Abstract
Background
The reduction of physical restraint utilization in the hospital setting is a key goal of high-quality care, but little is known about the rate of restraint use in general hospitals in the USA.
Objective
This study reports the rate of physical restraint coding among acute care hospital discharges in the USA and explores associated demographic and diagnostic factors.
Design
The National Inpatient Sample, a de-identified all-payors database of acute care hospital discharges in the USA, was queried for patients aged 18 and older with a diagnosis code for physical restraint status in 2019.
Participants
Hospitalized patients aged 18 and older.
Main Measures
Demographics, discharge diagnoses, in-hospital mortality, length of stay, total hospital charges.
Key Results
In total, 220,470 (95% CI: 208,114 to 232,826) hospitalizations, or 0.7% of overall hospitalizations, included a discharge code for physical restraint status. There was a 700-fold difference in coding for restraint utilization based on diagnosis, with 7.4% of patients with encephalitis receiving restraint diagnosis codes compared to < 0.01% of patients with uncomplicated diabetes. In an adjusted model, male sex was associated with an odds ratio of 1.4 (95% CI: 1.4 to 1.5) for restraint utilization coding, and Black race was associated with an odds ratio of 1.3 (95% CI: 1.2 to 1.4) relative to white race.
Conclusions
In the general hospital setting, there is variability in physical restraint coding by sex, race, and clinical diagnosis. More research is needed into the appropriate utilization of restraints in the hospital setting and possible inequities in restraint utilization.
Similar content being viewed by others
INTRODUCTION
A physical restraint is defined as “any action or procedure that prevents a person’s free body movement to a position of choice and/or normal access to his/her body by the use of any method, attached or adjacent to a person’s body that he/she cannot control or remove easily.”1 In the hospital setting, physical restraint can take many forms, including raised bed rails, limb restraints, hand mitts, and vests. The use of restraint has been justified as preventing greater harm to patients or medical staff,2 although some authors argue that restraint use is rarely, if ever, justified,3 and should be considered evidence of treatment failure.4 Physical restraints are associated with medical complications including skin breakdown, thrombosis, rhabdomyolysis, aspiration, positional asphyxia, and death,5 although precise rates of these complications are unclear, and are likely confounded by the underlying medical condition for which restraints were applied. Additionally, restraint is associated with psychological distress among patients,6 and may be associated with subsequent trauma syndromes.7 The effectiveness of physical restraints at reducing patient injuries is unclear, and is further confounded by severity of illness. For instance, one systematic review found that physical restraint utilization was not associated with changes in fall rates among older adults,8 and studies have indicated that patients who are physically restrained have higher rates of unplanned extubation in the intensive care unit (ICU), although these analyses could not control for the fact that patients may have been restrained precisely because the treating teams considered them to be at high risk of extubation.9,10
National guidelines from the Joint Commission have emphasized reduced use of restraints, and mandated restraint rate reporting in psychiatric hospitals.11 The rate of restraint usage varies widely among countries and medical settings. For example, studies have documented physical restraint use in 4.8% of general hospital patients in Switzerland and Austria,12 1.7% in psychiatric hospitals in Norway,13 23% in a tertiary care hospital in South Africa (with wide variation of 0 to 54.5% depending on inpatient unit),14 3.4% in Malaysian hospitals,15 61.2% in Chinese ICUs,16 and 50.1% of geriatric patients in Japanese hospitals during the COVID-19 pandemic.17 Moreover, there is substantial variability in restraint utilization even within the same region and health care setting, with one cross-sectional study of European ICUs finding the prevalence of physical restraint to vary between 0 and 100% depending on individual unit18; thus, pooling rates may mask important underlying variability.
Numerous studies have explored care programs for reducing physical restraint utilization,19,20 and improved understanding of restraint utilization in hospitals could help target evidenced-based interventions toward patients at highest risk of receiving physical restraints and guide subsequent quality improvement efforts. This study characterizes the occurrence of administrative claims diagnosis of physical restraint using nationally representative data to characterized encounters which included recorded use of restraints.
