Abstract
Background
Both increases and decreases in patients’ prescribed daily opioid dose have been linked to increased overdose risk, but associations between 30-day dose trajectories and subsequent overdose risk have not been systematically examined.
Objective
To examine the associations between 30-day prescribed opioid dose trajectories and fatal opioid overdose risk during the subsequent 15 days.
Design
Statewide cohort study using linked prescription drug monitoring program and death certificate data. We constructed a multivariable Cox proportional hazards model that accounted for time-varying prescription-, prescriber-, and pharmacy-level factors.
Participants
All patients prescribed an opioid analgesic in California from March to December, 2013 (5,326,392 patients).
Main Measures
Dependent variable: fatal drug overdose involving opioids. Primary independent variable: a 16-level variable denoting all possible opioid dose trajectories using the following categories for current and 30-day previously prescribed daily dose: 0-29, 30-59, 60-89, or ≥90 milligram morphine equivalents (MME).
Key Results
Relative to patients prescribed a stable daily dose of 0-29 MME, large (≥2 categories) dose increases and having a previous or current dose ≥60 MME per day were associated with significantly greater 15-day overdose risk. Patients whose dose decreased from ≥90 to 0-29 MME per day had significantly greater overdose risk compared to both patients prescribed a stable daily dose of ≥90 MME (aHR 3.56, 95%CI 2.24-5.67) and to patients prescribed a stable daily dose of 0-29 MME (aHR 7.87, 95%CI 5.49-11.28). Patients prescribed benzodiazepines also had significantly greater overdose risk; being prescribed Z-drugs, carisoprodol, or psychostimulants was not associated with overdose risk.
Conclusions
Large (≥2 categories) 30-day dose increases and decreases were both associated with increased risk of fatal opioid overdose, particularly for patients taking ≥90 MME whose opioids were abruptly stopped. Results align with 2022 CDC guidelines that urge caution when reducing opioid doses for patients taking long-term opioid for chronic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Prescribed opioid dose has long been recognized as an important risk factor for opioid-related overdose deaths. The initial studies that raised safety concerns about opioid analgesics all identified higher prescribed daily dose (measured in milligram morphine equivalents, MME) as a significant overdose risk factor.1,2,3 In response to these and other studies, the Centers for Disease Control and Prevention (CDC) issued guidelines in 2016 that discouraged clinicians from prescribing opioids for pain and strongly discouraged prescribing high doses.4 These guidelines catalyzed shifts in clinical practice away from opioid prescribing and led health systems, health insurers, and state lawmakers to impose dose-based restrictions on opioid prescribing.5,6,7,8
Shifts away from overprescribing were needed to reduce rates of opioid use disorder and overdose. However, recent studies indicate that decreasing patients’ prescribed opioid dose is also risky and is associated with increased rates of overdose,9,10,11 suicide,12, 13 and disruptions in care,14, 15 particularly for patients with physical opioid dependence or whose prescriptions are stopped abruptly. Unfortunately, most studies have limited power to examine how changes in prescribed dose affect overdose risk because fatal overdose events are rare among all patients prescribed opioids. Given this limitation, some studies have grouped patients based on long-term trajectories in their prescribed daily opioid dose.16,17,18 Most prior multivariable studies of overdose risk have analyzed opioid dose using mean daily dose as a either a categorical19,20,21,22 or binary23 variable; others have used total dose,24,25,26 maximum daily dose,27 or dose variability28 over a specific time period.
To our knowledge, no prior studies have examined the impact of patients’ short-term opioid dose trajectories on overdose risk across the full range of clinically important dose categories. As noted above, prior studies indicate that receipt of high-dose opioids as well as both increases and decreases in prescribed opioid dose can impact overdose risk in multiple ways that are difficult to disentangle without huge sample sizes. For example, dose increases can worsen opioid-related respiratory depression, while decreases can precipitate withdrawal or prompt risky behavior among patients with opioid use disorder. We conducted a large statewide cohort study to provide better data to clinicians and policymakers on how short-term changes in opioid dose affect overdose risk to help them make safer clinical decisions and design more nuanced prescribing policies, particularly for patients prescribed opioids for chronic pain.
