Abstract
Background
The simplified HOSPITAL score is an easy-to-use prediction model to identify patients at high risk of 30-day readmission before hospital discharge. An earlier stratification of this risk would allow more preparation time for transitional care interventions.
Objective
To assess whether the simplified HOSPITAL score would perform similarly by using hemoglobin and sodium level at the time of admission instead of discharge.
Design
Prospective national multicentric cohort study.
Participants
In total, 934 consecutively discharged medical inpatients from internal general services.
Main Measures
We measured the composite of the first unplanned readmission or death within 30 days after discharge of index admission and compared the performance of the simplified score with lab at discharge (simplified HOSPITAL score) and lab at admission (early HOSPITAL score) according to their discriminatory power (Area Under the Receiver Operating characteristic Curve (AUROC)) and the Net Reclassification Improvement (NRI).
Key Results
During the study period, a total of 3239 patients were screened and 934 included. In total, 122 (13.2%) of them had a 30-day unplanned readmission or death. The simplified and the early versions of the HOSPITAL score both showed very good accuracy (Brier score 0.11, 95%CI 0.10–0.13). Their AUROC were 0.66 (95%CI 0.60–0.71), and 0.66 (95%CI 0.61–0.71), respectively, without a statistical difference (p value 0.79). Compared with the model at discharge, the model with lab at admission showed improvement in classification based on the continuous NRI (0.28; 95%CI 0.08 to 0.48; p value 0.004).
Conclusion
The early HOSPITAL score performs, at least similarly, in identifying patients at high risk for 30-day unplanned readmission and allows a readmission risk stratification early during the hospital stay. Therefore, this new version offers a timely preparation of transition care interventions to the patients who may benefit the most.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Hospital readmissions after an initial hospitalization are common and are associated with a significant burden for the patients, their families, and the healthcare system.1,2,3 The transition of care from hospital to ambulatory setting is a high-risk period, especially for patients with higher comorbidity which has been associated with a higher risk of readmission.4,5,6 Furthermore, each admission is associated with a risk of new complications7, 8 and it is estimated that 30% of the readmissions are preventable und thus avoidable.9
To identify the patients at higher risk for readmission is challenging, as providers are not able to accurately evaluate the risk10 and very few prediction model tools have been validated. The HOSPITAL score showed good performances in predicting 30-day readmission, and a very good generalizability. It has been now validated in four continents, six countries, more than 136,000 patients in both retrospective11, 12 and prospective cohorts,13 and therefore currently is the best validated prediction model when compared to other scores14 and has outperformed the LACE score in two recent studies.11, 13 The original version of the HOSPITAL score includes seven readily available variables, and the simplified version six variables (number of procedures being left out), and both showed similar performances.15
Since the HOSPITAL score or its simplified version is calculated shortly before discharge, it may limit the time available to prepare the discharge. This timely constraint is mainly due to use of the last measured hemoglobin and sodium level before discharge, leaving only the variable length of stay unknown at time of admission. Therefore, we aimed to assess in a prospective multicenter cohort whether the simplified HOSPITAL score would perform similarly by using hemoglobin and sodium level at time of admission instead of discharge.
METHODS
Study Design and Participants
We conducted a prospective multicenter cohort study, which included all consecutive patient discharges from July 2017 to March 2018 in the medical services of four mid-sized hospitals in Switzerland. The participating centers were (1) Centre Hospitalier de Bienne, (2) Fribourg Cantonal Hospital, (3) Cantonal Hospital Baselland, Liestal, and (4) Neuchâtel Hospital Network. All are 100–120-bed services in a community teaching hospital.
All consecutive adult patients planning to be discharged alive from the internal general medicine wards were screened for eligibility. We included patients who were discharged home or to a nursing home and who stayed for at least 24 h at the hospital. In Switzerland, nursing homes are convalescent long-term care. Therefore, patients transferred to another acute-care hospital or to rehabilitation facilities were not included. We excluded patients from whom we could not obtain an informed consent (unable, not willing, or not obtained before discharge), were not living in the country, could not speak one of the two main national languages (French or Swiss German), or did not have a phone number to be reached at. Written informed consent was obtained from all the participants prior to their enrollment. The trial protocol was approved by the institutional review board of each site. The study was entirely funded by the Swiss National Science Foundation (government funding).
Study Outcome
The primary outcome was the composite of the number of patients who had an unplanned readmission or who died within 30 days after hospital discharge. Unplanned readmission was defined as an urgent or emergent hospitalization (i.e., not scheduled more than 24 h in advance for investigation or treatment) to any division of any acute care hospital and that happened within 30 days after discharge from the index hospital discharge. Death was defined as all-cause mortality occurring within 30 days after discharge. As patients who died may have been readmitted if they had not died, we included both readmission and death as a composite outcome. The patients who were first readmitted and then died in the hospital counted as both readmissions and deaths.
