Abstract
Background
Women who use drugs (WWUD) have low rates of contraceptive use and high rates of unintended pregnancy. Drug use is common among women in rural U.S. communities, with limited data on how they utilize reproductive, substance use disorder (SUD), and healthcare services.
Objective
We determined contraceptive use prevalence among WWUD in rural communities then compared estimates to women from similar rural areas. We investigated characteristics of those using contraceptives, and associations between contraceptive use and SUD treatment, healthcare utilization, and substance use.
Design
Rural Opioids Initiative (ROI) — cross-sectional survey using respondent-driven sampling (RDS) involving eight rural U.S. regions (January 2018–March 2020); National Survey on Family Growth (NSFG) — nationally-representative U.S. household reproductive health survey (2017–2019).
Participants
Women aged 18–49 with prior 30-day non-prescribed opioid and/or non-opioid injection drug use; fecundity determined by self-reported survey responses.
Main Measures
Unweighted and RDS-weighted prevalence estimates of medical/procedural contraceptive use; chi-squared tests and multi-level linear regressions to test associations.
Key Results
Of 855 women in the ROI, 36.8% (95% CI 33.7–40.1, unweighted) and 38.6% (95% CI 30.7–47.2, weighted) reported contraceptive use, compared to 66% of rural women in the NSFG sample. Among the ROI women, 27% had received prior 30-day SUD treatment via outpatient counseling or inpatient program and these women had increased odds of contraceptive use (aOR 1.50 [95% CI 1.08–2.06]). There was a positive association between contraception use and recent medications for opioid use disorder (aOR 1.34 [95% CI 0.95–1.88]) and prior 6-month primary care utilization (aOR 1.32 [95% CI 0.96–1.82]) that did not meet the threshold for statistical significance.
Conclusion
WWUD in rural areas reported low contraceptive use; those who recently received SUD treatment had greater odds of contraceptive use. Improvements are needed in expanding reproductive and preventive health within SUD treatment and primary care services in rural communities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
In the United States (U.S.), women are using drugs at increasing rates,1 with consequent rises in overdose deaths, substance-exposed pregnancies, and other related consequences over the past two decades.1,2 The national prevalence of maternal opioid-related diagnoses at time of hospital delivery3,4 and neonatal opioid withdrawal syndrome (NOWS) have increased considerably,4 with trends indicating higher rates of maternal opioid-related diagnoses and NOWS in rural compared to urban U.S. areas.5 Reproductive-age women who use drugs (WWUD) experience unintended pregnancies at up to double the rate than the general population.6 A contributing factor is substantially lower rates of highly effective contraceptive utilization among WWUD as compared to women who do not use drugs.7 Nationwide household surveys including the National Survey on Family Growth (NSFG), which include no questions about substance use, likely fail to capture the reproductive health needs of WWUD, particularly those in rural communities.8 Despite increasing awareness surrounding unintended pregnancies and associated maternal and neonatal morbidity and mortality among WWUD, little is known about disparities in utilization of reproductive health services of WWUD in rural communities.
Individual, community, and environmental factors contribute to 60–90% of pregnancies being unintended among WWUD,6 compared to 45% among the general U.S. population.9 WWUD less often use highly effective contraceptive methods (long-acting reversible contraception — intrauterine device or implant), and effective methods (hormonal pill, patch, injection, or ring),7,10,11 while relying heavily on condoms for contraception.7,12 Condoms are less effective at preventing pregnancy, given imperfect and inconsistent use. Contraceptive use and reproductive choice by WWUD is further influenced by high rates of intimate partner violence and sexual and reproductive coercion.13,14 While not all WWUD want or need highly or moderately effective contraception, the notable differences in unintended pregnancy rates may indicate a gap in reproductive health access and utilization and necessitates further investigation and interventions. Pregnant and parenting WWUD also face considerable stigma,15 frequently delaying or avoiding prenatal care, citing concerns around child protective service involvement and potential custodial loss.16,17 Delays to care contribute to maternal and neonatal complications including placental rupture, premature delivery, NOWS, and intrauterine growth restriction.18
Gender and sex-related factors unique to women contribute to their initial substance use, progression from initial use to SUD, and substance use disorder (SUD) treatment engagement and retention.2 WWUD tend to engage in higher-risk injection and sexual behaviors, experience higher rates of intimate partner violence, and have higher risk of acquiring HIV and HCV than their male counterparts.19,20,21 WWUD from rural communities experience additional layers of risk compared to WWUD in urban settings.22,23 In rural communities, WWUD experience poorer health outcomes partially due to unique barriers to accessing healthcare and reproductive services (limited service availability, insurance/financial concerns, limited transportation),22,24,25 and SUD treatment (specialist shortages,26 drive times to specialists,27 and rural-specific stigma28,29).
