Abstract
Background
Digital health devices (DHDs), technologies designed to gather, monitor, and sometimes share data about health-related behaviors or symptoms, can support the prevention or management of chronic conditions. DHDs range in complexity and utility, from tracking lifestyle behaviors (e.g., pedometer) to more sophisticated biometric data collection for disease self-management (e.g., glucometers). Despite these positive health benefits, supporting adoption and sustained use of DHDs remains a challenge.
Objective
This analysis examined the prevalence of, and factors associated with, DHD use within the Veterans Health Administration (VHA).
Design
National survey.
Participants
Veterans who receive VHA care and are active secure messaging users.
Main Measures
Demographics, access to technology, perceptions of using health technologies, and use of lifestyle monitoring and self-management DHDs.
Results
Among respondents, 87% were current or past users of at least one DHD, and 58% were provided a DHD by VHA. Respondents 65 + years were less likely to use a lifestyle monitoring device (AOR 0.57, 95% CI [0.39, 0.81], P = .002), but more likely to use a self-management device (AOR 1.69, 95% [1.10, 2.59], P = .016). Smartphone owners were more likely to use a lifestyle monitoring device (AOR 2.60, 95% CI [1.42, 4.75], P = .002) and a self-management device (AOR 1.83, 95% CI [1.04, 3.23], P = .037).
Conclusions
The current analysis describes the types of DHDs that are being adopted by Veterans and factors associated with their adoption. Results suggest that various factors influence adoption, including age, access to technology, and health status, and that these relationships may differ based on the functionalities of the device. VHA provision of devices was frequent among device users. Providing Veterans with DHDs and the training needed to use them may be important factors in facilitating device adoption. Taken together, this knowledge can inform future implementation efforts, and next steps to support patient-team decision making about DHD use.
Similar content being viewed by others
INTRODUCTION
Digital health devices (DHDs) are designed to gather, track, monitor, and sometimes share data about health-related behaviors or symptoms. The growing development and use of DHDs represents a technological revolution in healthcare, allowing patients and their care teams to continuously monitor health behaviors and outcomes outside of the clinical visit.1, 2 The aging US population and increased prevalence of patients living with multiple chronic conditions3 underscores the need to better engage patients in their own health in an effort to ameliorate health care resource burden.4 The Veterans Health Administration (VHA) Office of Connected Care is committed to improving health care through technology by engaging Veterans and their clinical teams outside of episodic health care visits, which can in part be supported by patient use of DHDs.5
DHDs and their associated data range in functions, from providing feedback to users to help them understand their health (i.e., lifestyle monitoring devices) to supporting preventative and self-management behaviors (i.e., self-management devices), thereby improving how patients and their clinical teams prevent and/or manage chronic conditions.6, 7 This functionality is especially relevant for Veterans, who face disproportionate rates of chronic disease compared to the general US adult population.8
Despite the potential benefits of DHDs, supporting their adoption remains a challenge. Most literature describes consumer intention to adopt DHDs,9, 10 rather than actual adoption. The objective of the current analysis was to examine use and perceptions of different types of DHDs among Veterans who receive healthcare within the VHA, and to identify factors associated with use of DHDs.
METHODS
Design
The Veterans Engagement with Technology Collaborative (VET-C) cohort was initiated in 2017 to help inform quality improvement and implementation efforts focused on virtual care technology implementation and use in VHA. 11 It includes longitudinal survey data collected at three time-points from a nationwide sample of Veterans who are known technology users, coupled with demographic and health information from VHA administrative data. Surveys collected data on Veteran perceptions of VHA healthcare, technology ownership and use, and preferences for using technology to support their health. VET-C was supported by VHA’s Quality Enhancement Research Initiative (QUERI) Program and the VHA Office of Connected Care. The Office of Connected Care’s mission is to deliver high-quality, Veteran-centered care, optimize individual and population health, advance health care that is personalized and proactive, and enhance the health care experience through virtual modalities of care.12 This work was designated as a program evaluation for quality improvement purposes by the affiliated institutional review boards (VHA Handbook 1058.05).