METHODS
Data Source
To assess nationwide occurrence of in-hospital physical restraints, this analysis utilized the 2019 edition of the National Inpatient Sample (NIS), from the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The NIS is a claims database including demographic information, discharge diagnoses (up to 40), and inpatient procedures (up to 25) drawn from 4568 acute care hospitals in 49 states covering 98% of the US population. The NIS is designed to provide nationally representative estimates of hospital discharges using a stratified sampling of 20% of overall discharges. Data are provided for hospitalizations in a de-identified format, with no mechanism for linking database entries to identified individuals. Of note, the NIS samples general hospitals only, and thus, estimates do not include facilities such as rehabilitation hospitals, freestanding psychiatric hospitals, or federally operated facilities. As this is a de-identified, publicly available database, this study was determined to be Not Human Subjects Research by the Mass General Brigham Institutional Review Board.
Data Selection
Hospitalizations involving physical restraint coding were identified using International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code Z78.1 “physical restraint status.” Discharges were included in this analysis for patients aged 18 or older if Z78.1 was included among the discharge diagnosis codes. Primary diagnoses of hospitalizations involving physical restraint were classified into diagnostic categories using the Clinical Classifications Software Refined (CCSR) (v2021.2. Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, Rockville, MD), which groups ICD-10-CM codes into clinically relevant categories. Patients who received mechanical ventilation were identified based on ICD-10 procedural codes 5A1935Z, 5A1945Z, and 5A1955Z. All data are presented as reported in the NIS.
Statistical Analysis
All analyses were conducted on data weighted according to the appropriate NIS discharge weight to obtain nationwide estimates. The survey design of the NIS, in which individual hospitals are clustered within strata (based on geographic region, hospital ownership, teaching status, and bed size) and then discharges sampled at 20% without replacement within strata, produces variance around all reported continuous and categorical variables. This variance is used to present sample uncertainty for the total number of discharges with a physical restraint code, whereas weighted point estimates are reported for all other analyses. Due to the non-normal distribution of age, length of stay, and total hospital charges, these values are reported as medians with interquartile range (IQR). All tests were two-sided, with an α level of 5% for all outcomes, without correction for multiple comparisons.
For the primary statistical analysis, a logistic regression was performed on the binary outcome of a hospitalization including vs. not including a billing code for physical restraint status. This logistic regression incorporates the sampling methodology of the NIS, so it explicitly considers the NIS stratum and hospital identifier as part of variance calculations. In this model, age (z score), sex, race, admission type (elective vs. non-elective), hospital bed size (small/medium/large), primary service line, region, income quartile of the patient’s ZIP code, and patient severity (defined based off of All Patient Refined-Diagnosis Related Groups’ (APR-DRGs) Severity of Illness)21,22 are descriptor variables. As a sensitivity analysis, this analysis was repeated separately for patients with a procedure code for mechanical ventilation during hospitalization. In a model of cost, the log-transformed total hospital charges were modeled using a general linear model (GLM) incorporating the sampling methodology of the NIS, with physical restraint code (yes or no), age (z score), sex, hospital region, hospital bed size (small/medium/large), admission type (elective vs. non-elective), primary service line, whether the admission involved a major operative procedure, primary payor, the log-transformed sum of total length of stay plus 1, and APR-DRGs Severity Of Illness as descriptor variables. All analyses were conducted using SPSS (version 29; IBM Software, Inc., Armonk, NY). This study is reported in accordance with the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement.23
RESULTS
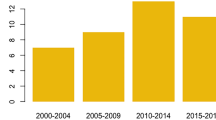
Among the 30,218,268 hospitalizations for patients aged 18 and older in the USA in the 2019 NIS, 220,470 (95% CI: 208,114 to 232,826) included a discharge diagnosis code for physical restraint status, for an overall restraint coding rate of 0.7%. Demographically, 42.9% of overall hospitalizations were for male patients, but 61.9% of coded restraints involved male patients. The proportion of hospitalizations involving a diagnosis code for physical restraint varied between 0.5 and 0.9% depending on the age of the patient, with peaks for those aged 18–20, 46–55, and 81–90 + years old (Fig. 1). Full demographic information for hospitalizations involving and not involving restraint coding are listed in Table 1.
Percentage of overall hospitalizations that involve a diagnosis of physical restraint status vs. the age of the patient. While the absolute number of hospitalizations and restraints varies by age, the proportion of hospitalizations with a restraint diagnosis is within the range of 0.5 to 0.9% for all ages.
