Abstract
Background
For the 5 million persons living with dementia (PLWD) in the USA, telemedicine may improve access to specialty care from their homes.
Objective
To elicit informal caregiver perceptions of tele-dementia care provided during COVID-19.
Design
Qualitative, observational study using grounded theory.
Participants
Informal caregivers aged 18 + who cared for an older adult who received tele-dementia services at two major VA healthcare systems participated in 30–60-min semi-structured telephone interviews.
Interventions
Interviews were designed using Fortney’s Access to Care model.
Main Measures
Thirty caregivers (mean age = 67, SD = 12, 87% women) were interviewed.
Key Results
Five major themes were (1) Tele-dementia care avoids routine disruption and pre-visit stress; (2) Transportation barriers to in-person visits include not only travel logistics but navigating the sequelae of dementia and comorbid medical conditions. These include cognitive, behavioral, physical, and emotional challenges such as balance issues, incontinence, and agitation in traffic; (3) Tele-dementia care saves time and money and improves access to specialists; (4) Tele-dementia facilitated communication between caregiver and provider without hindering communication between PLWD and provider; and (5) Caregivers described ideal future dementia care as a combination of virtual and in-person modalities with in-home help, financial and medical support, and dementia-sensitive caregiver access. Caregivers interviewed saved 2.6 h ± 1.5 h (range: 0.5 to 6 h) of travel time. Multiple caregivers described disruption of routines as difficult in PLWD and appreciated the limited preparation and immediate return to routine post telemedicine visit as positives.
Conclusions
Caregivers found tele-dementia care convenient, comfortable, stress reducing, timesaving, and highly satisfactory. Caregivers would prefer a combination of in-person and telemedicine visits, with an opportunity to communicate with providers privately. This intervention prioritizes care for older Veterans with dementia who have high care needs and are at higher risk for hospitalization than their same age counterparts without dementia.
Similar content being viewed by others
BACKGROUND
During the COVID-19 pandemic, family caregivers experienced higher levels of stress and burden due to increased caregiving responsibilities, heightened vigilance, and social isolation.1 These stressors were amplified by care recipients’ behavioral and psychological symptoms of dementia, respite cancellations, and cancelled appointments. Hospitalized patients were discharged home sooner to keep hospitals open for COVID-19 patients, and post-acute care options were limited.2 A recent survey of 576 family caregivers showed that caregivers reported higher anxiety, depression, fatigue, and sleep issues than non-caregivers. Caregivers who were women, younger, lower income, provided both personal and medical care, and cared for those with cognitive or behavioral problems reported worse outcomes.3
Some of these care recipients with cognitive and behavioral challenges are the estimated 5 million persons living with dementia (PLWD) in the USA. A survey of dementia caregivers in Italy early in the pandemic reported that 54.7% experienced worsening behaviors in care recipients including agitation, aggression, apathy, and depression.4 A study in Greece during the pandemic lockdown period reported increased behavioral and psychological symptoms in the PLWD and increased caregiver hyperarousal, avoidance symptoms, and COVID-19 worries.5 Some of the pandemic-related changes PLWD have experienced include difficulty complying with COVID-19 safeguarding procedures including masking, handwashing, and social distancing, further putting them at risk of contracting COVID-19.6,7,8 Compounding these challenges was the recognition that PLWD are at higher risk of hospitalization and death from complications of COVID-19.9,10,11
PLWD and their caregivers particularly need specialty care access to address behavioral and psychological symptoms of dementia and caregiver stress. Telemedicine has the potential to improve this access and reduce related stresses. Telemedicine appointment uptake increased drastically during the pandemic. Specialty tele-dementia care and caregiver perspectives are of unique interest to general internists as they are often the first line providers addressing the behavioral and psychological symptoms experienced by those with dementia and are tasked with treating or referring to subspecialty expertise, when available.
OBJECTIVE
Despite the massive shift to telemedicine, little is known about how dementia caregivers experience telemedicine visits. The objective of this qualitative study is to examine the informal caregivers’ perceptions, experiences, and satisfaction of specialty dementia care delivered through a telemedicine modality, hereafter termed “tele-dementia care,” provided during COVID-19 pandemic. Tele-dementia care was intended to provide all the elements that would take place in-person: patient and caregiver interviews, diagnosis, pharmacologic and non-pharmacologic management, and was not viewed as a temporary measure until in-person care was available.