A trained study nurse collected the outcomes at 30 days after hospital discharge by standardized phone interview. For patients who could not be reached after three attempts, information was collected through the patient relatives or the patients’ primary care physician. Finally, the electronic health system of the discharge hospital was screened for readmission or death. A lost to follow-up was defined as a patient with no information obtained from any of these four sources, or who withdrew consent during the study period.
Predictor Variables
We collected the variables of the HOSPITAL score based on the same definition of the original study. We collected the Hemoglobin and Sodium levels (letters “H” and “S”) both at admission (i.e., within the first 24 h of admission) and at discharge (i.e., last lab value available before discharge). Because not all of the hospitals had a specific oncology division, the variable “discharge from an Oncology service” (letter “O”) was replaced by “active Oncologic diagnosis on admission or during hospitalization,” i.e., in the past 5 years, including metastatic and non-metastatic solid tumors and hematologic malignancies.13, 15, 16 The following procedures (letter “P”) were taken into account in the original version for the HOSPITAL score: coronary angiography, angioplasty, thromboaspiration, stenting, pacemaker implantation, transesophageal echocardiography, esogastroduodenoscopy, endoscopic retrograde cholangio-pancreatography, coloscopy, bronchoscopy, biopsy, thoracocentesis, lumbal puncture, paracentesis, chemotherapy, radiotherapy, continuous pressure ventilation, intubation, transfusion (blood or platelets), graft, dialysis, operation, suture, electro-neuromyography, joint aspiration, cystoscopy, bone marrow aspiration/biopsy, magnetic resonance imaging, computer tomography, angiography, positron emission tomography, scintigraphy.1 We collected the variables “Index admission Type” (letter “I” and “T”) and “number of hospital Admission(s) during the previous year” (letter “A”) as in the original study. We adapted the cutoff for the length of stay (letter “L”) to the median length of stay in Switzerland (8 days instead of 5 days for the USA), as previously done.13, 16 The simplified version of the HOSPITAL score includes six variables with the number of procedures being left out (Table 1). The three versions of the HOSPITAL score were compared: the original HOSPITAL score, the simplified HOSPITAL score, and the early HOSPITAL score (simplified score with lab at admission).
Statistical Analysis
Baseline characteristics are presented using absolute and relative frequencies for categorical and median, lower quartile (lq), and upper quartile (uq) for continuous variables.
The area under the receiver operating characteristic (ROC) curve (AUROC) is presented with asymptotic normal 95% CI. The Brier score was calculated using internally predicted (estimated) probabilities and is presented with bias-corrected bootstrap 95% CI. Goodness of fit was assessed by comparing observed and predicted probabilities by deciles of the predicted probabilities. The three versions of the HOSPITAL score were categorized into two groups: unlikely and likely to be readmitted, according to the number of points. Optimal cut-points were 5 points for the HOSPITAL score, and 4 points for the simplified HOSPITAL score and the early HOSPITAL score (with lab values from admission). These were calculated according to the methods of Liu17 and Youden.18 At these cut-points, we calculated sensitivity (SE), specificity (SP), and predictive values (PV) with exact binomial 95%CI, likelihood ratios with the Katz 95%CI, and the diagnostic odds ratio with Cornfield 95%CI.
The original and simplified HOSPITAL scores were compared using the AUC (based on a non-parametric procedure suggested by DeLong et al.),19 and the category-free (or continuous) version of the net reclassification improvement or index (NRI)20, 21 with 95% bias-corrected bootstrap CI.
Readmission rates are presented with Wilson score 95% confidence intervals (CI). The composites of unplanned readmission and death were analyzed using the Kaplan–Meier estimator with 95%CI based on pointwise Greenwood standard errors. The competing risks for readmission and death (without readmission) were analyzed using the cumulative incidence with 95%CI.22
RESULTS
During the study period, we screened a total of 3239 patients. Among them, 2305 (71.2%) were excluded: 653 (20.2%) because of not meeting inclusion criteria and 1652 (51%) because of the presence of exclusion criteria. We therefore enrolled 934 medical patients (Fig. S1). For five patients, the 30 days interview could not be done: four because of withdrawal of consent and one because of violation of inclusion criteria (not discharged home/nursing home). In total, 924 of the remaining 929 patients had the primary outcome available while five patients had missing data (one lost to follow-up, two withdrew consent, two incomplete data). The variables of the HOSPITAL scores and the baseline characteristics for participants with and without 30-day readmission or death are reported in Tables 2 and 3 (also Table S2). Among the included patients, 122 (13.2%) had a 30-day unplanned readmission or death. Of those, 111 (91%) were readmitted and 21 (17%) died. Of those readmitted, 10 were first readmitted and then died in the hospital. The median hemoglobin levels at admission and discharge were 13.2 and 12.4 g/dl, and the median sodium level was 137 and 139 mmol/l, respectively. The proportions of patients categorized as high risk were 28% for the original score and 34% for the two simplified score versions (258, 311, and 312 patients, respectively).