In a GLM model of the log-transformed total hospital charge, adjusting for physical restraint code (yes or no), age (z score), sex, hospital region, hospital bed size (small/medium/large), admission type (elective vs. non-elective), primary service line, whether the admission involved a major operative procedure, primary payor, the log-transformed sum of total length of stay plus 1, and APR-DRGs Severity Of Illness, a physical restraint code was associated with an increased hospital charge of $5,445 per hospitalization, or an aggregate adjusted cost of $1.2 billion in 2019 (Table S1).
Hospitalizations with a coded restraint diagnosis included a wide variety of principal discharge diagnoses. Table 2 lists the most common CCSR categories diagnosed for hospitalizations involving restraint, while the raw ICD-10 codes are listed in Table S2. The most common diagnostic categories for hospitalizations involving restraint were septicemia (30,325 hospitalizations; 13.8% of coded restraints), schizophrenia spectrum and other psychotic disorders (11,985 hospitalizations; 5.4% of coded restraints), poisoning by drug (11,790 hospitalizations; 5.3% of coded restraints), respiratory failure (11,580 hospitalizations; 5.3% of coded restraints), and alcohol-related disorders (10,125 hospitalizations; 4.6% of coded restraints).
The overall rate of physical restraint coding differed based on the primary discharge diagnostic category (Table 3; Table S3). While overall 0.7% of hospitalizations involved physical restraint coding, when examining CCSR categories diagnosed at least 5000 times in 2019, 7.4% of the 5010 hospitalizations with a principal discharge diagnosis of encephalitis utilized a physical restraint code, the highest proportion of any diagnostic category. In contrast, < 0.01% of hospitalizations for diabetes mellitus without complication or uncomplicated pregnancy, the two categories with the lowest restraint rate, involved a code for physical restraints.
In order to explore factors associated with physical restraint coding, a logistic regression was performed on the binary outcome of a hospitalization including a diagnosis code for physical restraint (yes/no), adjusting for age (z score), sex, race, admission type (elective vs. non-elective), hospital bed size (small/medium/large), primary service line, region, income quartile of the patient’s ZIP code, and patient severity (Table 4). In this model, male sex (aOR 1.4; 95% CI: 1.4 to 1.5); Black (aOR 1.3; 95% CI: 1.2 to 1.4), Asian or Pacific Islander (aOR 1.2; 95% CI: 1.0 to 1.3), and Other (aOR 1.2; 95% CI: 1.1 to 1.4) races; non-elective admission (aOR 1.7; 95% CI: 1.6 to 1.8); mental health/substance abuse (aOR 6.5; 95% CI: 6.1 to 6.8), injury (aOR 2.8; 95% CI: 2.6 to 2.9), or surgical primary diagnosis (aOR 1.3; 95% CI 1.2 to 1.3); hospital region; and increasing disease severity (aOR 3.0; 95% CI: 3.0 to 3.1) were all associated with a higher odds of physical restraint coding. Increasing age (aOR 0.9; 95% CI: 0.9 to 0.9), small hospital size (aOR 0.8; 95% CI: 0.7 to 0.9), maternal and neonatal service line (aOR 0.1; 95% CI: 0.1 to 0.1), and second quartile of income ZIP code (aOR 0.9; 95% CI: 0.8 to 1.0) were associated with lower odds of physical restraint coding. In a sensitivity analysis of patients receiving mechanical ventilation during hospitalization, male sex, Black or Other race, non-elective admission, mental health or substance abuse, or injury primary diagnosis remained positively associated with higher odds of physical restraint coding (Table S4).
DISCUSSION
Among adult hospitalizations in general hospitals in the USA in 2019, 220,470 (95% CI: 208,114 to 232,826), or 0.7%, included a discharge diagnosis code for physical restraint status. Physical restraints were coded for patients with a range of primary diagnoses, including systemic medical illness, poisoning, psychiatric illness, substance use disorders, and neurologic illness. In an adjusted model, restraint coding was associated with an increased hospital charge of $5445 per hospitalization, or an aggregate adjusted cost of $1.2 billion.
The reduction of the use of physical restraints has been a target for quality improvement interventions, and has led to interdisciplinary quality improvement efforts.24 A 2020 scoping review found 31 studies targeting restraint reduction, with most involving multicomponent interventions.19 There were few common elements among these interventions, and limited evaluation of the effectiveness of these techniques. Some evidence suggests that front line staff can experience benefits from interventions focused on behavior management25; however, additional research is needed to develop and identify maximally effective behavior management strategies toward the goal of a safe environment of care which is not dependent on restraints.
