17 These included patient sex, age, insurance (private/Medicaid/Medicare/none/unknown), pain chronicity (acute/chronic/pre- or post-surgery/preventive), and new patient status (new/existing). We also controlled for alcohol and substance misuse/dependence (Appendix E) as these may influence physicians’ willingness to prescribe opioids. In addition, we controlled for pain type, after recoding 53 identified pain codes into eight broader classes of musculoskeletal, abdominal, chest (excluding heart), headache, eye/ear, dental, genitourinary, and other pain (Appendix E). Practice characteristics controlled for were census region (Northeast/Midwest/South/West) and metropolitan status (metropolitan/non-metropolitan). Finally, we included survey year and age as first-degree (linear) and second-degree (quadratic) orthogonal polynomials based on previously observed relationships.18
Statistical Analysis
We examined racial and ethnic differences in prescribed medication using log-link Poisson regression to estimate both crude relative risks (RRs), and adjusted RRs after including all covariates. Race and ethnicity were dummy coded19 with White and Hispanic/Latino used as reference groups. To obtain a direct comparison of the non-reference groups for race (Black and Other Race), we reran the analysis after re-referencing to Other Race.
To determine whether the magnitude of race disparities changed across survey years in a linear or quadratic fashion, we added first then second-degree Race × Date interaction terms and sequentially assessed change in model fit with likelihood ratio tests. This procedure was repeated for ethnicity. To explore any possible more complex non-linear trends, we also performed regression using natural cubic splines,20 fitting a series of smoothed local polynomial regressions across equally spaced time intervals. If this suggested an obvious pattern of higher-order changes in disparities across time, we reran initial models adding the appropriate polynomial interactions.
Analyses were performed with the survey package21 in R using NAMCS-provided patient weights to compute nationally representative estimates and sampling unit design variables to adjust for clustering. Multiple visits by the same patient are not identifiable in NAMCS data, but the 1-week recording period means repeated visits should be relatively uncommon and introduce little additional non-independence.
In accordance with NCHS guidelines,15 statistical significance was set to α = 0.01 to reduce type I error rate.
Sensitivity Analysis
Although NAMCS imputation of missing race and ethnicity data would seem unlikely to introduce large systematic bias, we nevertheless examined alternative imputations. We applied the principles of threshold analysis22 to examine what the true pattern in the missing/imputed data would need to be to nullify group differences, so that reasonable judgements can be made about whether such patterns in the missing data are plausible.
For ethnicity, we iteratively replaced NAMCS-imputed ethnicity data (N = 23,182) within the whole dataset (N = 94,421) with simulated data representing a range of relative risks. We then reran the main analysis on each whole dataset and from these analyses, identified the least extreme relative risk in the simulated/missing data that resulted in ethnicity becoming non-significant. The same procedure was performed for race. Given that relative risks for Black and White (vs. Other Race) were similar in the main analysis, relative risks for these comparisons were constrained to be equal in each simulation to reduce computational time.
RESULTS
Demographic and Clinical Characteristics of Pain-Related Visits
Of 599,293 NAMCS patient records, 94,422 were classified as pain-related, representing a population-weighted estimate of over 143 million annual primary care visits for pain (eTable 1), or 16% of all physician visits. Musculoskeletal, “other” (primarily post-operative), and abdominal pain were the most common types of pain for all racial and ethnic groups (eFigure 1). Racial and ethnic composition of visits was White (85%), Black (10%), Other Race (5%), and non-Hispanic/Latino (88%), Hispanic/Latino (12%).
Visits characteristics are shown in Table 1, with statistically significant differences (p < 0.01) within racial and ethnic groups observed for all characteristics except substance and alcohol misuse/dependence. Differences were generally small, with type of pain (eFigure 1), sex, chronicity, and new patient status showing a similar distribution for each group. More marked dissimilarities were evident for insurance, age, and geographic region. Black and Hispanic patients were twice as likely, and Other Race around 1.5 times as likely, to be Medicaid beneficiaries compared to White and non-Hispanic/Latino patients. Black and Hispanic/Latino patients also had a notably lower representation of ≥ 65-year-old adults compared to all other groups.
