Abstract
Background
Social risks contribute to poor health outcomes, especially for patients with complex medical needs. These same risks may impact access to primary care services.
Objective
To study associations between social risks and primary care utilization among patients with medical complexity.
Design
Prospective cohort study of respondents to a 2018 mailed survey, followed up to 2 years after survey completion.
Participants
Nationally representative sample of 10,000 primary care patients in the Veterans Affairs (VA) health care system, with high (≥ 75th percentile) 1-year risk of hospitalization or death.
Main Measures
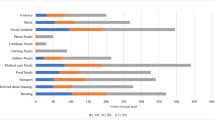
Survey-based exposures were low social support, no family member/friend involved in health care, unemployment, transportation problem, food insecurity, medication insecurity, financial strain, low medical literacy, and less than high school graduate. Electronic health record–based outcomes were number of primary care provider (PCP) encounters, number of primary care team encounters (PCP, nurse, clinical pharmacist, and social worker), and having ≥ 1 social work encounter.
Key Results
Among 4680 respondents, mean age was 70.3, 93.7% were male, 71.8% White non-Hispanic, and 15.8% Black non-Hispanic. Unemployment was associated with fewer PCP and primary care team encounters (incident rate ratio 0.77, 95% CI 0.65–0.91; p = 0.002 and 0.75, 0.59–0.95; p = 0.02, respectively), and low medical literacy was associated with more primary care team encounters (1.17, 1.05–1.32; p = 0.006). Among those with one or more social risks, 18.4% had ≥ 1 social work encounter. Low medical literacy (OR 1.95, 95% CI 1.45–2.61; p < 0.001), transportation problem (1.42, 1.10–1.83; p = 0.007), and low social support (1.31, 1.06–1.63; p = 0.01) were associated with higher odds of ≥ 1 social work encounter.
Conclusions
We found few differences in PCP and primary care team utilization among medically complex VA patients by social risk. However, social work use was low, despite its central role in addressing social risks. More work is needed to understand barriers to social work utilization.

Similar content being viewed by others

References
Davidson KW, Krist AH, Tseng CW, et al. Incorporation of Social Risk in US Preventive Services Task Force Recommendations and Identification of Key Challenges for Primary Care. JAMA. 2021;326(14):1410-1415. doi:https://doi.org/10.1001/jama.2021.12833.
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep Wash DC 1974. 2014;129 Suppl 2(Suppl 2):19-31. doi:https://doi.org/10.1177/00333549141291S206.
Knighton AJ, Stephenson B, Savitz LA. Measuring the Effect of Social Determinants on Patient Outcomes: A Systematic Literature Review. J Health Care Poor Underserved. 2018;29(1):81-106. doi:https://doi.org/10.1353/hpu.2018.0009.
Krause TM, Schaefer C, Highfield L. The association of social determinants of health with health outcomes. Am J Manag Care. 2021;27(3):e89-e96. doi:https://doi.org/10.37765/ajmc.2021.88603.
von dem Knesebeck O, Bickel H, Fuchs A, et al. Social inequalities in patient-reported outcomes among older multimorbid patients--results of the MultiCare cohort study. Int J Equity Health. 2015;14:17. doi:https://doi.org/10.1186/s12939-015-0142-6.
Coughlin SS, Datta B, Berman A, Hatzigeorgiou C. A cross-sectional study of financial distress in persons with multimorbidity. Prev Med Rep. 2021;23:101464. doi:https://doi.org/10.1016/j.pmedr.2021.101464.
McGilton KS, Vellani S, Yeung L, et al. Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: a scoping review. BMC Geriatr. 2018;18(1):231. doi:https://doi.org/10.1186/s12877-018-0925-x.
Daniel H, Bornstein SS, Kane GC, et al. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577-578. doi:https://doi.org/10.7326/M17-2441.
Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873-898. doi:https://doi.org/10.1161/CIR.0000000000000228.
Byhoff E, Kangovi S, Berkowitz SA, et al. A Society of General Internal Medicine Position Statement on the Internists’ Role in Social Determinants of Health. J Gen Intern Med. 2020;35(9):2721-2727. doi:https://doi.org/10.1007/s11606-020-05934-8.
National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019.
Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. The National Academies Press; 2014. https://doi.org/10.17226/18951.