METHODS
Overview
We analyzed statewide time-to-event data in a cohort comprising all patients ages 12 and older with any opioid prescription recorded in California’s prescription drug monitoring program database between March 1 and December 31, 2013. Our primary independent variable was a categorical, time-varying indicator denoting the trajectory of patients’ prescribed daily opioid dose over the previous 30 days. Our dependent variable was fatal opioid overdose during the subsequent 15 days measured using California death certificate records. Patients’ trajectories and outcomes were assessed in 15-day intervals through December 31, 2013. We chose 2013 because, prior to the 2016 CDC guidelines, both overall opioid prescribing and variation in prescribed opioid dose were much greater than they are today, increasing our ability to examine the inherent risks associated with dose changes. Moreover, most opioid-related deaths in 2013 involved prescription rather than illicit opioids; overdoses involving illicit synthetic opioids, particularly fentanyl, were rare in California before 2016.29
This study was approved by the California Committee for the Protection of Human Subjects and the University of California, Davis Institutional Review Board.
Data sources
Controlled substance prescription data were obtained from California's prescription drug monitoring program, which contains records for all outpatient Schedule II-IV prescriptions dispensed in California. In addition to prescriber and pharmacy identifiers, each prescription record included date dispensed, National Drug Codes, quantity, strength per unit, days’ supply, patient sex, date of birth, name, and address.
Statewide death certificate records were obtained from the California Department of Public Health. Each record was linked to the CDC’s Multiple Cause of Death file, which assigns one ICD-10 code for the underlying cause of death and up to 20 additional ICD-10 codes for contributing causes of death to each death certificate.
Data linkage
We linked 2013 death certificate and prescription drug records using The Link King,30 a publicly available SAS record linkage program that performs deterministic and probabilistic linkage31 and performs well on prescription drug monitoring program data.32 We first assigned a unique identifier to each death record and then identified all prescription records that matched to each death record. We then linked all prescription records not already associated with a death record that the program identified as belonging to the same person. We used the resulting patient-level file to identify our study cohort.
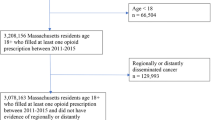
Cohort construction
Our cohort included all patients in California who filled any Schedule II-IV opioid analgesic prescription between March 1 and December 31, 2013, and who were between 12 and 111 years old when they filled their first prescription. Data from other projects33 indicate that 98% of opioid prescriptions in November and December 2012 had days’ supply ≤30. We therefore chose March 1, 2013, as the earliest inclusion date because it was the first date for which we had complete data on prescribed opioid dose for both the date of assessment and the date 30 days previously. We excluded prescriptions to animals, duplicate prescriptions, prescriptions with missing fill date, with missing or zero quantity, or prescriptions filled after a patient’s date of death (see Fig. 1).
Variable construction
Our dependent variable was a drug overdose death involving any opioids as defined by the CDC34: specifically, any underlying cause of death code indicating drug poisoning (X40-X44, X60-X64, X85, Y10-Y14) and any multiple cause-of-death code indicating opioids (T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6). In a sensitivity analysis, we used overdoses involving prescription opioids (i.e., by excluding overdoses that involved heroin, T40.1) as the dependent variable. Patient status and all time-varying independent variables were assessed in 15-day increments.
Our primary, time-varying independent variable was prescribed daily opioid dose. We calculated patients’ daily dose using standard conversion factors4 to calculate total prescribed dose in MME and then dividing that total by the prescription’s days’ supply. When patients had multiple active opioid prescriptions, we summed the daily dose for all prescriptions. Consistent with CDC recommendations, we set the conversion factor for buprenorphine (2% of all opioid prescriptions) to zero because of its unique pharmacodynamics and risk profile.4, 35 Finally, we grouped daily dose into 4 ordinal categories: 0-29 MME, 30-59 MME, 60-89 MME, and ≥90 MME. To evaluate the impact of 30-day prescribed opioid dose trajectories, we created a 16-level variable for all possible combinations of patients’ current daily dose and their daily dose 30 days previously, using the same 4 categories for each.
We identified additional independent variables through a literature review and our own prior work.33, 36 Patient sex (male, female, unknown) and age (12-24, 25-64, ≥65) were analyzed as fixed variables. All other variables were time varying.
Additional opioid-related independent variables included indicators for whether patients had 1) any active opioid prescription, 2) two or more active opioid prescriptions, 3) any active prescription for a long-acting opioid formulation, 4) any active prescription for a liquid opioid formulation, and 5) any active prescription for a transdermal opioid (i.e., non-pill, non-liquid) formulation. A categorical variable for opioid type (hydrocodone, oxycodone, morphine, buprenorphine, codeine, fentanyl, methadone, hydromorphone, other, multiple types) was also included. Tramadol was not added to Schedule IV until 2014 and so was not included in our study data.