Sample
The VET-C cohort was sampled from 15 geographically dispersed facilities (see Appendix).11 Veterans who were active users of health-related technologies were purposefully sampled as they were thought to be most willing to make a long-term commitment to providing feedback on VHA virtual care technologies, including DHDs and mobile health applications. Therefore, mobile phone ownership and secure messaging use (i.e., having sent ≥ five messages in the year prior to cohort recruitment) were sampling inclusion criteria. Approximately 52% of national VHA users have access to use secure messaging through the patient portal, and 27% of national VHA users are active users of secure messaging.13 Secure messaging use was used as a proxy for Veteran openness to using new technologies, as well as their use of other VHA patient-facing technologies more broadly.
Data Collection Procedures
Survey data were collected from the VET-C cohort at three time points: 2017–2018, 2019–2020, and 2021. Procedures for these first two rounds of data collection are described in previous publications.11, 14, 15 Veterans who responded to the first two rounds were invited to complete a third survey between May and December 2021. Veterans were mailed a hard copy of this survey; non-responders were mailed an additional copy four weeks later. A total of 1,373 Veterans were invited to participate in this third survey round; the denominator was adjusted to 1,358 to reflect five Veterans who were deceased and 10 surveys which were returned as undeliverable. We received responses from 858 Veterans (858/1,358, 63.2% response rate). Data presented in the current analysis was largely collected in the third round of VET-C survey administration, although some demographic data (i.e., age, race, ethnicity, gender, educational attainment) was gathered in the first round of survey administration (detailed below). In addition, survey data were supplemented with electronic health record data from the VHA Corporate Data Warehouse, as appropriate.
Measures
Digital Health Device Use
Surveys asked Veterans to report their use of nine DHDs, which were then categorized based on The National Institute for Health and Care Excellence16 classification of health technologies across three evidence-based tiers. The current analysis focuses on the second and third tiers, which describe DHDs that help users to (1) understand healthy living and illnesses through informing and simple monitoring (i.e., lifestyle monitoring devices) and (2) prevent and manage diseases (i.e., self-management devices).16 The team reached consensus on the appropriate classification for each device based on this previously published criteria.16 Among the nine DHDs represented on the VET-C survey, three were categorized as lifestyle monitoring DHDs: Fitbit, smartwatch, and digital pedometer. As these three devices typically offer similar functionality, we collapsed them into one category. The remaining six DHDs were categorized as self-management DHDs: blood pressure monitor, electrocardiogram (EKG/ECG) monitor, glucometer, asthma inhaler, pulse oximeter, and spirometer. Participants were asked to indicate if they: currently use the device, used the device in the past but no longer use it, or if they have never used it. Participants also indicated if VHA provided them with any of the above devices.
Covariates
Data collected from the VHA Corporate Data Warehouse included rurality of residence and Hierarchical Condition Category (HCC)17 scores. HCC – a measure of comorbidity – accounts for age, gender, medical diagnoses using ICD-10 codes, and eligibility for Medicare and Medicaid services.17 Normalized to 1.0, HCC scores < 1.0 are considered scores of relatively healthy individuals.18
Respondents reported factors associated with their physical health, health care use, (i.e., whether they usually receive care within or outside of VHA), marital status, and socioeconomic status (SES; difficulty paying for basics like food or heating/cooling). Veterans were also asked about their access to technology (i.e., “Do you own or have easy access to a: computer, tablet, smartphone?”).
Analyses
We classified participants into DHD “users” and “non-users.” Users indicated current or past use of a DHD; non-users indicated no current or previous use of a DHD. Some respondents skipped all questions related to DHDs; thus, we could not determine whether these respondents were device users. In addition, respondents were not included if they skipped questions used as covariates in the multivariable models. The final analytic sample included 846 Veterans. Univariate analyses characterized the sample. We modeled three multiple logistic regressions to assess factors associated with three outcomes: 1) any DHD use, 2) lifestyle monitoring DHD use, and 3) self-management DHD use. Adjusted odds ratios (AORs) and 95% confidence intervals were calculated to measure the association between each factor and each outcome, after controlling for other variables in the model. AORs with 95% confidence intervals that did not include 1.00 were considered statistically significant.