Houlihan J, Leffler S. Assessing and Addressing Social Determinants of Health: A Key Competency for Succeeding in Value-Based Care. Prim Care. 2019;46(4):561-574. doi:https://doi.org/10.1016/j.pop.2019.07.013.
Castrucci BC, Auerbach J. Meeting Individual Social Needs Falls Short Of Addressing Social Determinants Of Health. Health Affairs Forefront. Published January 16, 2019. Accessed 29 May 2022. https://www.healthaffairs.org/do/10.1377/forefront.20190115.234942//.
Gurewich D, Garg A, Kressin NR. Addressing Social Determinants of Health Within Healthcare Delivery Systems: a Framework to Ground and Inform Health Outcomes. J Gen Intern Med. 2020;35(5):1571-1575. doi:https://doi.org/10.1007/s11606-020-05720-6.
LaForge K, Gold R, Cottrell E, et al. How 6 Organizations Developed Tools and Processes for Social Determinants of Health Screening in Primary Care: An Overview. J Ambulatory Care Manage. 2018;41(1):2-14. doi:https://doi.org/10.1097/JAC.0000000000000221.
Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities--Addressing Social Needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. doi:https://doi.org/10.1056/NEJMp1512532.
Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals. JAMA Netw Open. 2019;2(9):e1911514. doi:https://doi.org/10.1001/jamanetworkopen.2019.11514.
American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, and American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home.; 2007. Accessed 29 May 2022. https://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf.
Garg A, Jack B, Zuckerman B. Addressing the social determinants of health within the patient-centered medical home: lessons from pediatrics. JAMA. 2013;309(19):2001-2002. doi:https://doi.org/10.1001/jama.2013.1471.
Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for U.S. adults. Health Serv Res. 2012;47(1 Pt 2):462-485. doi:https://doi.org/10.1111/j.1475-6773.2011.01308.x.
Butkus R, Rapp K, Cooney TG, Engel LS. Envisioning a Better U.S. Health Care System for All: Reducing Barriers to Care and Addressing Social Determinants of Health. Ann Intern Med. 2020;172(2 Suppl):S50-S59. doi:https://doi.org/10.7326/M19-2410.
Deb S, Miller NA. Relations among race/ethnicity, gender, and mental health status in primary care use. Psychiatr Rehabil J. 2017;40(2):233-243. doi:https://doi.org/10.1037/prj0000230.
Donald M, Ware RS, Ozolins IZ, Begum N, Crowther R, Bain C. The role of patient activation in frequent attendance at primary care: a population-based study of people with chronic disease. Patient Educ Couns. 2011;83(2):217-221. doi:https://doi.org/10.1016/j.pec.2010.05.031.
Hooker SA, Stadem P, Sherman MD, Ricco J. Patient loneliness in an urban, underserved family medicine residency clinic: prevalence and relationship to health care utilization. Fam Pract. Published online July 7, 2020. doi:https://doi.org/10.1093/fampra/cmaa065.
Taylor YJ, Spencer MD, Mahabaleshwarkar R, Ludden T. Racial/ethnic differences in healthcare use among patients with uncontrolled and controlled diabetes. Ethn Health. 2019;24(3):245-256. doi:https://doi.org/10.1080/13557858.2017.1315372.
Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care by veterans with psychiatric illness in the National Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835-1840. doi:https://doi.org/10.1007/s11606-008-0786-7.
Cunningham A, Mautner D, Ku B, Scott K, LaNoue M. Frequent emergency department visitors are frequent primary care visitors and report unmet primary care needs. J Eval Clin Pract. 2017;23(3):567-573. doi:https://doi.org/10.1111/jep.12672.
Folsom DP, McKibbin C, Jeste DV, Patterson T. Use of Primary Care and by Middle Aged and Older Persons with Schizophrenia. Prim Care Community Psychiatry. 2006;11(3):101-106. doi:https://doi.org/10.1185/135525706X121174.
Ford JD, Trestman RL, Steinberg K, Tennen H, Allen S. Prospective association of anxiety, depressive, and addictive disorders with high utilization of primary, specialty and emergency medical care. Soc Sci Med 1982. 2004;58(11):2145-2148. doi:https://doi.org/10.1016/j.socscimed.2003.08.017.
Fortney JC, Maciejewski ML, Warren JJ, Burgess JF. Does improving geographic access to VA primary care services impact patients’ patterns of utilization and costs? Inq J Med Care Organ Provis Financ. 2005;42(1):29-42. doi:https://doi.org/10.5034/inquiryjrnl_42.1.29.