To account for risks associated with receiving opioids from multiple prescribers and pharmacies, we included indicator time-varying variables identifying whether patients had active prescriptions 1) written by two or more different prescribers and 2) filled by two or more different pharmacies.
To account for risks associated with concomitant use of other controlled substances, we included time-varying indicator variables identifying whether patients had an active prescription for 1) any benzodiazepine, 2) carisoprodol, 3) any psychostimulant, and 4) any Z drug (zolpidem, eszopiclone, or zaleplon).37 We included a 4-level variable describing the combination of patient’s current benzodiazepine status with their status 30 days previously.
Statistical analysis and model construction
We began by examining monthly counts of our outcome variable versus the month of each patient’s first opioid prescription and the distribution of independent variables among patients who did versus did not experience a fatal opioid overdose.
We then constructed a time-varying Cox proportional hazards model to examine the relationships between 30-day prescribed opioid dose trajectory and fatal overdose risk. Follow up time was measured from the day of each patient’s first opioid dose on or after March 1, 2013, until the patient first experienced the outcome, died of some other cause, or reached the end of the study period. The follow up period ranged from 0 to 305 days.
To construct the model, we first added patient age, sex, and 30-day prescribed opioid dose trajectory as independent variables. We then added other opioid-related prescription-level variables, prescriber- and pharmacy-level variables, and finally, variables for other controlled substance prescriptions. We parameterized the model based on avoiding multicollinearity and optimizing overall model fit by minimizing Akaike information criterion. We explored models that measured daily opioid dose using both quantity of pills and MME per day; MME-based models were superior. We chose cutoffs for ordinal opioid dose categories that reflected clinically relevant dose intervals; models with categories for higher doses (e.g., ≥120 MME) had wide confidence intervals and poor model fit due to influence from outlier values. When adding a new variable caused major changes in other parameter estimates, we examined variable distributions to determine why the estimates changed. The optimal parameterization for many independent variables was binary indicator variables. For example, parameterizing overlapping prescriptions using number of days of overlap did not improve model fit compared to using a binary variable indicating whether patients had two or more active opioid prescriptions. We constructed separate tables of parameter estimates for the 16-level trajectory variable to facilitate examining the impact of 30-day change in daily opioid dose on overdose risk. We used the same model for both primary and sensitivity analyses.
Data preparation and analyses were conducted using SAS 9.4 and R 4.2.1.
RESULTS
Figure 1 shows the flow chart for cohort construction. Our cohort comprised 5,326,392 patients who filled ≥1 opioid prescription between March 1 and December 31, 2013. Fewer than 1% of prescriptions had missing or duplicate data.
Over the study period, we recorded 797 overdose deaths involving opioids and 108,352 deaths from other causes. Table 1 shows the distribution of overdose deaths by month, stratified by the month of each patient’s first opioid dose. Nearly two-thirds (66%) of all overdoses occurred among patients who received their initial opioid prescription in March; 15% of all overdoses occurred among patients who received their first opioid prescription in April. As shown in Table 2, patients who died from an opioid-related overdose were more likely to be male and less likely to be age 65 years or older, compared to patients who did not. Approximately 22% of patients who died from an overdose were prescribed ≥90 MME per day both at the last assessment before their overdose and 30 days previously, compared to only 4% of patients who did not. Among patients who died from an overdose, 26% were not prescribed any opioids at either the last assessment before their overdose or 30 days previously Table 3.
Tables 4a summarizes overdose risk associated with 30-day prescribed opioid dose trajectories relative to a stable, low dose of 0-29 MME per day. Thirty-day dose increases from 0-29 MME per day to either 60-89 MME (aHR 1.98, 95%CI 1.22, 3.20) or ≥90 MME (aHR 3.35, 95%CI 2.24, 5.01) per day as well as from 30-59 MME to ≥90 MME per day (aHR 4.13, 95%CI 2.30, 7.41) were all associated with significantly increased overdose risk during the subsequent 15 days, as was having either a previous or current dose ≥60 MME per day (with one exception; the increased risk associated with a 30-day dose decrease from 60-89 MME to 30-59 MME per day was not significant; aHR 1.75, 95%CI 0.79-3.88).