METHODS
Study Design
This study aimed at understanding the tele-dementia care program for older Veterans enrolled at two major Veteran Affairs (VA) medical centers in California and Ohio. This qualitative, observational study used grounded theory to answer the question, “What do caregivers report about their experience with receiving dementia care and specifically tele-dementia care?” The study was deemed exempt for human subjects’ research by the relevant Institutional Review Boards (IRB#59643).
Participants
We recruited a convenience sample of 30 family caregivers of older Veterans who sought tele-dementia care between October 2020 and August 2021. The sample size of 30 was selected as data saturation is often reached within 9–17 interviews.12. Since two sites were used, 15 interviews were conducted from each site. Eligible caregivers were English-speaking and > 18 years old, had telephone access, and could provide consent. Of 58 caregivers screened, 2 caregivers were excluded whose PLWD had died; 26 caregivers failed screening attempts as they did not answer the phone or felt too stressed to participate. Study staff contacted the caregivers, described the study, and obtained verbal informed consent. Some caregivers in this study used Veteran Affairs (VA)–provided tablets to receive tele-dementia care, while others used personal devices.
Survey and Interview
Caregivers participated in 30–60-min, telephone-based, semi-structured interviews between July 2021 and March 2022. The two interviewers (VN, MB) were trained qualitative researchers with experience interviewing informal caregivers in clinical settings. Audio recordings were transcribed for analysis.
The interview guide (Supplemental Appendix 1) was informed by Fortney’s Access to Care model13 and included questions related to domains of access to care (geographical, temporal, and digital factors) as well as perceived access to care, utilization, satisfaction, and quality. The interview guide began with caregiver background questions, the home caregiving situation, caregiver’s estimate of travel time to the main medical center, and PLWD’s assistance needs. The guide elicited dementia care medical history and access to care and utilization and probed to elicit thorough, detailed descriptions of caregivers’ experiences with Veterans’ dementia specialty care. Caregivers were asked to describe the Veteran’s experiences seeking care and treatment within and outside of the VA for dementia specialty care, as well as their experiences receiving care in-person versus via telemedicine. Caregivers were asked about time savings, ideal dementia care, and satisfaction with tele-dementia care on a 10-point scale. Caregivers were asked about post-pandemic care and the first 3 words that describe tele-dementia care. Caregivers were asked some optional, general demographic questions about their race, education, marital status, and financial situation. Financial situation was asked in the following manner: “Without telling us the exact amount, how would you describe your financial situation? I’m going to give you 5 options.” Age, stage of dementia of the Veteran, and one way distance to VA medical center were abstracted from the medical record.
Data Analysis
Descriptive statistics was used to summarize participant demographics. Qualitative analysis using a grounded theory approach was conducted by two coders (VN, MBH) and overseen by two research advisors (SI, RT). Guided by a post-positivist interpretive framework14, we focused our study on describing the caregiver experience using tele-dementia services. The four authors (SI, VN, MBH, RT) met weekly for 2 h over 5 months to discuss data collection and emergent patterns and theory. A codebook was developed by initially open coding15 the first five transcripts, and then meeting with the co-investigators to establish consensus with coding and resolve inconsistency. The coding and analysis continued with a constant comparative approach16. Once all the manuscripts were coded, axial coding15 was conducted to establish relationships between the codes. At weekly meetings, transcripts were reviewed and compared against emergent theory. Data were collected and analyzed until no new components of the theory arose from the new interviews. Saturation, therefore, was sought when there were no fundamental differences in the content of interviews.
The importance of the iterative review and discussion of transcripts, codes, and memos allowed the team to recognize emerging themes. Thematic analysis was conducted using both inductive and deductive generated coding, whereby the process was guided by Braun and Clarke17 that included familiarization with the data, generation of initial coding, noting emerging themes, reviewing themes, defining and naming the themes, achieving thematic saturation, and reporting findings. Through constant review of the data, quote comparison, code frequency assessment, memo writing, and relationship evaluation of coded segments against emerging themes, the team was able to build themes grounded in data. Feedback was gathered when the themes were presented to the broader group of co-investigators. All inconsistencies between the analysts were resolved over discussion with the co-investigators in the research meetings. ATLAS.ti version 9 software was used.18
RESULTS
Thirty caregivers (mean age = 67 y ± 11.6, 87% women) were interviewed. Mean distance from the VA medical center was 53.4 miles (SD = 34.4). All caregivers (100%) reported helping PLWD with instrumental activities of daily living (IADL) and 67% reported helping PLWD with at least one activity of daily living (ADL). Table 1 describes the characteristics of the study participants. Caregivers’ experiences were similar when discussing dementia care regardless of geographical area. The top three words to describe their tele-dementia experience were helpful, easy, and convenient and can be seen in Fig. 1.