Riley ED, Wu AW, Junge B, Marx M, Strathdee SA, Vlahov D. Health services utilization by injection drug users participating in a needle exchange program. Am J Drug Alcohol Abuse. 2002;28(3):497-511. doi:https://doi.org/10.1081/ada-120006738.
Wong ST, Peterson S, Black C. Patient activation in primary healthcare: a comparison between healthier individuals and those with a chronic illness. Med Care. 2011;49(5):469-479. doi:https://doi.org/10.1097/MLR.0b013e31820bf970.
Banerjee S, Radak T, Khubchandani J, Dunn P. Food Insecurity and Mortality in American Adults: Results From the NHANES-Linked Mortality Study. Health Promot Pract. 2021;22(2):204-214. doi:https://doi.org/10.1177/1524839920945927.
Tan J, Wang Y. Social Integration, Social Support, and All-Cause, Cardiovascular Disease and Cause-Specific Mortality: A Prospective Cohort Study. Int J Environ Res Public Health. 2019;16(9). doi:https://doi.org/10.3390/ijerph16091498.
Canterberry M, Figueroa JF, Long CL, et al. Association Between Self-reported Health-Related Social Needs and Acute Care Utilization Among Older Adults Enrolled in Medicare Advantage. JAMA Health Forum. 2022;3(7):e221874. doi:https://doi.org/10.1001/jamahealthforum.2022.1874.
Zulman DM, Maciejewski ML, Grubber JM, et al. Patient-Reported Social and Behavioral Determinants of Health and Estimated Risk of Hospitalization in High-Risk Veterans Affairs Patients. JAMA Netw Open. 2020;3(10):e2021457. doi:https://doi.org/10.1001/jamanetworkopen.2020.21457.
Wang L, Porter B, Maynard C, et al. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368-373. doi:https://doi.org/10.1097/MLR.0b013e31827da95a.
Greene L, Maciejewski ML, Grubber J, Smith VA, Blalock DV, Zulman DM. Association between patient-reported social, behavioral, and health factors and emergency department visits in high-risk VA patients. Health Serv Res. 2023;58(2):383-391. doi:https://doi.org/10.1111/1475-6773.14094.
Bigdeli M, Jacobs B, Tomson G, et al. Access to medicines from a health system perspective. Health Policy Plan. 2013;28(7):692-704. doi:https://doi.org/10.1093/heapol/czs108.
Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263-272.
Department of Veterans Affairs, Veterans Health Administration. Integrated Case Management Standards of Practice. Veterans Health Administration; 2019. Accessed 30 May 2022. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8489.
Beder J, Postiglione P. Social work in the Veterans Health Administration (VA) System: rewards, challenges, roles and interventions. Soc Work Health Care. 2013;52(5):421-433. doi:https://doi.org/10.1080/00981389.2012.737906.
US Department of Veterans Affairs Information Resource Center. VIReC Research User Guide: PSSG Geocoded Enrollee Files, 2015 Edition. US Department of Veterans Affairs, Health Services Research & Development Service, Information Resource Center; 2016.
U.S. Department of Veterans Affairs. Enrollment Priority Groups. Accessed 30 May 2022. https://www.va.gov/healthbenefits/resources/publications/IB10-441_enrollment_priority_groups.pdf.
US Department of Veterans Affairs Managerial Cost Accounting Office. Program Documents – FY21 Active Stop Codes. Accessed 30 May 2022. http://vaww.dss.med.va.gov/programdocs/pd_oident.asp.
Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS). Published online 2015. Accessed November 2, 2021. U.S. Agency for Healthcare Research and Quality.
Yoon J, Chee CP, Su P, Almenoff P, Zulman DM, Wagner TH. Persistence of High Health Care Costs among VA Patients. Health Serv Res. 2018;53(5):3898-3916. doi:https://doi.org/10.1111/1475-6773.12989.
Frayne S, Phibbs C, Saechao F, et al. Sourcebook: Women Veterans in the Veterans Health Administration. Volume 4: Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution. Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs; 2018. Accessed 4 Jan 2023. https://www.womenshealth.va.gov/WOMENSHEALTH/docs/WHS_Sourcebook_Vol-IV_508c.pdf.