Large-scale efforts are needed to expand access to family planning and reproductive services for WWUD in various care settings, particularly in rural communities where these services are generally lacking.30 However, there are limited data on current contraceptive use in the rural U.S. by WWUD. We sought to estimate contraceptive use prevalence among WWUD in rural communities compared to a national sample of women from rural areas, one of the first studies to do so. We hypothesized that WWUD in rural communities would have lower prevalence of contraceptive use compared to a nationally representative sample of women living in rural areas. We also aimed to identify characteristics of WWUD in rural communities associated with contraceptive use and to evaluate possible associations between contraceptive use and SUD treatment utilization, health care utilization, substance use, and HIV/HCV testing. We hypothesized that recent SUD treatment and healthcare utilization would be associated with increased contraceptive utilization, those with recent substance use would have reduced contraceptive utilization, and recent HIV/HCV testing would be associated with increased contraceptive utilization.
METHODS
Rural Opioids Initiative — Study Design, Participants, and Data Collection
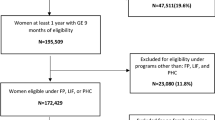
This investigation is a sub-analysis of the Rural Opioids Initiative (ROI) — a multi-site cross-sectional survey of people who use drugs from ten U.S. states (Illinois; Kentucky; North Carolina; New England which included Massachusetts, Vermont, and New Hampshire; Ohio; Oregon; Wisconsin; and West Virginia) with recruitment from January 2018 to March 2020.31 The ROI collected data on demographics, drug use, consequences of use, SUD treatment, HIV/HCV screening and treatment, and healthcare utilization. Eligible participants reported use of any opioid via any administration route and/or any other drug via injection in the prior 30 days “to get high” (e.g., smoking heroin; injecting heroin and smoking cocaine; injecting methamphetamine) except for Wisconsin which limited to injection use only. Inclusion criterion for all sites was age ≥18 years old except two states (Illinois, Wisconsin) where the age criterion was ≥15 years old. For this analysis, our study population included all women 18 to 49 years old who were able to become pregnant determined by survey responses. The upper age limit of 49 years aligns with the NSFG. The NSFG includes women between 15 and 18 years old; however, given only two ROI sites included this younger age range, with only two participants otherwise meeting inclusion criteria, they were excluded from further analysis.
All sites conducted recruitment using modified chain-referral sampling,31,32 a strategy based on respondent-driven sampling (RDS) methods to improve sampling of “hidden” populations.33,34 Study sites identified “seed” participants who represented local population demographics and recruited within their network. Participants were linked via referral chains when estimating weighted prevalence rates. Additional ROI data collection and management details are previously published.31 The ROI data coordinating center collected, standardized, managed, and distributed data for analyses approved by the publication committee. All study procedures were approved by the Institutional Review Board at each site.
National Survey of Family Growth
The National Center for Health Statistics conducts the NSFG,35,36 collecting nationally representative household estimates of family planning and reproductive health topics for men and women.35 The NSFG does not ask about drug use and as a household survey does not include those currently incarcerated or unhoused.8 The NSFG age limit expanded from 15–44 to 15–49 years old with the 2015–2017 cohort, and purposefully oversamples non-Hispanic Blacks, Hispanics, and teens.35,36 The NSFG uses U.S. Census Bureau Office of Management and Budget for residence location. We included NSFG respondents residing outside of U.S. Census Metropolitan Statistical Areas to approximate ROI regions.
Measures
We determined the ROI population of reproductive-age women who were not currently pregnant but could become pregnant via survey responses. The ROI survey asked all participants their gender (male, female, transgender, other) and was designed so only participants identifying as “female” were asked their pregnancy status (yes, no, or don’t know). Participants who selected “no” or “don’t know” regarding pregnancy status were then asked, “Are you using any medical forms of birth control such as pills, an IUD, implant, injection, ring, or patch, or are your ‘tubes tied’?” (yes, no, not applicable [no vaginal sex with a male in past 10 months], not applicable [not physically able to get pregnant right now — hysterectomy, health condition, menopause], or decline to answer). Those who answered “yes” or “no” were included in the analysis. We use the term “medical/procedural contraceptive” to encompass all medical forms of hormonal contraception (pill, injection, ring, patch) and all procedural/surgical contraceptive measures (intrauterine device, implant, tubal ligation) consistent with the ROI survey. Participants were not asked additional details about contraceptive methods, family planning preferences, or adequate information to assess use of condoms or other barrier methods as contraception.