RESULTS
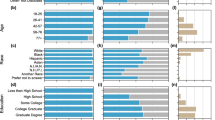
Table 1 presents demographic characteristics. Most were ≥ 65 years of age (71.7%, n = 607), male (87.5%, n = 740), white (88.9%, n = 752), non-Hispanic (96.8%, n = 819), married (68.3%, n = 578), and non-rural (85.1%, n = 720). Most reported that paying for basic necessities was “not very hard” (68.8%, n = 582) and education beyond high school (87%, n = 736), with a large portion having a master’s, professional, or doctoral degree (48.6%, n = 411). Most (86.6%, n = 733) indicated either current or previous DHD use (i.e., DHD users). More than half (57.8%, n = 489) reported that VHA provided them with at least one DHD. Among those who received a DHD from VHA, only 3.5% (n = 17) did not report any DHD use. Lifestyle monitoring DHD use was reported by 40.8% (n = 345) and self-management DHD use was reported by 79.4% (n = 672). Among self-management DHD users (n = 672), digital blood pressure monitors were most frequently reported (91.4%, n = 614; Table 2).
Factors associated with Digital Health Device Use
Results from the three multiple logistic regressions examining: (1) any DHD use, (2) lifestyle monitoring DHD use, and (3) self-management DHD use are in Table 3. When we examined any DHD use, Hispanic respondents had lower odds of being a DHD user compared to non-Hispanic respondents (AOR 0.22, 95% CI [0.06, 0.76], P = 0.017). Veterans with a master’s, professional, or doctoral degree had higher odds of being a device user compared to those with a high school education or less (AOR 2.07, 95% CI [1.06, 4.03], P = 0.033. Compared to those who reported receiving most of their care at VHA, those who reported receiving about half of their care outside VHA had greater odds of being a DHD user (AOR 1.88, 95% CI [1.03, 3.448], P = 0.040). Those who self-reported fair/poor physical health (compared to excellent/very good health) had higher odds of being a DHD user (AOR 2.58, 95% CI [1.33, 5.00], P = 0.005). Similarly, a higher HCC score (i.e., worse health) was associated with greater odds of being a DHD user (AOR 1.42, 95% CI [1.11, 1.82], P = 0.005). Further, respondents had higher odds of being a DHD user if they reported ownership or easy access to a tablet (AOR 1.81, 95% CI [1.16, 2.84], P = 0.009), or smartphone (AOR 2.13, 95% CI [1.17, 3.89], P = 0.014) compared to those who did not. Age, gender, race, marital status, rurality, SES, and computer access were not significantly associated with overall DHD use.
Regarding lifestyle monitoring DHD use, respondents who were ≥ 65 years (AOR 0.57, 95% CI [0.39, 0.81], P = 0.002) had lower odds of lifestyle monitoring DHD use compared those who were below 65 years of age. Veterans with a master’s, professional, or doctoral degree had higher odds of using a lifestyle monitoring DHD compared to those with a high school education or less (AOR 1.76, 95% CI [1.06, 2.94], P = 0.030. Those who reported ownership or easy access to a tablet (AOR 2.34, 95% CI [1.72, 3.19], P < 0.001), or smartphone (AOR 2.60, 95% CI [1.42, 4.75], P = 0.002) had higher odds of lifestyle monitoring DHD use compared to those who did not report ownership or easy access. Gender, race, ethnicity, marital status, rurality, SES, location of care, self-reported physical health, ownership or easy access to a computer, and HCC score were not significantly associated with lifestyle monitoring DHD use.
When we examined self-management DHD use, respondents who were ≥ 65 years (AOR 1.69, 95% CI [1.10, 2.59], P = 0.016), or male (AOR 2.50, 95% CI [1.49, 4.19], P = 0.001) had higher odds of use. Compared to respondents who self-reported excellent/very good health, those with good health (AOR 1.76, 95% CI [1.15, 2.68], P = 0.009) or fair/poor health (AOR 2.06, 95% CI [1.21, 3.52], P = 0.008) had higher odds of using a self-management DHD, as did those who had higher HCC scores (AOR 1.67, 95% CI [1.33, 2.10], P < 0.001). Respondents who owned or had easy access to a smartphone (AOR 1.83, 95% CI [1.04, 3.23], P = 0.037) also had higher odds of using a self-management DHD. Race, ethnicity, marital status, rurality, SES, education, location of care, and computer or tablet ownership/access were not significantly associated with self-management DHD use.