Table 4b summarizes overdose risk associated with 30-day prescribed opioid dose trajectories relative to patients with the same previous dose and no change in dose over 30 days. Increases from 0-29 MME per day to either 60-89 MME or ≥90 MME per day were associated with significantly greater overdose risk (the reference category and parameter estimates for these patients were identical to those in Table 4a). The overdose risk associated with a 30-day increase from 30-59 MME to ≥90 MME per day also remained significant (aHR 2.92, 95%CI 1.63, 5.31). For patients with a previous dose of ≥60 MME per day, large dose reductions (≥2 categories) were all associated with increased overdose risk, but only the increased risk associated with a decrease from ≥90 MME to 0-29 MME per day was statistically significant compared to patients on a stable dose. Patients whose opioid dose decreased from ≥90 to 0-29 MME per day had a significantly greater overdose risk during the subsequent 15 days compared to both patients prescribed a stable daily dose of ≥90 MME (aHR 3.56, 95%CI 2.24-5.67) and to patients prescribed a stable daily dose of 0-29 MME (aHR 7.87, 95%CI 5.49-11.28). Thirty-nine of the 40 patients who had a fatal overdose associated with this trajectory had their opioid access interrupted completely (i.e., current dose = 0 MME per day) after previously being prescribed ≥90 MME per day.
Patients prescribed benzodiazepines had substantially greater overdose risk; patients prescribed benzodiazepines at their current assessment or 30 days previously had significantly greater risk than patients prescribed benzodiazepines at neither time point. Being prescribed Z-drugs, carisoprodol, or prescription stimulants was not associated with significantly greater overdose risk. Overall results for our sensitivity analysis excluding overdose deaths involving heroin were similar to the primary findings (Table S1).
DISCUSSION
This project examined the impact of 30-day prescribed opioid dose trajectories on patients’ risk of fatal opioid-related overdose for all patients in California in 2013. For patients prescribed low daily opioid doses, large dose increases (≥2 categories) over 30 days were associated with significant increases in overdose risk during the subsequent 15 days compared to staying at their previous dose. These findings align with recommendations in the CDC guidelines to prescribe patients the lowest effective opioid dose and avoid major dose increases over short periods of time.38
We also found that nearly all patients prescribed daily doses ≥60 MME faced significantly greater overdose risk than patients prescribed stable, low opioid doses regardless of whether their dose increased, decreased, or was stable over 30 days (Table 4a). Patients prescribed ≥60 MME per day who experienced large dose reductions (≥2 categories) were at increased overdose risk compared to patients prescribed stable, high doses; this increased risk was significantly greater for patients prescribed ≥90 MME per day whose opioids were abruptly stopped. These findings suggest that much of the increased overdose risk for these patients is due to their high (≥60 MME per day) baseline opioid dose rather than their 30-day dose trajectory. However, large dose decreases in these patients are associated with increased overdose risk.
Most importantly, our results underscore that, for patients taking ≥90 MME per day, abruptly stopping prescription opioids drastically increases risk of fatal overdose during the subsequent 15 days. These results are consistent with prior studies showing that among patients with likely physical dependence from long-term use, opioid discontinuation is associated with greater overdose risk than dose decreases without discontinuation.10, 11 Almost all patients prescribed ≥90 MME per day have physical opioid dependence and so may have sought illicit opioids when their prescriptions were stopped. In contrast, some patients may have had their prescriptions cut off because they had high overdose risk for other reasons (e.g., due to uncontrolled opioid use disorder). Regardless, our results underscore that clinicians should closely monitor all patients prescribed ≥90 MME per day, avoid unilaterally stopping opioids for these patients, obtain patient agreement before considering any dose changes, prescribe naloxone, and screen them for opioid use disorder. These recommendations align with the 2019 US Health and Human Services guidelines on opioid dose reduction and the revised 2022 CDC guidelines, which both urge caution when reducing opioid doses.38, 39
Many patients with physical opioid dependence must exert substantial mental and physical effort to successfully reduce their opioid consumption;40 these patients appear to remain at high risk for overdose, mental health crisis, and even all-cause mortality for months to years after an opioid dose reduction.13, 41 Some protocols for safely reducing patient’s prescribed opioid dose have shown promise.42, 43 Transitioning patients to buprenorphine is another potential strategy to reduce overdose risk that will likely become more common since the X-waiver requirement was repealed in December 2022.