Opioid Medication
Population-weighted relative risks of medication receipt are shown in Table 2. The probability of receiving an opioid prescription for pain was 1.32 [95% CI 1.19–1.47] times greater for non-Hispanic/Latino (14.8%, 95% CI 14.1–15.6%) compared to Hispanic/Latino (11.2%, 95% CI 10.0–12.4%) patients (p < 0.001). Black patients were 1.60 [95% CI 1.33–1.92] times as likely and White patients 1.48 [95% CI 1.27–1.74] times as likely to be prescribed opioids than those from the Other Race group (p < 0.001). Overall probability of opioid receipt was 15.6% [95% CI 14.2–17.1%] for Black, 14.5% [95% CI 12.7–15.2%] for White, and 9.7% [95% CI 8.3–11.4%] for Other Race. There were no differences between Black and White patients (RR = 1.08, 95% CI 0.98–1.19, p = 0.121). Adjusted RRs for both ethnicity and race did not change substantively after controlling for covariates (Table 2).
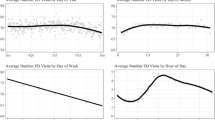
Table 2 also indicates increased opioid prescribing for existing patients, chronic pain patients, certain pain classes, and South and West institutions. Private health insurance was associated with reduced opioid prescribing. A quadratic association of age was also found (eFigure 2), with a peak probability of opioid receipt occurring at around 50 years old.
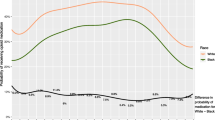
With regard to overall prescribing trends, opioid prescriptions increased from around 10% in 1999 to a peak of 21% in 2013–2014 followed by a rapid decline. However, Fig. 1 (also eTable 2) suggests no substantive change in the magnitude of racial disparities, with the Other Race group showing a consistently lower probability of opioid receipt throughout 1999–2019. This was supported by polynomial regression which found no linear (p = 0.62) or quadratic (p = 0.26) changes in racial disparities across time. Hispanic/Latino patients also showed a consistently lower probability of opioid receipt. While Fig. 1 suggests this discrepancy might narrow slightly from around 2011, no significant linear (p = 0.062) or quadratic (p = 0.081) changes were found.
Opioids most commonly prescribed for all groups were acetaminophen-hydrocodone, tramadol, and acetaminophen-oxycodone (eFigure 3).
Non-opioid Analgesics
The probability of being prescribed non-opioid analgesics only was 1.21 [95% CI 1.11–1.32, p < 0.001] times higher for Hispanic/Latino (21.6%, 95% CI 19.8–22.6%) compared to non-Hispanic/Latino (17.8%, 95% CI 17.2–18.5%) patients. Relative risks did not diminish after controlling for covariates (RR = 1.26 [95% CI 1.16–1.36], p < 0.001). There were no significant differences across Black vs. Other Race (p = 0.48) or White vs. Other Race (p = 0.33), but the proportion of non-opioid analgesic-only prescriptions was significantly higher for Black compared to White patients (RR = 1.15 [95% CI 1.07–1.24], p < 0.001). Table 2 also shows chronic pain, certain pain classes, and older age (eFigure 2) were associated with an increased probability of receiving only non-opioid analgesics.
Figure 2 (also eTable 3) shows a relatively constant rate overall of non-opioid analgesic prescribing until a marked increase around 2012–2013. Although there is some suggestion that this increase is evident primarily for Hispanic/Latino patients, no significant linear (p = 0.297) or quadratic (p = 0.789) effects were found. There were also no linear (p = 0.066) or quadratic (p = 0.617) effects for race. The most common analgesics provided when no opioids were prescribed were Ibuprofen, Aspirin, and Naproxen (eFigure 4).
Sensitivity Analysis
Threshold analysis of NAMCS-imputed data found that, for overall race differences in opioid prescribing to become non-significant, the missing Other Race group would have to have been at least 1.6 and 1.3 times as likely as Black and White patients respectively to receive an opioid prescription. For ethnicity differences to be nullified, missing Hispanic/Latino patients would have to be at least 1.3 times as likely as non-Hispanic/Latinos to receive an opioid prescription. These findings therefore indicate that a strong reversal of direction would have to be present in the missing/imputed data to nullify the significant race and ethnicity differences in the main analyses. We also conducted analysis after excluding NAMCS-imputed data (N = 66,726) and found the same pattern of results, albeit with RRs slightly higher compared to the imputed dataset for Black vs. Other Race (1.95 v 1.60) and White v Other Race (1.80 v 1.48), but with no other differences in RRs.