Table 4 displays frequencies and comparisons of DHD use by the most prevalent chronic conditions in the sample. There was a significantly smaller proportion of lifestyle monitoring DHD users (n = 87, 25.3%) compared to non-users (n = 165, 33.1%) among respondents with ischemic heart disease; P = 0.017. There were no other significant differences in lifestyle monitoring DHD use across the examined chronic conditions. Significantly greater proportions of self-management DHD users compared to non-users had atrial fibrillation, diabetes, chronic kidney disease, ischemic heart disease, and hypertension (Ps < 0.001). There were no significant differences in self-management DHD use among respondents with asthma or COPD.
DISCUSSION
Age, ethnicity, education, access to technology, and health were associated with DHD use in this cohort of US Veterans. Some associations differed by DHD functionality, extending existing knowledge on DHD use which has mostly focused on general DHD adoption. Notably, recent work found younger age was associated with a greater likelihood of general DHD use.19 The current evaluation found that this direction varied by device functionality; older adults were less likely to use a lifestyle monitoring DHD, but more likely to use a self-management DHD. Older adults are more likely to have a chronic disease20 and therefore may be more likely to be recommended a self-management DHD by their clinical team. However, the association between age and self-management DHD use was still significant after adjusting for comorbidities using HCC scores. Older adults’ lower likelihood to adopt a lifestyle monitoring DHD may also be attributed to them feeling less familiar with lifestyle monitoring DHDs or the benefits they could provide. Lifestyle monitoring is associated with enhanced disease management, and a reduced risk for chronic diseases and mortality.21,22,23 Despite the benefit lifestyle monitoring DHDs could have on clinical outcomes related to many chronic diseases, respondents with specific chronic conditions were not more likely to use a lifestyle monitoring DHD. It is important to raise clinical team members’ awareness of how lifestyle monitoring DHDs can yield data to support clinical or self-management of chronic conditions. As digital literacy remains a significant barrier to device adoption,24 investing in education and training for patients who are more hesitant to adopt DHDs will also be needed.
Significantly more survey respondents with diabetes, chronic kidney disease, ischemic heart disease, hypertension, or atrial fibrillation were users of a self-management DHD. Chronic respiratory diseases (asthma and COPD) were not associated with self-management DHD use. It may be that certain self-management DHDs (e.g., blood pressure cuffs, glucometers) have historically been more available compared to more recent commercialization of DHDs for chronic respiratory diseases. Given the high prevalence and burden of chronic respiratory disease, particularly in Veterans,25 future initiatives may look to targeting adoption efforts for devices specific to respiratory monitoring (e.g., digital pulse oximeters, digital asthma inhalers).26 This could include engaging healthcare systems to purchase DHDs for respiratory monitoring. One of the most prominent barriers to adoption of DHDs is their cost.27 In this sample, most device users reported being provided a device by VHA. VHA policy allows many different DHDs to be covered; however, access requires care teams and Veterans to be effectively informed of their availability.28 As provision of devices may reduce barriers to their use, it is important that VHA care team members and Veterans are educated about their availability as part of VHA benefits.