We believe our study is the first and largest to estimate the impact of 30-day prescribed opioid dose trajectories on overdose risk across the full range of clinically relevant dose trajectories. Our results are consistent with prior studies examining longer-term dose trajectories and showing that dose increases,44 decreases,9,10,11 and dose variability28 are all opioid overdose risk factors for patients with physical opioid dependence. Most of these prior studies lacked sufficient sample to examine overdose risks associated with short-term dose trajectories in granular detail.
In addition to findings around prescribed dose, our study examined fatal opioid overdose risk associated with other aspects of controlled substance prescribing. Despite widely publicized concerns about risks associated with carisoprodol, z-drugs, and psychostimulants,45 receiving these drug classes was not associated with fatal overdose risk after controlling for other independent variables. Similarly, neither receiving a long-acting opioid formulation nor receiving opioids from multiple prescribers or pharmacies was significantly associated with overdose risk in our model. Prior studies that identified these risk factors did not account for the full range of independent variables in our multivariable model.46,47,48 In contrast, our finding that benzodiazepine co-prescription substantially increases opioid overdose risk is consistent with prior studies on this topic;49, 50 additional research on specific patterns and trajectories of co-prescribing associated with overdose risk are needed to inform guidelines for this high-risk patient population.
Our study has limitations. We analyzed older data. Prescribing patterns are much different and rates of high-dose opioid prescribing are much lower today than they were in 2013, so our findings should be interpreted in an appropriate historical context. The inherent risks associated with prescription opioid use are likely stable over time, but replication of our analysis with more recent data can inform specific clinical or policy recommendations. We were unable to examine prescribed opioid dose trajectories for more than one 30-day increment because our data were limited to one calendar year; analyzing data with longer retrospective “look-back” and prospective follow up periods would allow evaluation of how short and long-term dose trajectories jointly impact overdose risk over longer periods of time. Finally, we did not have access to data about patients’ clinical characteristics, about methadone dispensed for addiction treatment, or, most importantly, about why patients’ prescribed dose was changed or abruptly stopped before an overdose. However, these weaknesses are counterbalanced by our use of population-based data from a large US state with a large number of overdose events. Datasets that include clinical and diagnostic data are nearly always restricted to specific insurers or health systems, and so lack either the statistical power or detailed cause-of-death information necessary to evaluate the impact of 30-day changes in prescribed opioid dose on overdose risk.
Data availability
Data supporting study findings are not available from the authors because data use agreements signed with the California Departments of Justice and Public Health preclude sharing data with third parties.
REFERENCES
Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Annals of internal medicine. 2010;152(2):85-92.
Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321.
Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686-691.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016;315(15):1624-1645.
Centers for Medicare & Medicaid Services. Medicare Program; Contract Year 2019 Policy and Technical Changes to the Medicare Advantage, Medicare Cost Plan, Medicare Fee-for-Service, the Medicare Prescription Drug Benefit Programs, and the PACE Program In: Department of Health and Human Services, ed. Vol 832018:16440-16757.
Davis CS, Lieberman AJ. Laws limiting prescribing and dispensing of opioids in the United States, 1989-2019. Addiction. 2021;116(7):1817-1827.
Heins SE, Frey KP, Alexander GC, Castillo RC. Reducing High-Dose Opioid Prescribing: State-Level Morphine Equivalent Daily Dose Policies, 2007-2017. Pain Med. 2020;21(2):308-316.
Bohnert ASB, Guy GP, Jr., Losby JL. Opioid Prescribing in the United States Before and After the Centers for Disease Control and Prevention's 2016 Opioid Guideline. Ann Intern Med. 2018;169(6):367-375.
Agnoli A, Xing GB, Tancredi DJ, Magnan E, Jerant A, Fenton JJ. Association of Dose Tapering With Overdose or Mental Health Crisis Among Patients Prescribed Long-term Opioids. Jama-J Am Med Assoc. 2021;326(5):411-419.
Larochelle MR, Lodi S, Yan S, Clothier BA, Goldsmith ES, Bohnert ASB. Comparative Effectiveness of Opioid Tapering or Abrupt Discontinuation vs No Dosage Change for Opioid Overdose or Suicide for Patients Receiving Stable Long-term Opioid Therapy. JAMA Netw Open. 2022;5(8):e2226523.
DiPrete BL, Ranapurwala SI, Maierhofer CN, et al. Association of Opioid Dose Reduction With Opioid Overdose and Opioid Use Disorder Among Patients Receiving High-Dose, Long-term Opioid Therapy in North Carolina. JAMA Netw Open. 2022;5(4):e229191.