Five primary themes related to the caregiver’s experiences with obtaining dementia specialty care were derived. Results are presented below and include selected representative quotations. The section headings below the themes are subthemes.
Theme 1: Tele-dementia Care Avoids Routine Disruption and Pre-visit Stress
Limited Preparation for Visits and Immediate Return to Routine
Multiple caregivers described how they appreciated the limited preparation needed for a tele-dementia visit, including immediate return to routine post visit completion (Table 2, 1.1).
Pre-visit Stress Experienced by Caregivers and PLWD
In the absence of tele-dementia care, caregivers described needing many hours for visit preparation since the PLWD may not want to get ready and leave the home according to the planned schedule, or may have stress around changes in routine when they cannot control the activities of the day (Table 2, 1.2, 1.3, 1.4). A caregiver stated “it makes him decline actually… I wouldn’t even tell him up to the minute we were leaving because he would be so anxious” (Table 2, 1.5).
Even When Technical Issues Are Present, an Alternative to In-person Care Is Beneficial
Caregivers noted occasional technical issues that some participants faced (e.g., internet connection, speed of internet, grainy quality of the video). Despite this, participants interviewed still felt an alternative to in-person visits was beneficial (Table 2, 1.6).
Theme 2: Transportation Barriers to In-person Visits Include Not Only Travel Logistics, But Navigating the Sequelae of PLWD’s Dementia and Other Comorbid Medical Conditions
Caregivers described that transportation included exiting the house, entering the car safely, driving to the facility, parking, exiting the car, and walking to the building and into the clinic.
Cognitive Barriers to Transportation: Attention and Executive Function Challenges
Many caregivers described their PLWD as having an inability to follow instructions. Caregivers described opening their front door and having the person with dementia elope or refuse to get in the car. They also described behaviors such as locking and unlocking doors (Table 2, 2.1).
Perceptual Disturbances—Hallucinations
Multiple caregivers described auditory and visual hallucinations and delusions present in the PLWD that made staying home and leaving difficult (Table 2. 2.2).
Physical Challenges
Multiple caregivers noted that their PLWD encountered numerous physical challenges including loss of balance, incontinence, hearing and vision loss that made exiting the house and entering the car difficult when trying to access in-person care (Table 2, 2.3).
Emotional, Cognitive, and Physical Challenges Together
One caregiver stated her husband had “…nervousness issues, where he ends up having bowel movements” (Table 2, 2.4). Additionally, several caregivers described their PLWD’s fear and stress in traffic created potentially dangerous driving situations. When in the car, many caregivers experienced stress as some PLWD demonstrated unsafe passenger behaviors that were distracting “he would get so scared in the traffic, I don’t know how I could drive and keep him calm” (Table 2, 2.5). Another confessed she felt “I’m going to have a wreck, just because you’re scaring me!” (Table 2, 2.6). One caregiver takes a bus after PLWD had license suspended so “I don’t have to deal with his arguing and trying to tell me what to do.” (Table 2, 2.7).
Navigating Parking and Walking from Car to Clinic with PLWD Is Challenging
When caregivers arrived at the medical center, they could not leave their PLWD unattended, but also struggled physically with getting them from the parking spot to the facility. One caregiver described “Drop him off, get him in, get him sat down, and then I go back to the car, go across the street with my vehicle, park in the parking lot, come flying back across as fast as I can” (Table 2, 2.8).
Theme 3: Tele-dementia Care Saves Time and Money and Improves Access to Specialists
When asked how much time saved, answers varied widely. Caregivers reported they saved 2.6 h ± 1.5 h (range: 0.5 to 6 h) of travel time.
Avoiding Travel Saves Money
Caregivers reported that avoiding travel-related costs like gas saves money, and the hassle of filing for travel reimbursement (Table 2, 3.1).
Accessing Dementia Specialty Care Is Hard and Older Adults Can Benefit from Specialized Medical Professionals
One caregiver described difficulty finding Lewy body dementia specialists in her geographical area, “We have nobody in our area… We don’t even have a nursing home or memory care.” (Table 2, 3.2). Another caregiver appreciated the geriatrics specialty care for dementia “Senior citizens have special needs and things that are happening to them just because of their age, and they need a doctor that specializes in that area.” (Table 2, 3.3).