The results of this study indicate that coding of physical restraint use occurs at different rates across clinical conditions, with a more than 700-fold variation in coding of restraint usage between patients diagnosed with encephalitis and those diagnosed with uncomplicated diabetes, the conditions with the highest and lowest restraint utilization in this sample. Overall, the conditions with the highest fractional utilization of restraint coding involve illnesses associated with neurologic impairment, including encephalitis, poisoning, stroke, traumatic brain injury, and neurocognitive disorders. While the NIS does not include the primary indication for restraint status, prior literature has implicated encephalopathy/delirium26,27 and dementia28,29 in agitation with high risk to caregivers, which may explain the utilization of physical restraints in these patients. As evidence suggests limitations in the use of coded data for identification of both dementia and delirium, interpretation of this association is limited30,31,32,33; nevertheless, given the specific morbidity of these groups, further research is on optimal use of restraints in service of health outcomes.
Demographic factors were associated with the use of physical restraints as a discharge diagnosis. These include male sex, which is consistent with prior literature finding higher rates of physical restraint in males.34,35 Likewise, non-elective admissions were more likely to involve restraint than elective admission, which may be explained by different diagnoses and comorbidities among elective and non-elective hospitalizations. Notably, there was a significant association between race and physical restraint as a discharge diagnosis, with Black, Asian or Pacific Islander, and Other race categories with higher odds of restraint than white patients. This result remained significant even controlling for primary diagnosis and disease severity, and in a sensitivity analysis looking only at patients who received mechanical ventilation, who are expected to be among the most seriously ill. Similar disparities in restraint utilization have been identified in the emergency department setting.36,37 For this study, race was reported by the treating hospital and no information is available on the procedure used to ascertain race at the various participating hospitals; this is significant as race defined in this way may differ from self-identified race, and may have important impacts on differences in healthcare outcomes.38 Nonetheless, the association warrants further focused investigation.
The results of this observational study based on routinely collected data must be considered in view of its inherent strengths and limitations. The strength of the study is the use of nationally representative data which provides real-world evidence of hospital care as it is delivered in the USA. This dataset includes treatment for all conditions and in all wards of general hospitals, and thus minimizes bias that may come from studies focusing on an individual healthcare system, region, or payment source. As such, this study describes the experience of those who used hospitals in the USA in 2019.
As is true of any real-world evidence, limitations of the study follow from the clinical data generating process on which these results are based.39,40,41,42 As a claims study, this analysis is necessarily limited to the billing for physical restraint status, and not on objective observation of restraint during hospitalization of the sort which studies based on electronic health records or proactive observation may have. If physical restraints are applied during a hospitalization but not coded for in the final discharge claim, then that hospitalization will be erroneously misclassified as not involving restraint. While we are not aware of literature assessing the accuracy of claims data for restraint, the fact that the 0.7% restraint rate found in the NIS is lower than the restraint rate in nearly all cross-sectional studies from different countries worldwide suggests that these results undercount the true incidence of restraint. As a speculative matter, we expect such a validation would show that coding of restraints is specific but not sensitive, but the present data are unable to test this expectation. Validation of this physical restraint status code will thus be important for future work in this area. Similarly, it is not known whether under-coding varies by clinical or demographic characteristics. As a result, systematic coding effects, meaning structural variation in who is diagnostically coded with restraint as opposed to true differences in clinical restraint rates, could explain the associations described here. The nature and duration of restraint, even when coded, are not captured by the available codes, making true outcomes a heterogenous group. That is, those who were restrained once briefly and those who spent most of their encounter restrained produce the same coded outcome despite the difference in clinical pictures. Understanding where or when during the hospital stay restraints were applied, such as critical care vs. general care, may provide better insight into restraint use as a safety intervention or a response to behavior. Finally, as the unit of sampling of the NIS is hospitalizations, and not individual patients, some individuals may be counted more than once for distinct hospitalizations (at the same or different healthcare facilities), which may bias the demographic information presented here.