We did not find significant differences in DHD use by race, rurality, or SES. Hispanic respondents were less likely to be DHD users, but the sample of Hispanic Veterans within our analytic cohort was too small to find significant differences when examining lifestyle monitoring DHD use and self-management DHD use separately. Previous literature has documented disparities in health-related technology use based on SES (i.e., “the digital divide”). It is therefore noteworthy that our analysis did not identify such disparities among this sample. One possible explanation is that our sample was highly educated, particularly in comparison to the overall population of Veterans29 and VHA users.30, 31 Differences in education and current health status may partially mediate the racial and ethnic disparities commonly seen in technology use.32
Smartphone owners were more likely to use both lifestyle monitoring DHDs and self-management DHDs. This is a promising indicator for the trajectory of DHD adoption, as smartphone ownership is increasing annually.33 As of 2021, 85% of Americans reported owning a smartphone,33 a number similar in magnitude to our sample (90%) and to other broader Veteran populations (81.5%).34 Programs that support technology access may also support DHD adoption. For example, VHA’s Offices of Connected Care and Rural Health successfully supported tablet use by distributing tablets to Veterans experiencing barriers to in-person access, with the intention of supporting clinical video visits.35 In the current analysis, tablet ownership was associated with lifestyle monitoring DHD use, but not self-management DHD use, and was nearly 40% lower than that of smartphones. This number is comparable to that seen in larger, nationally representative studies.33 It is possible that those who own such technologies feel more comfortable with technology and are more likely to use a device. As use of one technology often generates use of others,36 any initiatives to support technology ownership will likely further support DHD adoption.
Limitations and Future Directions
The current analysis describes what types of devices are being adopted among Veterans. While DHDs can enhance health outcomes, not all are necessary for all patients. Additional work is needed to understand optimal applications of DHDs and corresponding dose/response relationships. The current work can inform future implementation efforts and evaluations of the effectiveness of DHD adoption. Additionally, this analysis is limited to patient characteristics. Future work would benefit from integrating healthcare system and healthcare team perspectives to more fully account for the range of possible barriers and facilitators to DHD adoption. Future work would also benefit from better understanding the directionality of these associations. This analysis focused on DHD use but did not capture DHD ownership or other barriers to use. Future work should also explore device ownership, as patients who own but do not use a DHD likely face unique barriers to adoption. Additionally, self-reported DHD use may not accurately reflect actual DHD use. We are also unable to distill respondents’ use of multifunctional devices, or how, if at all, patient-generated data is being communicated back to the care team.
This sample was purposefully recruited to assist quality improvement and implementation efforts focused on virtual care technologies, and as such, was comprised of active users of VHA’s patient portal. Users of VHA’s patient portal are often more educated, younger, and have higher income than the general Veteran population.37, 38 In addition, as is typical with the overall Veteran population, our sample was mostly male, and therefore may not be representative of non-Veterans within the general US population. Finally, we are unable to assess the temporal impact of surveying Veterans among this cohort during the COVID-19 pandemic.
Conclusion
DHDs have the potential to support health promotion and disease management and it is important to identify factors that are associated with device use to support future engagement efforts. Older age was associated with greater odds of self-management DHD adoption, but lower odds of lifestyle monitoring DHD adoption. Additionally, provision of DHDs and access to technology were associated with device adoption. Individuals living with a chronic disease were more likely to adopt a device for self-management, though there remain opportunities to support respiratory disease management and adoption for lifestyle monitoring.
References
Vogels E. About one-in-five Americans use a smart watch or fitness tracker. 2020. https://www.pewresearch.org/fact-tank/2020/01/09/about-one-in-five-americans-use-a-smart-watch-or-fitness-tracker/. Accessed 23 Oct 2023.
Wearable Medical Devices Market Size, Share and Industry Analysis by Product (Diagnostic & Patient Monitoring, Therapeutics), by Application (Remote Patient Monitoring and Home Healthcare, Sports and Fitness), by Distribution Channel (Retail Pharmacies, Online Pharmacies, Hypermarkets) and Regional Forecast 2019–2026. 2019. https://www.fortunebusinessinsights.com/industry-reports/wearable-medical-devices-market-101070. Accessed 23 Oct 2023.
James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392(10159):1789-1858.
Mitchell M, Kan L. Digital technology and the future of health systems. Health Systems & Reform. 2019;5(2):113-120.