The primary variable was medical/procedural contraceptive use. Characteristics potentially associated with contraceptive use were examined on the basis of previous literature and a priori hypotheses.9,37,38 We included categorical characteristics: age; education level; race/ethnicity; relationship status. We included yes/no characteristics: homelessness in prior 6 months; incarceration in prior 6 months; trading sex for drugs, money, or housing in prior 30 days; and having had sex without a condom ≥ 1 time in prior 30 days.
We divided SUD treatment service utilization within the prior 30 days into two categories: (1) medication for opioid use disorder (MOUD) use (buprenorphine, methadone, or naltrexone), and (2) SUD treatment via outpatient counseling or inpatient/residential program. Survey participants could indicate use of more than one SUD treatment (e.g., prescribed buprenorphine and engaged in counseling). Another outcome was healthcare location in the prior 6 months with four categories: (1) ambulatory care (private clinician or community health), (2) acute care (urgent care or emergency department), (3) health department or mobile van, (4) no care received. Other outcomes included the following: prior 30-day substance use (opioids, methamphetamine, cocaine, alcohol, or tobacco) and prior year HIV/HCV testing.
Analyses
We used descriptive statistics to summarize participant characteristics, prevalence estimates, and site-specific variation of medical/procedural contraceptive use. Overall, unweighted and RDS-weighted estimates of medical/procedural contraceptive use and 95% confidence intervals were calculated using mixed-effects models.34 Study site was the random effect in these models, and estimates were obtained by averaging over site-specific effects. We then stratified the data by site to compute site-specific estimates of medical/procedural contraceptive use and bootstrapped 95% confidence intervals. West Virginia was excluded from weighted estimates due to incomplete RDS data at time of analysis.
To compare rates of medical/procedural contraceptive use between the ROI and NSFG groups, we restricted the NSFG sample of women to match the ROI inclusion criteria, excluding currently pregnant NSFG respondents, those not sexually active within the past 10 months, and those reporting infertility due to a medical condition or non-contraceptive surgery. Differences in age, race/ethnicity, and education between the ROI and NSFG samples were assessed using chi-squared test with Rao and Scott’s second-order correction to account for weighting in the NSFG survey data. We fit a logistic regression model on the pooled sample and calculated marginal means to estimate the rates of medical/procedural contraceptive use in the ROI and NSFG groups after adjusting for demographic differences.
Within the ROI sample, we assessed bivariate associations between contraceptive use and participant characteristics using Pearson’s chi-square test. Multivariable associations were assessed using generalized linear mixed methods with site-level random intercepts between contraceptive use and MOUD treatment; SUD treatment with outpatient counseling or inpatient program; primary care access with ambulatory services (private clinician or community health center); recent substance use; and HIV/HCV testing. Potential confounders with p-values ≤ 0.10 in bivariate analyses were included as covariates in each model, in addition to the main independent variable of medical/procedural contraceptive use. Analyses were conducted in R v.4.0.5 using the ‘lme4’ package.
RESULTS
The ROI recruited 3,048 participants from eight study sites. Sixteen (0.5%) who self-identified as transgender or other gender and 30 (3.4%) women who were currently pregnant were excluded from the analytic sample. Our sample included 855 WWUD, with average age 33 years (SD 8), who were predominantly White (83%) and insured (79%) (Table 1). Overall, 50% had engaged in condom-less sex in the prior 30 days and 53% had experienced homelessness in the prior 6 months. The overall prevalence of medical/procedural contraceptive use was 36.8% unweighted (95% CI 33.7, 40.1) and 38.6% weighted (95% CI 30.7, 47.2) (Table 2). Overall and site-specific prevalence estimates of medical/procedural contraceptive use are listed in Table 2.