Avoiding COVID Exposure
A few caregivers appreciated the avoidance of COVID-19 exposure “He doesn’t understand the COVID procedures…he’s had his shot and he wears a mask, so his main problem is the hands and getting too close to others.” (Table 2, 3.4).
Theme 4: Tele-dementia Facilitated Communication Between Caregiver and Provider Without Hindering Communication Between PLWD and Provider
Even Though Caregivers Like In-person Visits, It Is Easier for Both PLWD and Caregivers to be Heard During Tele-dementia Visits
One caregiver described “the one advantage to doing it on video is that if I can get him to leave the room, then I can actually talk without the interruptions…” (Table 2, 4.1).
“Truth” Telling Is Different for the PLWD and the Caregiver
“Truth” telling seemed to refer to the accuracy of information given by the PLWD to the care provider. For example, the PLWD may mis-remember and report inaccurate information about current state (Table 2, 4.2). Another caregiver expressed appreciation to talk to the provider before or after scheduled visits (Table 2, 4.3).
In-person Communication Is Challenging for PLWD When Providers Are Masking
In the COVID-19 era, masks and face-shields are necessary safeguarding for healthcare professionals, but this too can be problematic for some patients, especially those with sensory impairments like hearing. Although tele-dementia can also be challenging for those with hearing impairment, at times providers may be able to speak over video or telephone without a mask on “It’s difficult to understand anybody with a mask on.” (Table 2, 4.4).
Theme 5: Caregivers Described Ideal Future Dementia Care as a Combination of Virtual and In-Person Modalities with In-home Help, Financial and Medical Support, and Dementia-Sensitive Caregiver Access
Caregivers Hope to Use Tele-dementia Services Beyond the Pandemic
Caregivers hope to continue using tele-dementia services beyond the pandemic due to the convenience, especially as the disease advances and getting out of the home becomes increasingly difficult. However, they did not want to eliminate in-person visits completely “I’d take a mixture.” (Table 2, 5.1).
Caregivers Feel Calmer and with Less Stress During Tele-dementia Visits
One caregiver reflected upon the way she shows up to tele-dementia visits versus in-person visits. “I kind of tend to think that I’m more calm virtually.” (Table 2, 5.2).
Caregivers Described What an Ideal Future State of Dementia Care Would Be Like, Both for Their PLWD and for Caregivers
Caregivers discussed how they had dreamt about this and provided comments about an ideal future state. “In the ideal world? More caring.” (Table 2, 5.3). They also described respite care coming “at least every other day” (Table 2, 5.4) and wishing there was a “handyman type of home health aide, that wouldn’t mind being outside with him, like raking leaves or shoveling snow” (Table 2, 5.5). They also described hope for financial assistance for “middle class” caregivers “Because a lot of us don’t want to put our loved one in a home and don’t want to have to give up everything to do that.” (Table 2, 5.6).
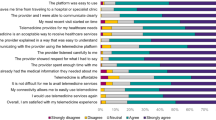
Words Describing Caregivers’ Tele-dementia Experiences
Satisfaction with the tele-dementia services at the VA was expressed (m = 8.6; SD = 1.9) on the 1 to 10 scale. A word cloud was generated from caregiver responses regarding how they would describe their experience. The more frequently a word was used by the caregivers interviewed, the larger the word’s size was in the corresponding graphic (Fig. 1).
Our findings are illustrated in Fig. 2.
DISCUSSION
The key findings of this study are that tele-dementia care has the potential to alleviate not only the logistical and transportation challenges experienced by caregivers when trying to receive in-person dementia care, but also behavioral and COVID-19-related challenges. PLWD were able to receive specialty dementia care in their homes through this program and the dyad of caregiver and PLWD were able to communicate effectively with providers. Caregivers found tele-dementia care to be convenient, effective, stress reducing, safe, satisfactory, time saving, and highly valued.
Prior tele-dementia studies largely characterize barriers and facilitators to engaging in tele-health,19 or focus on the physician experience.20 Care models involving telehealth and dementia care differed in that they utilized care navigators and nurses to provide support21 or used asynchronous telehealth for non-pharmacologic support for dementia behaviors.22 Transportation studies have mainly reported on the loss of driving in those diagnosed with dementia23 or use of transportation assistance.24 As one of the first studies to explore the challenging layers that dementia caregivers face when trying to obtain specialty dementia care, we add to the research by describing the processes that compromise transporting a PLWD from the home to the clinic.