Hallvik SE, El Ibrahimi S, Johnston K, et al. Patient outcomes following opioid dose reduction among patients with chronic opioid therapy. Pain. 2022;163(1):83-90.
Fenton JJ, Magnan E, Tseregounis IE, Xing G, Agnoli AL, Tancredi DJ. Long-term Risk of Overdose or Mental Health Crisis After Opioid Dose Tapering. JAMA Netw Open. 2022;5(6):e2216726.
Perez HR, Buonora M, Cunningham CO, Heo M, Starrels JL. Opioid Taper Is Associated with Subsequent Termination of Care: a Retrospective Cohort Study. J Gen Intern Med. 2020;35(1):36-42.
Binswanger IA, Shetterly SM, Xu S, et al. Opioid Dose Trajectories and Associations With Mortality, Opioid Use Disorder, Continued Opioid Therapy, and Health Plan Disenrollment. JAMA Netw Open. 2022;5(10):e2234671.
Wei YJ, Chen C, Lewis MO, Schmidt SO, Winterstein AG. Trajectories of prescription opioid dose and risk of opioid-related adverse events among older Medicare beneficiaries in the United States: A nested case-control study. PLoS Med. 2022;19(3):e1003947.
Rikard SM, Nataraj N, Zhang K, Strahan AE, Mikosz CA, Guy GP, Jr. Longitudinal dose patterns among patients newly initiated on long-term opioid therapy in the United States, 2018 to 2019: an observational cohort study and time-series cluster analysis. Pain. 2023.
Gisev N, Buizen L, Hopkins RE, et al. Five-Year Trajectories of Prescription Opioid Use. JAMA Netw Open. 2023;6(8):e2328159.
Ferris LM, Saloner B, Krawczyk N, et al. Predicting Opioid Overdose Deaths Using Prescription Drug Monitoring Program Data. Am J Prev Med. 2019;57(6):e211-e217.
Metcalfe L, Murrelle EL, Vu L, et al. Independent Validation in a Large Privately Insured Population of the Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or Overdose. Pain Med. 2020;21(10):2219-2228.
Lin LA, Brummett CM, Waljee JF, Englesbe MJ, Gunaseelan V, Bohnert ASB. Association of Opioid Overdose Risk Factors and Naloxone Prescribing in US Adults. J Gen Intern Med. 2020;35(2):420-427.
Garg RK, Fulton-Kehoe D, Franklin GM. Patterns of Opioid Use and Risk of Opioid Overdose Death Among Medicaid Patients. Med Care. 2017;55(7):661-668.
Geissert P, Hallvik S, Van Otterloo J, et al. High-risk prescribing and opioid overdose: prospects for prescription drug monitoring program-based proactive alerts. Pain. 2018;159(1):150-156.
Lo-Ciganic WH, Huang JL, Zhang HH, et al. Evaluation of Machine-Learning Algorithms for Predicting Opioid Overdose Risk Among Medicare Beneficiaries With Opioid Prescriptions. JAMA Netw Open. 2019;2(3):e190968.
Dong X, Rashidian S, Wang Y, et al. Machine Learning Based Opioid Overdose Prediction Using Electronic Health Records. AMIA Annu Symp Proc. 2019;2019:389-398.
Saloner B, Chang HY, Krawczyk N, et al. Predictive Modeling of Opioid Overdose Using Linked Statewide Medical and Criminal Justice Data. JAMA psychiatry. 2020;77(11):1155-1162.
Zedler BK, Saunders WB, Joyce AR, Vick CC, Murrelle EL. Validation of a Screening Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or Overdose in a US Commercial Health Plan Claims Database. Pain Med. 2018;19(1):68-78.
Glanz JM, Binswanger IA, Shetterly SM, Narwaney KJ, Xu S. Association Between Opioid Dose Variability and Opioid Overdose Among Adults Prescribed Long-term Opioid Therapy. JAMA Netw Open. 2019;2(4):e192613.
California Department of Public Health. California Opioid Overdose Surveillance Dashboard. https://skylab.cdph.ca.gov/ODdash/. Updated 2019. Accessed October 3, 2022, 2022.
Campbell KM. The Link King v9.0. http://www.the-link-king.party. Accessed May 23, 2022, 2022.
Fellegi IP, Sunter AB. A Theory for Record Linkage. J Am Stat Assoc. 1969;64(328):1183-1210.