In the prior 30 days, 85% of those in ROI sample had used opioids/heroin/fentanyl and 73% had used methamphetamine/crystal (Table 1). Women reporting not using a medical/procedural contraceptive were more likely to have recently used methamphetamine than those who used contraception (76% vs. 69%; p=0.021). This difference was also seen in those who used both opioids and methamphetamine (64% vs. 55%; p= 0.015) Women who reported medical/procedural contraceptive use were more likely to have received SUD treatment using MOUD in the prior 30 days (25% vs. 20%; p=0.049) and SUD treatment via outpatient counseling, or inpatient program (33% vs. 24%; p=0.006) compared to those not using contraceptives.
In analyses adjusted for age, race/ethnicity, education level, relationship status, recent homelessness, and insurance status, those in the ROI sample who used SUD treatment services via outpatient counseling or inpatient program within the prior 30 days were 50% more likely to report contraceptive use compared to those who had not (aOR 1.50 [95% CI 1.08–2.06) (Table 3). There was no evidence supporting an association between contraceptive use and recent opioid/heroin/fentanyl, cocaine/crack, combined opioid and cocaine, alcohol, or tobacco use. However, those with recent methamphetamine use, whether alone or in combination with opioids, were less likely to use medical/procedural contraceptive than those without recent methamphetamine use (aOR 0.72 [95% CI 0.52, 0.99]; aOR 0.71 [95% CI 0.53, 0.95], respectively).
There were 570 women included in the NSFG cohort; 46 were excluded as they were currently pregnant (7.5%). This cohort sample is representative of 7,035,913 housed women of unknown drug use status who live in rural areas. Women in the ROI compared to the NSFG sample of women had a 69% lower likelihood of medical/procedural contraceptive use (aOR 0.31 [95% CI, 0.25–0.4]) after controlling for age, race/ethnicity, and education. Women in the NSFG sample were more racially and ethnically diverse and more likely to have attained some college education or higher compared to the ROI sample (Table 4).
DISCUSSION
Medical/procedural contraceptive use by reproductive-age WWUD in rural U.S. communities was substantially lower (36.8% unweighted across all sites, 38.6% weighted all sites except West Virginia), compared to women from rural communities surveyed in the NSFG, of whom 66% reported medical/procedural contraceptive use. The NSFG likely includes some WWUD; however, given the high prevalence of recent homelessness (53%) and incarceration (40%) among the ROI WWUD, household-based surveys such as NSFG likely miss the majority of those in this highly stigmatized and marginalized population. Our findings highlight the urgency for better addressing the reproductive health and family planning needs for WWUD in rural America who experience marked socioeconomic consequences and medical complications of unintended pregnancies.
We found a positive association in the ROI with prior 30-day SUD treatment involving outpatient counseling or inpatient program suggesting that these interventions that often involve more time with patients are perhaps more likely to give advice regarding contraception and family planning. While recent MOUD use was greater among women using contraception than those not using contraception (25% vs. 20%), the positive association with MOUD treatment and contraception use did not meet the threshold for statistical significance (aOR 1.34 [95% CI 0.95–1.88]). This discrepancy could perhaps be explained by the high prevalence of methamphetamine use in the ROI population, and current lack of FDA-approved medications to treat stimulant use disorders. Overall, the ROI population had a low utilization of SUD treatment, with 22% recently receiving MOUD and 27% utilizing outpatient counseling, or inpatient program — indicating a clear need to expand access and utilization of SUD treatment in rural communities. SUD treatment encounters are a potential missed opportunity to discuss reproductive health and offer contraceptives to those interested.39
Among the ROI population, 44% reported they primarily utilized healthcare via ambulatory services with a positive association between using medical/procedural contraceptive and prior 6-month utilization of ambulatory services that did not meet the threshold for statistical significance (aOR 1.32 [95% CI 0.96–1.82]), after controlling for insurance status. This suggests that factors besides disparities in healthcare access and availability may be contributing to lower contraceptive use among WWUD in rural areas. Outpatient clinicians caring for WWUD are frequently addressing more acute medical and psychosocial issues and they may wait until patients are deemed more stable before discussing family planning.40 WWUD, particularly those currently pregnant, face considerable stigma — thus may be reluctant or uncomfortable accessing medical services.41 WWUD may also have less trust in the healthcare system,42 which, along with child custody and criminal/legal concerns, could hinder counseling on reproductive health. Some women are also equivocal about possibly getting pregnant, and WWUD more frequently report ambivalence around child-bearing or believe they cannot conceive.43 Clinicians need to consider what constitutes patient-centered contraceptive counseling and family planning,44 particularly given the stigma, discrimination, and historical harms WWUD have experienced and concerns around possible or perceived coercion. There is a critical need for development of women-specific integrated programs offering SUD treatment and/or harm reduction services with reproductive health services,30,45,46 in various service delivery models. Pregnant and parenting WWUD may also benefit from these types of care models.47,48 Rural communities, with less overall healthcare availability, have further limitations in availability of SUD treatment programs that include wraparound services (behavioral health, social services) and family-specific programs.49 This further emphasizes the importance of primary care clinics in delivering SUD treatment and reproductive health services for WWUD in rural areas.