The discriminatory power of the three score versions was almost identical with an AUROC of 0.66 (95%CI 0.61–0.71) for the original and early HOSPITAL score, and 0.66 (95%CI 0.60–0.70) for the simplified version. The overall comparison between the different versions of the score was not statistically significant (p value 0.96).
The sensitivity of the HOSPITAL score was slightly lower in comparison to the simplified score and its early version using the lab at admission (50% vs 57% and 58% respectively), while its specificity was slightly higher compared to both simplified scores (75% vs 70% and 70% respectively). The global performance of each score was similar in terms of positive and negative predictive values, as well as for the positive likelihood ratio (LR). The negative LR was slightly worse in the HOSPITAL score compared to both the simplified score and its early version (0.66, 0.61, and 0.60 respectively).
The Brier score of 0.11 (95%CI 0.10 to 0.13) indicated a good overall performance of the original HOSPITAL score. Both the simplified version of the HOSPITAL score and the early HOSPITAL score had the same accurate performance with a Brier score of 0.11 (95%CI 0.10 to 0.13).
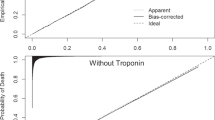
All three scores showed a reasonable goodness-of-fit with p values from the Hosmer–Lemeshow test of 0.35, 0.34, and 0.22 for the original, early, and simplified HOSPITAL scores respectively (Fig. 1).
Goodness-of-fit for the three versions of the HOSPITAL score. Observed probabilities of readmission or death with 95% confidence intervals per decile of the internally predicted probabilities. The distribution of patients with (red) and without (black) readmissions or deaths is shown in the gray area.
The net reclassification improvement (NRI) in the simplified compared to the original HOSPITAL score was as follows: − 0.15 (95%CI − 0.32 to 0.03) with a p value of 0.12. Compared with the model at discharge, the model with lab at admission (early version) showed improvement in classification based on the continuous NRI 0.28 (95%CI 0.08 to 0.48) with a significative p value of 0.004 mainly driven by an improvement in prediction of non-cases that compensated the worse prediction for cases: 75% (599/802) non-cases had a lower risk if lab at admission was used, while 39% (48/122) cases had a higher risk if lab at admission was used.
DISCUSSION
This study validates the use of the HOSPITAL score using lab at admission instead of discharge, which allows a more timely decision-making. Not only the performance was identical with a C-statistic of 0.66, but we found an even better prediction of non-cases. Therefore, the early HOSPITAL score offers an interesting alternative to identify the risk of readmission earlier during the hospital stay. To our knowledge, the early HOSPITAL score is the only validated score that can be used early after admission to assess the risk of 30-day readmission and death.
Among the six variables included in the early HOSPITAL score, five are known at admission, and only the length of stay (LOS) above the median (≥ 8 days) would remain unknown until the threshold is reached. We showed in this study that only 15% of the patients would be reclassified from low risk to high risk once the length of stay exceeds the cut-off. Therefore, 85% of the patients may have their prediction calculated already at time of hospital admission. Other known readmission prediction models include variables that are available only at discharge or after discharge.
We can hypothesize that the similar performance using lab values at admission may be explained by quite similar values of hemoglobin and sodium between admission and discharge, which does not affect the score. These lab values probably reflect more the severity of the patient’s comorbidities than the state of health at a specific time (admission vs discharge). For example, it is expected that a patient with a hemoglobin level at admission lower than 12 g/dl will still leave the hospital with a hemoglobin below 12 g/dl, since the transfusion threshold is much lower. Regarding the low level of sodium, we identified more patients with hyponatremia at admission than at discharge. This was to be expected, but the purpose of the study was to show that by using the admission values, the score is still able to identify patients at high risk of admission. And indeed, the results showed that this is the case.