Phillips SP. Defining and measuring gender: a social determinant of health whose time has come. Int J Equity Health. 2005;4:11. doi:https://doi.org/10.1186/1475-9276-4-11.
Lett E, Asabor E, Beltrán S, Cannon AM, Arah OA. Conceptualizing, Contextualizing, and Operationalizing Race in Quantitative Health Sciences Research. Ann Fam Med. 2022;20(2):157-163. doi:https://doi.org/10.1370/afm.2792.
Dordunoo D, Abernethy P, Kayuni J, McConkey S, Aviles-G ML. Dismantling “Race” in Health Research. Can J Nurs Res Rev Can Rech En Sci Infirm. Published online January 21, 2022:8445621221074849. doi:https://doi.org/10.1177/08445621221074849.
Dieleman JL, Chen C, Crosby SW, et al. US Health Care Spending by Race and Ethnicity, 2002-2016. JAMA. 2021;326(7):649-659. doi:https://doi.org/10.1001/jama.2021.9937.
Manuel JI. Racial/Ethnic and Gender Disparities in Health Care Use and Access. Health Serv Res. 2018;53(3):1407-1429. doi:https://doi.org/10.1111/1475-6773.12705.
Hayes SL, Salzberg CA, McCarthy D, et al. High-Need, High-Cost Patients: Who Are They and How Do They Use Health Care? The Commonwealth Fund. 2016; pub 1897 vol 26. Accessed 5 Jan 2023. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2016_aug_1897_hayes_who_are_high_need_high_cost_patients_v2.pdf
The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th Edition.; 2016. Accessed 30 May 2022. https://www.aapor.org/aapor_main/media/publications/standard-definitions20169theditionfinal.pdf.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. doi:https://doi.org/10.7326/0003-4819-147-8-200710160-00010.
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600-1620. doi:https://doi.org/10.1111/1475-6773.12730.
Armstrong B, Levesque O, Perlin JB, Rick C, Schectman G. Reinventing Veterans Health Administration: focus on primary care. J Healthc Manag Am Coll Healthc Exec. 2005;50(6):399-408; discussion 409.
Schall MW, Duffy T, Krishnamurthy A, et al. Improving patient access to the Veterans Health Administration’s primary care and specialty clinics. Jt Comm J Qual Saf. 2004;30(8):415-423. doi:https://doi.org/10.1016/s1549-3741(04)30047-x.
Leung LB, Rubenstein LV, Yoon J, et al. Veterans Health Administration Investments In Primary Care And Mental Health Integration Improved Care Access. Health Aff Proj Hope. 2019;38(8):1281-1288. doi:https://doi.org/10.1377/hlthaff.2019.00270.
Edes T, Kinosian B, Vuckovic NH, Nichols LO, Becker MM, Hossain M. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954-1961. doi:https://doi.org/10.1111/jgs.13030.
Darkins A, Ryan P, Kobb R, et al. Care Coordination/Home Telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E-Health Off J Am Telemed Assoc. 2008;14(10):1118-1126. doi:https://doi.org/10.1089/tmj.2008.0021.
U.S. Department of Veterans Affairs. Past rates: 2020 VA health care copay rates. Published October 12, 2022. Accessed 26 Apr 2023. https://www.va.gov/health-care/copay-rates/past-rates-2020/.
Blosnich JR, Dichter ME, Gurewich D, et al. Health Services Research and Social Determinants of Health in the Nation’s Largest Integrated Health Care System: Steps and Leaps in the Veterans Health Administration. Mil Med. 2020;185(9-10):e1353-e1356. doi:https://doi.org/10.1093/milmed/usaa067.
Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976-993. doi:https://doi.org/10.1007/s10900-013-9681-1.
Janio EA, Sorkin DH. Food insecurity and healthcare access, utilization, and quality among middle and later life adults in California. J Aging Health. 2021;33(3-4):171-186. doi:https://doi.org/10.1177/0898264320967563.
Fiori KP, Heller CG, Rehm CD, et al. Unmet Social Needs and No-Show Visits in Primary Care in a US Northeastern Urban Health System, 2018-2019. Am J Public Health. 2020;110(S2):S242-S250. doi:https://doi.org/10.2105/AJPH.2020.305717.
Chang ET, Zulman DM, Nelson KM, et al. Use of General Primary Care, Specialized Primary Care, and Other Veterans Affairs Services Among High-Risk Veterans. JAMA Netw Open. 2020;3(6). doi:https://doi.org/10.1001/jamanetworkopen.2020.8120.