Caregivers detailed the sequential pre-visit tasks that need to be completed by the PLWD to be transported. Despite vehicle availability, a confluence of other factors must align. The PLWD must follow directions, and not have any behavioral issues that preclude safely entering or sitting in a car. The appropriate time, patience, physical assistance, and cueing may be needed to get the PLWD ready for the appointment. In cases where these factors do not align, such as if distress behaviors preclude safely entering the vehicle, the PLWD would be unable to safely get to in-person appointments on time. When dealing with PLWD, services providing transportation assistance are necessary, but not sufficient to meet the needs of this population. Additionally, the cost savings of tele-dementia care noted by caregivers also predates a period of high gas prices, so the monetary relief could be even more pronounced in periods of higher gas price fluctuations. From the caregiver perspective, tele-dementia care overcame all these transportation and logistics–related challenges because the visit was integrated into the daily routine with minimal disruption. Tele-dementia care avoids amplifying behavioral challenges that are often present from changing environmental triggers. Some of these avoidance advantages are due to the virtual modality in general, but others are specific to tele-dementia care.
Communication was a second notable area from our study. The caregiver’s remarks about PLWD having difficulty understanding providers with masks raise an important consideration about whether in-person communication with masks and face shields is clearer than tele-health communication. Additionally, the ability for both the dyad of dementia caregiver and PLWD to be heard by medical providers during visits is very important for future dementia healthcare design. The discrepancies we uncovered in “truth” telling between the caregivers and PLWD are common and may be attributed to “anosognosia,” or an impaired awareness of the deficits associated with dementia.25 Additionally, when behavioral and psychological symptoms of dementia are present, the caregiver would benefit from direct discussion with the provider on management strategies.
The implications of asking caregivers to describe both their own experiences and Veterans’ experiences with seeking dementia care and treatment are to understand the real problems Veterans face. Family caregivers, who experience daily life alongside individuals with dementia, provide valuable insight into the lived experience of those with dementia and family caregivers. We recognize this is a limitation; however, informant reporting is used frequently in dementia care.
This study has several limitations that may influence the interpretation and transferability of results. Our sample was based on a convenience sample of caregivers identified by physicians which may have led to selection and inclusion bias. Also, our sample was largely homogenous in gender, race, spousal relationship, and cohabitant status and only included caregivers of Veterans with medical care at the Veterans Health Administration (VHA), which may affect the variability of experiences that were captured. The experience of Veterans may not be generalizable outside of the VA given that all participants had access to services, medications, and supplies provided by the VHA. This was a pilot program evaluation and was conducted while also rapidly disseminating this clinical care in the context of notable healthcare changes during COVID-19 pandemic including clinic closures and emergency protocols, so providers could not specifically train in tele-dementia care. It remains to be seen if the program remains equally acceptable when in-person care becomes more available. Despite these limitations, the caregivers’ level of acceptability of tele-dementia care even with technical difficulties suggests that this is a way to deliver high-quality care ongoing as the pandemic waxes and wanes.
Strengths of this study include the design, attainment of rich qualitative data, timeliness and relevance of the results. Although spousal caregivers are the majority of caregivers represented here, 30% of caregivers are other relatives. Caregiver demographics of primarily women are consistent with national statistics that two thirds of dementia caregivers are women nationally.26
Systems level challenges do exist that make enacting tele-dementia care difficult. Policy supporting telemedicine is currently largely under emergency use authorization from the COVID-19 pandemic and varies by state. We recommend that policymakers continue considering the role of tele-medicine in caring for older adults and support tele-dementia care as a reimbursable care model beyond the pandemic. By continuing to utilize telemedicine, access to hard-to-reach specialty care can improve. Caregivers are often left out as members of the care-recipient’s health care team27 and standards for incorporating caregivers into outpatient settings are nonexistent. Visitation restrictions applied institutionally during the pandemic negatively affected caregivers and PLWD.28,29 As we recognize the difficulty for health systems to engage caregivers, we point out the value in developing business cases for consistently incorporating caregivers into care and capturing this benefit.27 Additionally, we recommend that if dementia caregivers need to cancel in-person appointments due to a variety of factors, attempting tele-dementia care, instead of rescheduling appointments, can be beneficial to all parties. Recognizing and addressing the unique challenges of transporting PLWD must be a priority for healthcare systems. At a family level, having appointment offerings that miss high traffic hours could also be helpful for those with dementia as multiple caregivers described how sitting in traffic negatively impacts a PLWD’s mood and behaviors, to the point of putting them in dangerous driving situations. Additional transportation assistance from parking lots to clinics would help many caregivers and care recipients.