An early identification of high-risk patients may be indeed valuable. In a recent meta-analysis of 47 randomized controlled trials, it was shown in the subgroup analysis that interventions starting already during hospital stay and continuing after discharge were more effective in reducing readmissions compared to interventions starting after discharge.23 The study emphasizes that interventions enhancing patient empowerment were the most effective, and thus highlights the importance of patient’s education in reducing hospital readmissions. Therefore, the use of the early HOSPITAL score may offer to target patients at high risk of readmission earlier during the admission in order to anticipate the discharge and simplify the preparation, the organization of an intervention, and patient’s empowerment.
The study has to be interpreted considering some limitations. First, the findings might not apply to other patient populations, as any validation study. However, our study included patients discharged from the general internal medicine ward from different teaching hospital sizes, which included medical patients with multiple chronic conditions. Second, the only remaining variable not available at admission is the LOS. However, as mentioned above, only 15% of high-risk patients would have their risk classification changing due to the LOS, and most of these patients may have a predictable short versus long LOS at admission. Therefore, a patient who is high risk based on admission variables will remain at high risk regardless of length of stay, and may therefore be targeted for readmission reduction strategies early on. The strengths of this large study are the prospective and multicenter design, giving a high level of validation.
CONCLUSION
The early HOSPITAL score showed overall good and similar performance in identifying patients at high risk for 30-day unplanned readmission. Interestingly, the early version using most of the parameters available already at admission showed similar good performance and could be useful in identifying patients earlier before their hospital discharge. Therefore, this early HOSPITAL score version offers a readmission risk stratification early during the hospital stay, which allows a timely preparation of transition care interventions to the patients who may benefit the most. Using the early HOSPITAL score might allow to target high-risk patients, who will more benefit from an intervention and thus reduce readmission.
References
Donzé J, Aujesky D, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med. 2013;173:632–638.
Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428.
Zekry D, et al. Prospective comparison of 6 comorbidity indices as predictors of 1-year post-hospital discharge institutionalization, readmission, and mortality in elderly individuals. J Am Med Dir Assoc. 2012;13:272–278.
van Walraven C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557.
Librero J, Peiró S, Ordiñana R. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52:171–179.
Forster AJ et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170:345–349.
Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167.
van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391-402.
Allaudeen N, Schnipper JL, Orav EJ, Wachter RM, Vidyarthi AR. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26:771–776.
Cooksley T, et al. Readmissions of medical patients: an external validation of two existing prediction scores. QJM. 2016;109:245–248.
Donzé JD, et al. International Validity of the HOSPITAL Score to Predict 30-Day Potentially Avoidable Hospital Readmissions. JAMA Intern Med. 2016;176:496–502.
Aubert CE, Folly A, Mancinetti M, Hayoz D, Donzé J. Prospective validation and adaptation of the HOSPITAL score to predict high risk of unplanned readmission of medical patients. Swiss Med Wkly. 2016;146:w14335.
Kansagara D, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698.
Aubert CE, et al. Simplification of the HOSPITAL score for predicting 30-day readmissions. BMJ Qual Saf. 2017;26:799–805.
Aubert CE, et al. HOSPITAL Score and LACE Index to Predict Mortality in Multimorbid Older Patients. Drugs Aging. 2022;39:223–234.
Liu X. Classification accuracy and cut point selection. Stat Med. 2012;31(23):2676–86.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845.
Pencina MJ, D’Agostino RB, D’Agostino RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172; discussion 207-212.
Pencina MJ, D’Agostino RB, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30:11–21.
Choudhury JB. Non-parametric confidence interval estimation for competing risks analysis: application to contraceptive data. Stat Med. 2002;21:1129–1144.
Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14:106–173.
Funding
Open access funding provided by University of Bern. The study was funded by the Swiss National Science Foundation (PP00P3-17066), which had no role in the study design, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All the authors had full access to all of the data in the study, take responsibility for the integrity of the data and the accuracy of the data analysis, and are the guarantor. Study concept and design: Donzé. Acquisition of data: Donzé, Mathys, Genné, Leuppi, Mancinetti. Aujesky. Analysis and interpretation of data: Mathys, Donzé, Bütikofer. Drafting of the manuscript: Mathys, Donzé, Bütikofer. Critical revision of the manuscript for important intellectual content: Bütikofer, Genné, Leuppi, Mancinetti, Aujesky. Statistical analysis: Bütikofer.
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mathys, P., Bütikofer, L., Genné, D. et al. The Early HOSPITAL Score to Predict 30-Day Readmission Soon After Hospitalization: a Prospective Multicenter Study. J GEN INTERN MED 39, 756–761 (2024). https://doi.org/10.1007/s11606-023-08538-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08538-0