Women with prior 30-day methamphetamine use alone or in combination with opioids had a lower likelihood of using medical/procedural contraceptive compared to those not recently using methamphetamine. Lower contraceptive use in women using methamphetamine is noteworthy given methamphetamine is frequently used for energy and sexual enhancement and is associated with higher-risk sexual behaviors and STI, HIV, and HCV transmission.50 Of the 855 ROI participants, 50% had reported prior 30-day condom-less sex. Methamphetamine is also disproportionately used in many rural communities,51,52 and 73% of women in our study reported recent use. Research into the most effective contraceptive options and family planning services for women who use methamphetamine is warranted.
HIV/HCV testing within the last year was low, at 35%, regardless of contraceptive use. Women who inject drugs are at higher risk for acquiring HIV, HCV, and other infections, given high rates of needle sharing, high-risk sexual behaviors, transactional sex, and engagement in sex work.21 Women who inject drugs and those engaging in transactional sex and sex work should be screened for HIV and offered pre- and post-exposure prophylaxis (PrEP/PEP) to reduce HIV acquisition risk.53 Testing and treating reproductive-age WWUD for sexually transmitted and blood-borne infections is important for their health and to reduce the likelihood of vertical transmission if they were to become pregnant.54 Efforts are needed to expand adoption of clinical practice guidelines around prescribing PrEP/PEP, screening for infectious disease, and offering highly effective HCV curative treatment for WWUD in rural communities in various treatment settings.
Limitations and Future Directions
There are limitations to our study. When participants were asked about contraceptive use, one choice included not using contraception as they were “not physically able to get pregnant right now” with reasons including “hysterectomy, health condition, menopause.” Given the incorrect assumption among many WWUD that they are unable to get pregnant,43,55,56 our sample may underrepresent the number of reproductive-age women who could become pregnant. The cross-sectional survey design only assessed contraceptive use at one timepoint. We also did not collect more detailed information about specific contraceptive methods thus limiting assessing differences in use of highly versus moderately effective methods or use of combined methods. Further research is needed to study contraceptive and family planning preferences and how to provide patient-centered contraceptive counseling for WWUD.44 The survey also did not ask participants’ plans or desire for pregnancy or about their use of condoms or other less effective methods including rhythm or withdrawal as primary or additional form of contraception. The ROI sample also lacked racial/ethnic diversity, a major limitation, given Black, Latina, and multi-racial women face increased rates of reproductive coercion and unintended pregnancy.57 They also experience gendered racism and reproductive harms by the healthcare system with ongoing mistrust of contraceptive counseling.58 Finally, the survey only asked female-identifying participants to answer questions about contraceptives and pregnancy. We note that female-identified individuals are not the only people who use contraception, need reproductive services, and can get pregnant. Studies are needed on approaches to best serve people of all racial/ethnic and gender identities who use drugs and who can become pregnant.
Some sites had large variation between weighted and unweighted prevalence estimates — particularly Illinois which went from a 31.1 to 61.9% estimated prevalence. This can be explained by very short referral chain lengths in Illinois for women who reported contraceptive use, leading to these participants being weighted more heavily. The smaller the network — the number of community connections a participant has — the more these participants are weighted in statistical calculations to account for the possibility that those with smaller networks (shorter referral chains) represent a more difficult to reach and recruit population when calculating prevalence estimates.
Conclusion
Despite these limitations, our study provides important insights into the lower prevalence of contraceptive use among WWUD in rural communities compared to a general population of rural women. Interventions that expand access to and improve integration of reproductive health services within SUD treatment, primary care, and harm reduction programs for WWUD are urgently needed in rural areas.