Albright DL, Thyer BA, Waller RJ. Utilization of Outpatient Social Work Services Among Veterans with Combat-Related Polytrauma: A Review and Case Analysis. Mil Behav Health. 2019;7(1):4-13.
Huded JM, Lee A, Song S, et al. Association of a geriatric emergency department program with healthcare outcomes among veterans. J Am Geriatr Soc JAGS. 2022;70(2):601-608.
Brignone E, Gundlapalli AV, Blais RK, et al. Increased Health Care Utilization and Costs Among Veterans With a Positive Screen for Military Sexual Trauma. Med Care. 2017;55 Suppl 9 Suppl 2(9):S70-S77.
Berrett-Abebe J, Donelan K, Berkman B, Auerbach D, Maramaldi P. Physician and nurse practitioner perceptions of social worker and community health worker roles in primary care practices caring for frail elders: Insights for social work. Soc Work Health Care. 2020;59(1):46-60. doi:https://doi.org/10.1080/00981389.2019.1695703.
Hamity C, Jackson A, Peralta L, Bellows J. Perceptions and Experience of Patients, Staff, and Clinicians with Social Needs Assessment. Perm J. 2018;22:18-105. doi:https://doi.org/10.7812/TPP/18-105.
Kostelanetz S, Pettapiece-Phillips M, Weems J, et al. Health Care Professionals’ Perspectives on Universal Screening of Social Determinants of Health: A Mixed-Methods Study. Popul Health Manag. Published online October 25, 2021. doi:https://doi.org/10.1089/pop.2021.0176.
Cornell PY, Halladay CW, Ader J, et al. Embedding Social Workers In Veterans Health Administration Primary Care Teams Reduces Emergency Department Visits. Health Aff Proj Hope. 2020;39(4):603-612. doi:https://doi.org/10.1377/hlthaff.2019.01589.
Fraser MW, Lombardi BM, Wu S, de Saxe Zerden L, Richman EL, Fraher EP. Integrated Primary Care and Social Work: A Systematic Review. J Soc Soc Work Res. 2018;9(2):175-215.
McGregor J, Mercer SW, Harris FM. Health benefits of primary care social work for adults with complex health and social needs: a systematic review. Health Soc Care Community. 2018;26(1):1-13. doi:https://doi.org/10.1111/hsc.12337.
Sommers LS, Marton KI, Barbaccia JC, Randolph J. Physician, nurse, and social worker collaboration in primary care for chronically ill seniors. Arch Intern Med. 2000;160(12):1825-1833. doi:https://doi.org/10.1001/archinte.160.12.1825.
Cohen AJ, Russell LE, Elwy AR, et al. Adaptation of a social risk screening and referral initiative across clinical populations, settings, and contexts in the Department of Veterans Affairs Health System. Front Health Serv. 2022;2:958969. doi:https://doi.org/10.3389/frhs.2022.958969.
Shepardson RL, Johnson EM, Possemato K, Arigo D, Funderburk JS. Perceived barriers and facilitators to implementation of peer support in Veterans Health Administration Primary Care-Mental Health Integration settings. Psychol Serv. 2019;16(3):433-444. doi:https://doi.org/10.1037/ser0000242.
Sheahan KL, Goldstein KM, Than CT, et al. Women Veterans’ Healthcare Needs, Utilization, and Preferences in Veterans Affairs Primary Care Settings. J Gen Intern Med. 2022;37(Suppl 3):791-798. doi:https://doi.org/10.1007/s11606-022-07585-3.
Funding
This work was undertaken as part of the US Department of Veterans Affairs, Primary Care Analytics Team. Funding was provided by the Veterans Health Administration, Office of Primary Care. Dr. Maciejewski received VA HSR&D funding (RCS 10–391, CIN 14–310).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The views expressed are those of the authors and do not represent the views of the US Department of Veterans Affairs or the US government.
Conflict of Interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations
This work was presented at the 2022 Society of General Internal Medicine annual meeting in Orlando, FL, as a poster.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rao, M., Greene, L., Nelson, K. et al. Associations Between Social Risks and Primary Care Utilization Among Medically Complex Veterans. J GEN INTERN MED 38, 3339–3347 (2023). https://doi.org/10.1007/s11606-023-08269-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08269-2