Mohanty AF, Crook J, Porucznik CA, Johnson EM, Rolfs RT, Sauer BC. Development and evaluation of a record linkage protocol for Utah's Controlled Substance Database. Health informatics journal. 2017;23(1):35-43.
Henry SG, Stewart SL, Murphy E, et al. Using Prescription Drug Monitoring Program Data to Assess Likelihood of Incident Long-Term Opioid Use: a Statewide Cohort Study. J Gen Intern Med. 2021;36(12):3672-3679.
Centers for Disease Control and Prevention. Prevention for States Indicator Support Toolkit. March 23, 2018.
Coe MA, Lofwall MR, Walsh SL. Buprenorphine Pharmacology Review: Update on Transmucosal and Long-acting Formulations. J Addict Med. 2019;13(2):93-103.
Tseregounis IE, Henry SG. Assessing opioid overdose risk: a review of clinical prediction models utilizing patient-level data. Transl Res. 2021.
Szmulewicz A, Bateman BT, Levin R, Huybrechts KF. The Risk of Overdose With Concomitant Use of Z-Drugs and Prescription Opioids: A Population-Based Cohort Study. The American journal of psychiatry. 2021;178(7):643-650.
Dowell D, Ragan K, Jones C, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids–United States, 2022. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports / Centers for Disease Control. 2022;71(3):1-98.
HHS Guide for Clinicians on the Appropriate Dosage Reduction or Discontinuation of Long-Term Opioid Analgesics. US Department of Health and Human Services. https://www.hhs.gov/opioids/sites/default/files/2019-10/8-Page%20version__HHS%20Guidance%20for%20Dosage%20Reduction%20or%20Discontinuation%20of%20Opioids.pdf. Published 2019. Accessed 2 may 2020, 2020.
Henry SG, Paterniti DA, Feng B, et al. Patients' experience with opioid tapering: A conceptual model with recommendations for clinicians. J Pain. 2019;20(2):181-191.
Gordon KS, Manhapra A, Crystal S, et al. All-cause mortality among males living with and without HIV initiating long-term opioid therapy, and its association with opioid dose, opioid interruption and other factors. Drug and alcohol dependence. 2020;216:108291.
Sullivan MD, Boudreau D, Ichikawa L, et al. Primary Care Opioid Taper Plans Are Associated with Sustained Opioid Dose Reduction. J Gen Intern Med. 2020;35(3):687-695.
Sullivan MD, Turner JA, DiLodovico C, D'Appollonio A, Stephens K, Chan YF. Prescription Opioid Taper Support for Outpatients With Chronic Pain: A Randomized Controlled Trial. J Pain. 2017;18(3):308-318.
Hser YI, Saxon AJ, Mooney LJ, et al. Escalating Opioid Dose Is Associated With Mortality: A Comparison of Patients With and Without Opioid Use Disorder. J Addict Med. 2019;13(1):41-46.
Wang Y, Delcher C, Li Y, Goldberger BA, Reisfield GM. Overlapping prescriptions of opioids, benzodiazepines, and carisoprodol: "Holy Trinity" prescribing in the state of Florida. Drug and alcohol dependence. 2019;205:107693.
Yang Z, Wilsey B, Bohm M, et al. Defining risk of prescription opioid overdose: pharmacy shopping and overlapping prescriptions among long-term opioid users in medicaid. J Pain. 2015;16(5):445-453.
Baumblatt JA, Wiedeman C, Dunn JR, Schaffner W, Paulozzi LJ, Jones TF. High-Risk Use by Patients Prescribed Opioids for Pain and Its Role in Overdose Deaths. JAMA internal medicine. 2014;174(5):796-801.
Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. JAMA. 2016;315(22):2415-2423.
Hernandez I, He M, Brooks MM, Zhang Y. Exposure-Response Association Between Concurrent Opioid and Benzodiazepine Use and Risk of Opioid-Related Overdose in Medicare Part D Beneficiaries. JAMA Network Open. 2018;1(2):e180919-e180919.
Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert ASB. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ. 2015;360:h2698.
Funding
This study was funded by National Institutes of Health grant R01DA044282. The funder had no input into study design, results interpretation, or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 19 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Henry, S.G., Fang, SY., Crawford, A.J. et al. Impact of 30-day prescribed opioid dose trajectory on fatal overdose risk: A population-based, statewide cohort study. J GEN INTERN MED 39, 393–402 (2024). https://doi.org/10.1007/s11606-023-08419-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08419-6