Loncar-Turukalo T, Zdravevski E, Machado Da Silva J, Chouvarda I, Trajkovik V. Literature on Wearable Technology for Connected Health: Scoping Review of Research Trends, Advances, and Barriers. Journal of Medical Internet Research. 2019;21(9):e14017. doi:https://doi.org/10.2196/14017
Lu L, Zhang J, Xie Y, et al. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR mHealth and uHealth. 2020;8(11):e18907. doi:https://doi.org/10.2196/18907
Lin B. Wearable smart devices for P4 medicine in heart disease: Ready for medical cyber-physical systems? Omics: a journal of integrative biology. 2019;23(5):291–292. doi:https://doi.org/10.1089/omi.2019.0059
Eibner C, Krull H, Brown KM, et al. Current and Projected Characteristics and Unique Health Care Needs of the Patient Population Served by the Department of Veterans Affairs. RAND Corporation; 2015.
Zhang M, Luo M, Nie R, Zhang Y. Technical attributes, health attribute, consumer attributes and their roles in adoption intention of healthcare wearable technology. International Journal of Medical Informatics. 2017/12/01/ 2017;108:97–109. doi:https://doi.org/10.1016/j.ijmedinf.2017.09.016
Park E. User acceptance of smart wearable devices: An expectation-confirmation model approach. Telematics and Informatics. 2020;47:101318.
Etingen B, Amante DJ, Martinez RN, et al. Supporting the Implementation of Connected Care Technologies in the Veterans Health Administration: Cross-Sectional Survey Findings from the Veterans Engagement with Technology Collaborative (VET-C) Cohort. J Participat Med. 2020/9/30 2020;12(3):e21214. doi:https://doi.org/10.2196/21214
VHA Connected Care Strategic Plan 2021–2025 (2021).
VHA Support Service Center Capital Assets (VSSC). U.S. Department of Veterans Affairs.
Martinez RN, Smith BM, Etingen B, et al. Health-Related Goal Setting and Achievement Among Veterans with High Technology Adoption. Journal of General Internal Medicine. 2021/11/01 2021;36(11):3337–3345. doi:https://doi.org/10.1007/s11606-021-06779-5
Hogan TP, Etingen B, Lipschitz JM, et al. Factors Associated With Self-reported Use of Web and Mobile Health Apps Among US Military Veterans: Cross-sectional Survey. JMIR Mhealth Uhealth. Dec 30 2022;10(12):e41767. doi:https://doi.org/10.2196/41767
National Institute for Health and Care Excellence. Evidence Standards Framework for Digital Health Technologies. 2019. Accessed July 14, 2022. https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf
Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health care financing review. 2004;25(4):119.
Hoffman AF, Reiter KL, Randolph RK. Average Beneficiary CMS Hierarchical Condition Category (HCC) Risk Scores for Rural and Urban Providers. Chapel Hill, NC: Sheps Center for Health Services Research. 2018;
Chandrasekaran R, Katthula V, Moustakas E. Patterns of Use and Key Predictors for the Use of Wearable Health Care Devices by US Adults: Insights from a National Survey. Journal of Medical Internet Research. 2020;22(10):e22443. doi:https://doi.org/10.2196/22443
Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell. 2014;159(4):709-713.
Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. The Lancet. 2017;390(10113):2643-2654.
Anderson E, Durstine JL. Physical activity, exercise, and chronic diseases: A brief review. Sports Medicine and Health Science. 2019/12/01/ 2019;1(1):3–10. doi:https://doi.org/10.1016/j.smhs.2019.08.006
Treadwell JR, Reston JT, Rouse B, Fontanarosa J, Patel N, Mull NK. Automated-Entry Patient-Generated Health Data for Chronic Conditions: The Evidence on Health Outcomes. 2021. Technical Brief. 21-EHC012.