DISCUSSION
Analysis of 94,422 records of patient visits to US office-based physicians for pain found significant racial and ethnic disparities in prescriptions for opioid medication, with little evidence of any narrowing of these disparities across the 21-year period from 1999 to 2019. Non-Hispanic/Latino patients were 1.32 times as likely overall to be prescribed opioids and 0.79 times as likely to be prescribed only non-opioid analgesics compared to Hispanic/Latinos, after controlling for insurance status, pain type, age, and other variables. White and Black patients were respectively 1.61 and 1.57 times as likely to receive opioid medication for pain compared to the Other Race group comprised of Asian, Native-Hawaiian/Pacific-Islanders (NHPI), and American-Indian/Alaska-Natives (AIAN) populations. Although these underrepresented subgroups are combined as a single group in NAMCS data due to limited NHPI and AIAN group sizes, census data indicates a likely composition of around 80% Asian, 17% AIAN, and 3% NHPI.23 No differences were found between White and Black patients, contrary to most studies of ED settings where White patients receive more opioid prescriptions.3,24,25 Although the reasons for this apparent discrepancy across ED and primary care settings are unclear, differences in time pressures, pain severity, chronicity, and consultation time13 are likely to be influential.13
To our best knowledge, this is the first investigation of pain medication prescribed in primary care that compares the more underrepresented racial groups with White and Black patient populations in a broad representative sample, and corroborates recent findings examining older Medicare patients seeking treatment for new low back pain.9 The lack of previous research is likely to be attributable to the difficulty of achieving sufficiently large samples, but is nevertheless surprising given that the Institute of Medicine report noted a particular need for further research on Asian, NHPI, and AIAN populations.1 Although visits to office-based physicians for pain by these patients collectively represent only 5% of all pain-related visits, this still constitutes around 7 million visits annually (Table 1). Furthermore, census projections indicate Hispanic and Asian populations to be the fastest growing subgroups in the US with population estimates for Asian Americans alone projected to almost triple to 62 million by 2065.26 Therefore, working to eliminate disparities in these groups is fundamental to future efforts for improving the nation’s health.
It is important to note that the choice of the “best” medication is dependent upon a considered clinical judgement of what is most appropriate for the presenting condition, and disparities in opioid prescribing do not automatically equate to inferior pain treatment. Nevertheless, the existence of substantive racial and ethnic disparities, especially after controlling for major potential confounds, does not seem to be easily explainable by differences in clinical presentation. Although the current data present robust evidence of the continued existence of disparities in pain care, they do not allow the determination of underlying mechanisms. Several explanations can nevertheless be considered. One, a significant proportion of the US Hispanic and Asian population report speaking English less than “very well” impairing their ability to communicate their health symptoms.1,12 Combined with time pressures, this can lead to diagnostic uncertainty and a reluctance to prescribe potentially inappropriate opioid medication. Two, physicians’ unconscious biases, including beliefs that minority groups are more easily addicted25 or have lower pain sensitivity27 despite evidence to the contrary12,28 may affect prescribing. Notably, however, unconscious biases have typically been previously investigated for Black and White patients, and we found no differences in prescribing between these two groups. Three, Asians and AIANs may be less likely to express pain due to embedded cultural values of stoicism or unwillingness to ask for help12 and Hispanic patients may reject opioids due to fears over addiction and side effects.29 Four, patients from specific underrepresented populations may exhibit greater reluctance to accept physician treatment recommendations based on a legacy of mistrust of the medical community and thus may be more likely to reject opioid treatment.1
The lack of narrowing of ethnic and racial disparities across 1999–2019 suggests legal, regulatory, and policy efforts30,31,32 to eliminate healthcare disparities have been unsuccessful with regard to pain treatment. Key recommendations of the Institute of Medicine report1 commissioned by Congress in 1999 included improving access to healthcare for underserved groups, better cross-cultural education during medical training to correct unconscious biases, and improving provider-patient communication by greater recruitment of underrepresented workers into healthcare. While legislation such as the Affordable Care Act has undoubtedly improved access to care for underserved groups,33 a failure to sufficiently implement the latter objectives may underlie the apparent continued existence of disparities in actual treatment.
Several limitations should be noted. To minimize administrative burden, NAMCS records minimal patient-provider encounter details and so offers limited insight into why disparities occur. In addition, unmeasured potential confounds such as reduced opioid availability in poorer, predominantly Black neighborhoods25,34 that might influence prescribing would not be adequately captured by the census region variable. We were, nevertheless, able to adjust for several important variables, and findings would be unlikely to be reversed with additional covariates. It is important to note that factors such as insurance status could plausibly occupy mediating, explanatory roles by, for example, acting as a class signaller which could affect providers’ empathic reactions and consequently their prescribing behavior. If this is the case, treating such variables as confounds by controlling for them could potentially result in an underestimation of RRs, and future studies should employ causal analysis models to help examine alternative model specifications.