CONCLUSION
A coded diagnosis of physical restraint status was present for 220,470 (95% CI: 208,114 to 232,826) hospitalizations in the 2019 NIS, or 0.7% of overall hospitalizations. There was significant variability in restraint coding based on sex and race, and restraint rate varied by more than 700-fold among clinical diagnoses. These results highlight potential care disparities in restraint utilization, which may have consequences for equity and health outcomes; however, validation of restrain coding in claims data is a critical further step in extending this of research.
Data Availability
Publicly available datasets were analyzed in this study. The dataset analyzed for this study can be obtained from the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality at https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
References
Bleijlevens MHC, Wagner LM, Capezuti E, Hamers JPH, Workgroup the IPR. Physical Restraints: Consensus of a Research Definition Using a Modified Delphi Technique. J Am Geriatr Soc. 2016;64(11):2307-2310. doi:https://doi.org/10.1111/jgs.14435.
Mohr WK. Restraints and the Code of Ethics: an Uneasy Fit. Arch Psychiatr Nurs. 2010;24(1):3-14. doi:https://doi.org/10.1016/j.apnu.2009.03.003.
Crutchfield P, Gibb TS, Redinger MJ, Ferman D, Livingstone J. The Conditions for Ethical Application of Restraints. Chest. 2019;155(3):617-625. doi:https://doi.org/10.1016/j.chest.2018.12.005.
Romijn A, Frederiks BJM. Restriction on Restraints in the Care for People With Intellectual Disabilities in the Netherlands: Lessons Learned from Australia, UK, and United States. J Policy Pract Intellect Disabil. 2012;9(2):127-133. doi:https://doi.org/10.1111/j.1741-1130.2012.00345.x.
Mohr WK, Petti TA, Mohr BD. Adverse Effects Associated with Physical Restraint. Can J Psychiatry. 2003;48(5):330-337. doi:https://doi.org/10.1177/070674370304800509.
Wong AH, Ray JM, Rosenberg A, et al. Experiences of Individuals Who Were Physically Restrained in the Emergency Department. JAMA Netw Open. 2020;3(1):e1919381. doi:https://doi.org/10.1001/jamanetworkopen.2019.19381.
Franks ZM, Alcock JA, Lam T, Haines KJ, Arora N, Ramanan M. Physical Restraints and Post-Traumatic Stress Disorder in Survivors of Critical Illness. A Systematic Review and Meta-analysis. Ann Am Thorac Soc. 2021;18(4):689-697. doi:https://doi.org/10.1513/AnnalsATS.202006-738OC.
Sze TW, Leng CY, Lin SKS. The Effectiveness of Physical Restraints in Reducing Falls Among Adults in Acute Care Hospitals and Nursing Homes: a Systematic Review. JBI Libr Syst Rev. 2012;10(5):307-351. doi:https://doi.org/10.11124/jbisrir-2012-4.
Chang LY, Wang KWK, Chao YF. Influence of Physical Restraint on Unplanned Extubation of Adult Intensive Care Patients: a Case-Control Study. Am J Crit Care. 2008;17(5):408-415. doi:https://doi.org/10.4037/ajcc2008.17.5.408.
Rose L, Burry L, Mallick R, et al. Prevalence, Risk Factors, and Outcomes Associated with Physical Restraint Use in Mechanically Ventilated Adults. J Crit Care. 2016;31(1):31-35. doi:https://doi.org/10.1016/j.jcrc.2015.09.011.
Staggs VS. Variability in Psychiatric Facility Seclusion and Restraint Rates as Reported on Hospital Compare Site. PS. 2020;71(9):893-898. doi:https://doi.org/10.1176/appi.ps.202000011.
Thomann S, Zwakhalen S, Richter D, Bauer S, Hahn S. Restraint Use in the Acute-Care Hospital Setting: a Cross-Sectional Multi-centre Study. Int J Nurs Stud. 2021;114:103807. doi:https://doi.org/10.1016/j.ijnurstu.2020.103807.
Reitan SK, Helvik AS, Iversen V. Use of Mechanical and Pharmacological Restraint Over an Eight-Year Period and Its Relation to Clinical Factors. Nord J Psychiatr. 2018;72(1):24-30. doi:https://doi.org/10.1080/08039488.2017.1373854.
Kalula SZ, Petros SG. Use of Physical Restraint in Hospital Patients: a Descriptive Study in a Tertiary Hospital in South Africa. Curationis. 2016;39(1):1605. doi:https://doi.org/10.4102/curationis.v39i1.1605.