CONCLUSIONS
Caregivers found tele-dementia care to be convenient, effective, stress reducing, safe, satisfactory, and time saving, and see this care modality as a part of ideal future state dementia care. Tele-dementia services prioritize care for older Veterans with dementia who have high care needs and are at higher risk for hospitalization. This care complements in-home support services to help older adults with dementia age in place. It can also leverage access to specialty care and can be scalable beyond a healthcare system level to a regional or national level. Tele-dementia care is also consistent with and contributes to “age-friendly” care.30 Future directions may include measuring program effectiveness and ability to prevent emergency room visits or delay institutional care, and looking into differences in caregiver responses based on education and occupation. However, this need for additional evaluation is balanced with the real-world need to care for an increasing number of older adults with dementia, complex psychosocial needs and multiple medical conditions, and a declining geriatrics subspecialist workforce.31,32 Our study illustrates that caregivers welcome tele-dementia specialty care, not simply as a temporary measure to mitigate the risk of the pandemic, but also as a permanent feature of specialty dementia care to mitigate safety and stress of managing PLWD.
References
Masoud S, Glassner AA, Mendoza M, Rhodes S, White CL. “A different way to survive”: the experiences of family caregivers of persons living with dementia during the COVID-19 pandemic. J Fam Nurs. 2022. 10748407221111079.
Dang S, Penney LS, Trivedi R, Noel PH, Pugh MJ, Finley E … & Leykum L. Caring for caregivers during COVID‐19. J Am Geriatr Soc. 2020;68(10):2197.
Beach SR, Schulz R, Donovan H, Rosland AM. Family caregiving during the COVID-19 pandemic. Gerontologist. 2021;61(5):650-660.
Canevelli M, Valletta M, Blasi MT, Remoli G, Sarti G, Nuti F … & Bruno G. Facing dementia during the COVID‐19 outbreak. J Am Geriatr Soc. 2020.
Alexopoulos P, Soldatos R, Kontogianni E, Frouda M, Skondra M, Passa M … & Politis A. COVID-19 crisis effects on caregiver distress in neurocognitive disorder. J Alzheimer’s Dis. 2021;79(1):459–466.
Wong R, Lovier MA. Relationship between dementia, COVID‐19 risk, and adherence to COVID‐19 mitigation behaviors among older adults in the United States. Int J Geriatr Psychiatry. 2022.
Korczyn AD. Dementia in the COVID‐19 period. J Alzheimers Dis. 2020;75(4):1071‐1072. https://doi.org/10.3233/JAD‐200609
Toniolo S, Scarioni M, Di Lorenzo F, et al. Dementia and COVID‐19, a bidirectional liaison: risk factors, biomarkers, and optimal health care. J Alzheimers Dis. 2021;82(3):883‐898. https://doi.org/10.3233/JAD‐210335
Wang H, Li T, Barbarino P, et al. Dementia care during COVID‐19. Lancet. 2020;395:1190‐11911. https://doi.org/10.1016/S0140-6736(20)30755-8.
Wang Q, Davis PB, Gurney ME, Xu R. COVID‐19 and dementia: analyses of risk, disparity, and outcomes from electronic health records in the US. Alzheimers Dement. 2021;17(8):1297‐1306.
COVID-19 guidance for older adults. Center for Disease Control and Prevention. https://www.cdc.gov/aging/covid19-guidance.html. Published January 8, 2021. Accessed January 25, 2021.
Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. 2022;292:114523.
Fortney JC, Burgess JF Jr, Bosworth HB, Booth BM, Kaboli PJ. A re-conceptualization of access for 21st century healthcare. J Gen Intern Med. 2011;26(suppl 2):639–647.
Guest G, Namey EE, Mitchell ML. Collecting qualitative data: a field manual for applied research. London, UK: Sage Publications 2013. https://doi.org/10.4135/9781506374680.
Saldana J. The coding manual for qualitative researchers (3rd ed.), Sage Publications Ltd, Thousand Oaks, California 2016.