A further limitation is the high proportion of imputed race and ethnicity data; although the general pattern of disparities observed is consistent with other studies6,7,8,10 and threshold analysis suggested that disparities would disappear only under relatively implausible conditions. NAMCS also does not assess pain severity; although previous evidence has typically found underrepresented groups to report greater, not less, pain12,35 compared to non-Hispanic or White patients. Medication and diagnostic information are also provider-reported so may not be optimally reliable, although verification checks have generally been favorable.15 Finally, while the aggregation of Asian, NHPI, and AIAN patients into a single group due to small samples is useful in broadly indicating the primary care experiences of the most underrepresented populations, it is impossible to determine whether this masks differential care experiences amongst these subgroups.
In summary, an analysis of 94,422 patient records observed no differences between Black and White patients in medication prescribed for pain but found that other underrepresented races and Hispanic/Latino patients were markedly less likely to receive prescriptions for opioid medication. There was little evidence for change in these prescribing disparities across a 21-year period from 1999 to 2019. Overall, these findings suggest that despite political and regulatory efforts, additional intervention strategies or better implementation of existing strategies are needed to eliminate disparities and achieve the goal of equitable healthcare.
Data Availability
This study uses publicly available data which can be downloaded from the CDC website (https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm).
References
Institute Of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. https://doi.org/10.17226/12875.
The White House. FACT SHEET: Biden-Harris Administration Releases Agency Equity Action Plans to Advance Equity and Racial Justice Across the Federal Government. Published 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/04/14/fact-sheet-biden-harris-administration-releases-agency-equity-action-plans-to-advance-equity-and-racial-justice-across-the-federal-government/. Accessed 23 June 2023.
Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299:70-78. https://doi.org/10.1001/jama.2007.64.
Parast L, Mathews M, Martino S, Lehrman WG, Stark D, Elliott MN. Racial/ethnic differences in emergency department utilization and experience. J Gen Intern Med. 2022;37:49-56. https://doi.org/10.1007/s11606-021-06738-0.
National Center For Health Statistics. National Ambulatory Medical Care Survey: 2018 National Summary Tables. Published 2018. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2018-namcs-web-tables-508.pdf. Accessed 5 June 2023.
Rasu RS, Knell ME. Determinants of opioid prescribing for nonmalignant chronic pain in US outpatient settings. Pain Med. 2018;19:524-532. https://doi.org/10.1093/pm/pnx025.
Ly DP. Racial and Ethnic disparities in the evaluation and management of pain in the outpatient setting, 2006-2015. Pain Med. 2019;20:223-232. https://doi.org/10.1093/pm/pny074.
Lin HC, Wang Z, Boyd C, Simoni-Wastila L, Buu A. Associations between statewide prescription drug monitoring program (PDMP) requirement and physician patterns of prescribing opioid analgesics for patients with non-cancer chronic pain. Addict Behav. 2018;76:348-354. https://doi.org/10.1016/j.addbeh.2017.08.032.
Ly DP. Association of patient race and ethnicity with differences in opioid prescribing by primary care physicians for older adults with new low back pain. JAMA Health Forum. 2021;2:e212333. https://doi.org/10.1001/jamahealthforum.2021.2333.
Olsen Y, Daumit GL, Ford DE. Opioid prescriptions by U.S. primary care physicians from 1992 to 2001. J Pain. 2006;7:225-235. https://doi.org/10.1016/j.jpain.2005.11.006.
Bauer, SR, Hitchner, L, Harrison H, Gerstenberger J, Steiger S. Predictors of higher-risk chronic opioid prescriptions in an academic primary care setting. Subst Abus. 2016;37:110-117.
Institute of Medicine. Relieving pain in America: A blueprint for transforming prevention, care, education, and research. 2011. https://doi.org/10.17226/13172.
Heron SL, Stettner E, Haley LL. Racial and ethnic disparities in the emergency department: a public health perspective. Emerg Med Clin North Am. 2006;24:905-923. https://doi.org/10.1016/j.emc.2006.06.009.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315:1624-1645. https://doi.org/10.1001/jama.2016.1464.
National Center For Health Statistics. Datasets and documentation. Centers for Disease Control and Prevention. Published 2023. https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm. Accessed 5 May 2023.
Centers For Disease Control And Prevention. The Ambulatory Care Drug Database System. Published 2023. https://www2.cdc.gov/drugs/applicationnav1.asp. Accessed 5 May 2023.
Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13:150-174. https://doi.org/10.1111/j.1526-4637.2011.01310.x
Dahlhamer J, Connor E, Jonaki Bose BS, Lucas JW, Zelaya C. Prescription opioid use among adults with chronic pain: United States, 2019. National Health Statistics Reports. 2021;162:1-9.
Cohen J, Cohen P, West S, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ US: Lawrence Erlbaum Associates Publishers; 2003.
Hastie TJ. Generalized additive models (Chapter 7). In: Chambers JM, Hastie TJ, eds. Statistical Models. Wadsworth & Brooks/Cole; 1992.
Lumley T. survey: analysis of complex survey samples. R package version 4.2. 2023.
Thompson T, Dias S, Poulter D et al. Efficacy and acceptability of pharmacological and non-pharmacological interventions for non-specific chronic low back pain: a protocol for a systematic review and network meta-analysis. Syst Rev. 2020;9. https://doi.org/10.1186/s13643-020-01398-3.
United States Census Bureau. Census data. Published 2023. https://www.census.gov/data.html. Accessed 23 June 2023.
Thompson T, Stathi S, Buckley F, Shin JI, Liang CS. Trends in racial inequalities in the administration of opioid and non-opioid pain medication in US Emergency Departments across 1999-2020. J Gen Intern Med. 2023. https://doi.org/10.1007/s11606-023-08401-2.
Morden NE, Chyn D, Wood A, Meara E. Racial inequality in prescription opioid receipt - role of individual health systems. N Engl J Med. 2021;385:342-351. https://doi.org/10.1056/NEJMsa2034159.
Koh H, Park J. Health Equity Matters for Asian Americans, Native Hawaiians, and Pacific Islanders. Published 2023. https://jamanetwork.com/channels/health-forum/fullarticle/2760153. Accessed 23 Aug 2023.
Santoro TN, Santoro JD. Racial bias in the US opioid epidemic: A Review of the history of systemic bias and implications for care. Cureus. 2018;10:e3733. https://doi.org/10.7759/cureus.3733.
Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314:1468-1478. https://doi.org/10.1001/jama.2015.11859.
Meints SM, Cortes A, Morais CA, Edwards RR. Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Manag. 2019;9:317-334. https://doi.org/10.2217/pmt-2018-0030.
Centers For Medicare & Medicaid Services. CMS Framework for Health Equity 2022–20322. Published 2023. https://www.cms.gov/files/document/cms-framework-health-equity-2022.pdf. Accessed 23 June 2023.
Public Law 111 - 148 - Patient Protection and Affordable Care Act. Published 2010. https://www.govinfo.gov/app/details/PLAW-111publ148. Accessed 5 May 2023.
Meghani SH, Polomano RC, Tait RC, Vallerand AH, Anderson KO, Gallagher RM. Advancing a national agenda to eliminate disparities in pain care: directions for health policy, education, practice, and research. Pain Med. 2012;13:5-28. https://doi.org/10.1111/j.1526-4637.2011.01289.x.
Buchmueller TC, Levy HG. The ACA’s impact on racial and ethnic disparities in health insurance coverage and access to care. Health Aff (Millwood). 2020;39:395-402. https://doi.org/10.1377/hlthaff.2019.01394.
Morales ME, Yong RJ. Racial and ethnic disparities in the treatment of chronic pain. Pain Med. 2021;22:75-90. https://doi.org/10.1093/pm/pnaa427.
Goya Arce AB, Richardson PA, Tran ST, Bhandari RP. Comparison of pain and psychosocial correlates among Hispanic and Non-Hispanic White youth with chronic pain. Pain Rep. 2022;7:e1020. https://doi.org/10.1097/PR9.0000000000001020.
Author information
Authors and Affiliations
Contributions
TT was responsible for the study conceptualisation, data analysis, and writing of the draft manuscript. CL directly accessed and verified the underlying data reported in the manuscript. All authors contributed to the interpretation of findings, revised the draft for important intellectual content, agreed to be accountable for all aspects of the work, and approved the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of Interest:
MS has received honoraria/has been a consultant for AbbVie, Angelini, Lundbeck, and Otsuka, all unrelated to this work. All authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thompson, T., Stathi, S., Shin, J.I. et al. Racial and Ethnic Disparities in the Prescribing of Pain Medication in US Primary Care Settings, 1999–2019: Where Are We Now?. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-024-08638-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-024-08638-5