Eskandari F, Abdullah KL, Zainal NZ, Wong LP. Incidence Rate and Patterns of Physical Restraint Use Among Adult Patients in Malaysia. Clin Nurs Res. 2018;27(3):278-295. doi:https://doi.org/10.1177/1054773816677807.
Gu T, Wang X, Deng N, Weng W. Investigating Influencing Factors of Physical Restraint Use in China Intensive Care Units: a Prospective, Cross-Sectional, Observational Study. Aust Crit Care. 2019;32(3):193-198. doi:https://doi.org/10.1016/j.aucc.2018.05.002.
Okuno T, Itoshima H, Shin J ho, Morishita T, Kunisawa S, Imanaka Y. Physical Restraint of Dementia Patients in Acute Care Hospitals During the COVID-19 Pandemic: a Cohort Analysis in Japan. PLoS ONE. 2021;16(11):e0260446. doi:https://doi.org/10.1371/journal.pone.0260446.
Benbenbishty J, Adam S, Endacott R. Physical Restraint Use in Intensive Care Units Across Europe: the PRICE Study. Intensiv Crit Care Nurs. 2010;26(5):241-245. doi:https://doi.org/10.1016/j.iccn.2010.08.003.
Abraham J, Hirt J, Kamm F, Möhler R. Interventions to Reduce Physical Restraints in General Hospital Settings: a Scoping Review of Components and Characteristics. J Clin Nurs. 2020;29(17-18):3183-3200. doi:https://doi.org/10.1111/jocn.15381.
Barbui C, Purgato M, Abdulmalik J, et al. Efficacy of Interventions to Reduce Coercive Treatment in Mental Health Services: Umbrella Review of Randomised Evidence. Br J Psychiatry. 2021;218(4):185-195. doi:https://doi.org/10.1192/bjp.2020.144.
Elgwairi E, Yang S, Nugent K. Association of the All-Patient Refined Diagnosis-Related Groups Severity of Illness and Risk of Mortality Classification with Outcomes. South Med J. 2021;114(10):668-674. doi:https://doi.org/10.14423/SMJ.0000000000001306.
Santos JV, Viana J, Pinto C, et al. All Patient Refined-Diagnosis Related Groups’ (APR-DRGs) Severity of Illness and Risk of Mortality as Predictors of In-Hospital Mortality. J Med Syst. 2022;46(6):37. doi:https://doi.org/10.1007/s10916-022-01805-3.
Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12(10):e1001885. doi:https://doi.org/10.1371/journal.pmed.1001885.
Park M, Tang JHC. Changing the Practice of Physical Restraint Use in Acute Care. J Gerontol Nurs. 2007;33(2):9-16. doi:https://doi.org/10.3928/00989134-20070201-04.
Afriyie-Boateng M, Loftus C, Wiesenfeld L, Hunter M, Lawson A. Proactive Psychiatry Intervention Using a Nurse-Led Behavioral Response Model for Hospitalized Patients With Behavioral Disturbances. J Healthc Qual. 2019;41(5):267-273. doi:https://doi.org/10.1097/JHQ.0000000000000208.
Williamson R, Lauricella K, Browning A, et al. Patient Factors Associated with Incidents of Aggression in a General Inpatient Setting. J Clin Nurs. 2014;23(7-8):1144-1152. doi:https://doi.org/10.1111/jocn.12294.
Tachibana M, Inada T, Ichida M, Ozaki N. Risk Factors for Inducing Violence in Patients with Delirium. Brain Behav. 2021;11(8):e2276. doi:https://doi.org/10.1002/brb3.2276.
Cipriani G, Vedovello M, Nuti A, Di Fiorino M. Aggressive Behavior in Patients with Dementia: Correlates and Management. Geriatr Gerontol Int. 2011;11(4):408-413. doi:https://doi.org/10.1111/j.1447-0594.2011.00730.x.
Wharton T, Ford BK. What is Known About Dementia Care Recipient Violence & Aggression Against Caregivers? J Gerontol Soc Work. 2014;57(5):460-477. doi:https://doi.org/10.1080/01634372.2014.882466.
McCoy TH, Snapper L, Stern TA, Perlis RH. Underreporting of Delirium in Statewide Claims Data: Implications for Clinical Care and Predictive Modeling. Psychosomatics. 2016;57(5):480-488. doi:https://doi.org/10.1016/j.psym.2016.06.001.