Slevin P, Kessie T, Cullen J, Butler MW, Donnelly SC, Caulfield B. A qualitative study of chronic obstructive pulmonary disease patient perceptions of the barriers and facilitators to adopting digital health technology. DIGITAL HEALTH. 2019/01/01 2019;5:2055207619871729. doi:https://doi.org/10.1177/2055207619871729
Boersma P, Cohen R, Zelaya C, Moy E. Multiple Chronic Conditions Among Veterans and Nonveterans: United States, 2015–2018. Vol. 153. U.S. Department of Health and Human Services; 2021. National Health Statistics Report. February 23, 2021. Accessed July 14, 2022. https://www.cdc.gov/nchs/data/nhsr/nhsr153-508.pdf
Chan AHY, Pleasants RA, Dhand R, et al. Digital Inhalers for Asthma or Chronic Obstructive Pulmonary Disease: A Scientific Perspective. Pulm Ther. Dec 2021;7(2):345-376. doi:https://doi.org/10.1007/s41030-021-00167-4
Ferguson C, Hickman LD, Turkmani S, Breen P, Gargiulo G, Inglis SC. “Wearables only work on patients that wear them”: Barriers and facilitators to the adoption of wearable cardiac monitoring technologies. Cardiovascular Digital Health Journal. 2021/04/01/ 2021;2(2):137–147. doi:https://doi.org/10.1016/j.cvdhj.2021.02.001
McNeal DM, Fehling K, Ho PM, et al. Engaging Stakeholders in Identifying Access Research Priorities for the Department of Veterans Affairs. Journal of General Internal Medicine. 2022/04/01 2022;37(1):14–21. doi:https://doi.org/10.1007/s11606-021-07195-5
Current Population Survey: Veteran Supplement. Accessed August 23, 2023. https://data.census.gov/mdat
Bernard D, Woodroffe A, Liu S. Understanding Veterans’ Healthcare Use and Experience, 2018–2019 November 2022. Research Findings #50. https://meps.ahrq.gov/data_files/publications/rf50/rf50.pdf
Eibner C, Krull H, Brown KM, et al. Current and Projected Characteristics and Unique Health Care Needs of the Patient Population Served by the Department of Veterans Affairs. RAND Health Quarterly. 2016;5(4)
Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The Digital Divide in Health-Related Technology Use: The Significance of Race/Ethnicity. The Gerontologist. 2019;59(1):6-14. doi:https://doi.org/10.1093/geront/gny138
Mobile Fact Sheet. Pew Research Center. Accessed July 14, 2022, https://www.pewresearch.org/internet/fact-sheet/mobile/
Jaworski BK, Taylor K, Ramsey KM, et al. Predicting Uptake of the COVID Coach App Among US Military Veterans: Funnel Analysis Using a Probability-Based Panel. JMIR Mental Health. 2022;9(4):e36217. doi:https://doi.org/10.2196/36217
Zulman DM, Wong EP, Slightam C, et al. Making connections: nationwide implementation of video telehealth tablets to address access barriers in veterans. JAMIA Open. 2019;2(3):323-329. doi:https://doi.org/10.1093/jamiaopen/ooz024
Hogan TP, Nazi KM, Luger TM, et al. Technology-assisted patient access to clinical information: an evaluation framework for blue button. JMIR Res Protoc. 2014;3(1):18-18. doi:https://doi.org/10.2196/resprot.3290
Shimada SL, Allison JJ, Rosen AK, Feng H, Houston TK. Sustained Use of Patient Portal Features and Improvements in Diabetes Physiological Measures. J Med Internet Res. 2016/07/01 2016;18(7):e179. doi:https://doi.org/10.2196/jmir.5663
Shimada SL, Brandt CA, Feng H, et al. Personal Health Record Reach in the Veterans Health Administration: A Cross-Sectional Analysis. J Med Internet Res. 2014/12/12 2014;16(12):e272. doi:https://doi.org/10.2196/jmir.3751
Funding
This work was supported by the US Department of Veterans Affairs, Office of Connected Care, and Office of Research and Development, Health Services Research and Development Service, Quality Enhancement Research Initiative Program (PEC 15–470; principal investigator: TPH). The views expressed in this article are those of the authors and do not necessarily reflect the position and/or policy of the Department of Veterans Affairs or of the United States Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations
Some of the contents of this manuscript were presented at the 2023 Department of Veterans Affairs Health Services Research & Development Conference, February 10, 2023, and the AcademyHealth 2023 Annual Research Meeting, June 27, 2023.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Robinson, S.A., Shimada, S.L., Zocchi, M.S. et al. Factors Associated with Veteran Self-Reported Use of Digital Health Devices. J GEN INTERN MED 39 (Suppl 1), 79–86 (2024). https://doi.org/10.1007/s11606-023-08479-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08479-8