Creswell J, Poth CN. Qualitative inquiry and research design: choosing among five approaches (4th ed.), Sage, Los Angeles 2018.
Braun V, Clarke V. Thematic analysis revised. Qual Res Psychol. 2006;3(2):77-101.
ATLAS.ti 9.0 Download (Free trial) - Atlasti.exe (informer.com); Lewins, Ann & Silver, Christina (2007). Using software in qualitative research: A step-by-step guide. London: Sage
Moo LR, Gately ME, Jafri Z, et al. Home-based video telemedicine for dementia management. Clin Gerontol. 2020;43(2):193-203. https://doi.org/10.1080/07317115.2019.1655510
Banerjee D, Vajawat B, Varshney P, Rao TS. Perceptions, experiences, and challenges of physicians involved in dementia care during the COVID-19 Lockdown in India: a qualitative study. Front Psychiatry. 2021;11:615758.
Possin KL, Merrilees JJ, Dulaney S, Bonasera SJ, Chiong W, Lee K … & Miller BL. Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the care ecosystem randomized clinical trial. JAMA Int Med. 2019;179(12):1658–1667.
Williams K, Blyler D, Vidoni ED, Shaw C, Wurth J, Seabold D … & Van Sciver A. A randomized trial using telehealth technology to link caregivers with dementia care experts for in‐home caregiving support: FamTechCare protocol. Res Nurs Health. 2018;41(3):219–227.
Connors MH, Ames D, Woodward M, Brodaty H. Predictors of driving cessation in dementia. Alzheimer Dis Assoc Disord. 2018;32(1):57-61.
Weber SR, Pirraglia PA, Kunik ME. Use of services by community-dwelling patients with dementia: a systematic review. Am J Alzheimer's Dis Other Dementias®. 2011;26(3):195-204.
de Ruijter NS, Schoonbrood AM, van Twillert B, Hoff EI. Anosognosia in dementia: a review of current assessment instruments. Alzheimer’s Dement Diagn Assess Dis Monit. 2020;12(1):e12079.
Alzheimer’s Association. 2022 Alzheimer’s disease facts and figures.Alzheimers Dement. 2022;18.
National Alliance for Caregiving. Caring for the caregiver: Incentivizing medical providers to include caregivers as part of the treatment team [White paper]. https://www.caregiving.org/wp-content/uploads/2021/12/NAC_CaringForCaregiver_Paper_121221.pdf; 2021. Accessed November 9, 2022.
Migliaccio R, Bouzigues A. Dementia and COVID-19 lockdown: more than a double blow for patients and caregivers. J Alzheimer's Dis Rep. 2020;4(1):231-235.
Nash WA, Harris LM, Heller KE, Mitchell BD. “We are saving their bodies and destroying their souls.”: family caregivers’ experiences of formal care setting visitation restrictions during the COVID-19 pandemic. J Aging Soc Policy. 2021;33(4-5):398-413.
Fulmer T, Mate KS, Berman A. The age‐friendly health system imperative. J Am Geriatr Soc. 2018;66(1):22-24.
Juul D, Colenda CC, Lyness JM, Dunn LB, Hargrave R, Faulkner LR. Subspecialty training and certification in geriatric psychiatry: a 25-year overview. Am J Geriatr Psychiatry. 2017;25(5):445-453.
Lester PE, Dharmarajan TS, Weinstein E. The looming geriatrician shortage: ramifications and solutions. J Aging Health. 2020;32(9):1052-1062.
Acknowledgements
The authors would like to thank members of the Geriatrics Research Education and Clinical Centers in Palo Alto and Cleveland for their support for the clinical care that informed this work including Dat Hoang-Gia, J. Lisa Tenover, Kristal Samson, and Alyssa Peters, as well as Jennifer S. Smith.
Funding
Funding support from Mission Act, VA Office of Academic Affiliation, Geriatric Research, Education, and Clinical Center, GRECC Connect, a promising Office of Rural Health Practice, Elizabeth Dole Center of Excellence for Veteran and Caregiver Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Access research domains: equity/subpopulations, and effective interventions.
Prior presentations: Gerontological Society of America 2022 poster.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Iyer, S.S., Ngo, V., Humber, M.B. et al. Caregiver Experience of Tele-dementia Care for Older Veterans. J GEN INTERN MED 38, 2960–2969 (2023). https://doi.org/10.1007/s11606-023-08188-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08188-2