Wilkinson T, Ly A, Schnier C, et al. Identifying Dementia Cases with Routinely Collected Health Data: a Systematic Review. Alzheimers Dement. 2018;14(8):1038-1051. doi:https://doi.org/10.1016/j.jalz.2018.02.016.
Castro VM, Roberson AM, McCoy TH, et al. Stratifying Risk for Renal Insufficiency Among Lithium-Treated Patients: an Electronic Health Record Study. Neuropsychopharmacology. 2016;41(4):1138-1143. doi:https://doi.org/10.1038/npp.2015.254.
Luccarelli J, Kalluri AS, Thom RP, Hazen EP, Pinsky E, McCoy Jr TH. The Occurrence of Delirium Diagnosis among Youth Hospitalizations in the United States: a Kids’ Inpatient Database Analysis. Acta Psychiatrica Scandinavica. n/a(n/a). doi:https://doi.org/10.1111/acps.13473.
Raguan B, Wolfovitz E, Gil E. Use of physical restraints in a general hospital: a cross-sectional observational study. Isr Med Assoc J. 2015;17(10):633-638.
Souza LM da S, Santana RF, Capeletto C da SG, Menezes AK, Delvalle R. Factors associated with mechanical restraint in the hospital environment: a cross-sectional study. Rev Esc Enferm USP. 2019;53:e03473. doi:https://doi.org/10.1590/S1980-220X2018007303473.
Wong AH, Whitfill T, Ohuabunwa EC, et al. Association of Race/Ethnicity and Other Demographic Characteristics With Use of Physical Restraints in the Emergency Department. JAMA Netw Open. 2021;4(1):e2035241. doi:https://doi.org/10.1001/jamanetworkopen.2020.35241.
Schnitzer K, Merideth F, Macias-Konstantopoulos W, Hayden D, Shtasel D, Bird S. Disparities in Care: the Role of Race on the Utilization of Physical Restraints in the Emergency Setting. Acad Emerg Med. 2020;27(10):943-950. doi:https://doi.org/10.1111/acem.14092.
MacIntosh T, Desai MM, Lewis TT, Jones BA, Nunez-Smith M. Socially-Assigned Race, Healthcare Discrimination and Preventive Healthcare Services. PLoS ONE. 2013;8(5):e64522. doi:https://doi.org/10.1371/journal.pone.0064522.
Sherman RE, Anderson SA, Dal Pan GJ, et al. Real-World Evidence - What Is It and What Can It Tell Us? N Engl J Med. 2016;375(23):2293-2297. doi:https://doi.org/10.1056/NEJMsb1609216.
Kim HS, Lee S, Kim JH. Real-world Evidence Versus Randomized Controlled Trial: Clinical Research Based on Electronic Medical Records. J Korean Med Sci. 2018;33(34):e213. doi:https://doi.org/10.3346/jkms.2018.33.e213.
Eichler HG, Pignatti F, Schwarzer-Daum B, et al. Randomized Controlled Trials Versus Real World Evidence: Neither Magic Nor Myth. Clin Pharmacol Ther. 2021;109(5):1212-1218. doi:https://doi.org/10.1002/cpt.2083.
Nazha B, Yang JCH, Owonikoko TK. Benefits and Limitations of Real-World Evidence: Lessons from EGFR Mutation-Positive Non-Small-Cell Lung Cancer. Futur Oncol. 2021;17(8):965-977. doi:https://doi.org/10.2217/fon-2020-0951.
Funding
This work was supported by the National Institute of Mental Health (T32MH112485, JL; R01MH120991, THM). The sponsor had no role in study design, writing of the report, or data collection, analysis, or interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
JL receives funding from Harvard Medical School Dupont Warren Fellowship and Livingston Awards. He has received equity in Revival Therapeutics, Inc. THM receives funding from Institute of Mental Health, National Human Genome Research Institute Home, Telefonica Alpha, and Springer Nature. The remaining authors have no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luccarelli, J., Sacks, C.A., Snydeman, C. et al. Coding for Physical Restraint Status Among Hospitalized Patients: a 2019 National Inpatient Sample Analysis. J GEN INTERN MED 38, 2461–2469 (2023). https://doi.org/10.1007/s11606-023-08179-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08179-3