Abbreviations
- MOUD :
-
medications for opioid use disorder
- NOWS :
-
neonatal opioid withdrawal syndrome
- NSFG :
-
National Survey on Family Growth
- PEP :
-
post-exposure prophylaxis
- PrEP :
-
pre-exposure prophylaxis
- RDS :
-
respondent driven sampling
- ROI :
-
Rural Opioid Initiative
- SUD :
-
substance use disorder
- U.S. :
-
United States
- WWUD :
-
women who use drugs
References
Substance Abuse and Mental Health Services Administration (SAMHSA). 2019 National Survey on Drug Use and Health. Rockville, MD; 2020. https://www.samhsa.gov/data/release/2019-national-survey-drug-use-and-health-nsduh-releases.
Ait-Daoud N, Blevins D, Khanna S, Sharma S, Holstege CP, Amin P. Women and addiction: an update. Med Clin North Am. 2019;103(4):699-711. doi:https://doi.org/10.1016/j.mcna.2019.03.002
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization — United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845-849. doi:https://doi.org/10.15585/mmwr.mm6731a1
Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA - J Am Med Assoc. 2021;325(2):146-155. doi:https://doi.org/10.1001/jama.2020.24991
Villapiano NLG, Winkelman TNA, Kozhimannil KB, Davis MM, Patrick SW. Rural and urban differences in neonatal abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2017;171(2):194-196. doi:https://doi.org/10.1001/jamapediatrics.2016.3750
Heil SH, Jones HE, Arria A, et al. Unintended pregnancy in opioid-abusing women. J Subst Abuse Treat. 2011;40(2):199-202. doi:https://doi.org/10.1016/j.jsat.2010.08.011
Terplan M, Hand DJ, Hutchinson M, Salisbury-Afshar E, Heil SH. Contraceptive use and method choice among women with opioid and other substance use disorders: a systematic review. Prev Med (Baltim). 2015;80:23-31. doi:https://doi.org/10.1016/j.ypmed.2015.04.008
Armstrong KA, Kennedy MG, Kline A, Tunstall C. Reproductive health needs: comparing women at high, drug-related risk of HIV with a national sample. J Am Med Womens Assoc. 1999;54(2).
Finer L, Zolna M. Declines in unintended pregnancy in the United States, 2008-2011. N Engl J Med. 2016;374(9):843-852. doi:https://doi.org/10.1056/NEJMSA1506575
Charron E, Rennert L, Mayo RM, Eichelberger KY, Dickes L, Truong KD. Contraceptive initiation after delivery among women with and without opioid use disorders: a retrospective cohort study in a statewide Medicaid population, 2005–2016. Drug Alcohol Depend. 2021;220. doi:https://doi.org/10.1016/j.drugalcdep.2021.108533
Griffith G, Kumaraswami T, Chrysanthopoulou SA, Mattocks KM, Clark RE. Prescription contraception use and adherence by women with substance use disorders. Addiction. 2017;112(9):1638-1646. doi:https://doi.org/10.1111/add.13840
Black KI, Stephens C, Haber PS, Lintzeris N. Unplanned pregnancy and contraceptive use in women attending drug treatment services. Aust New Zeal J Obstet Gynaecol. 2012;52(2):146-150. doi:https://doi.org/10.1111/j.1479-828X.2012.01413.x
Bergmann JN, Stockman JK. How does intimate partner violence affect condom and oral contraceptive Use in the United States?: a systematic review of the literature. Contraception. 2015;91(6):438-455. doi:https://doi.org/10.1016/j.contraception.2015.02.009
Stone RH, Griffin B, Fusco RA, Vest K, Tran T, Gross S. Factors affecting contraception access and use in patients with opioid use disorder. J Clin Pharmacol. 2020;60(S2):S63-S73. doi:https://doi.org/10.1002/jcph.1772
Choi S, Rosenbloom D, Stein MD, Raifman J, Clark JA. Differential gateways, facilitators, and barriers to substance use disorder treatment for pregnant women and mothers. J Addict Med. 2021;Publish Ah(00):1-12. doi:https://doi.org/10.1097/adm.0000000000000909
O’Connor A, Harris E, Hamilton D, Fisher C, Sachmann M. The experiences of pregnant women attending a specialist service and using methamphetamine. Women and Birth. 2020;(2019):1-10. doi:https://doi.org/10.1016/j.wombi.2020.01.011
Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Heal Justice 2015 31. 2015;3(1):1-15. doi:https://doi.org/10.1186/S40352-015-0015-5
Smith K, Lipari RN. Women of Childbearing Age and Opioids. Rockville, MD; 2017. https://www.samhsa.gov/data/sites/default/files/report_2724/ShortReport-2724.html.
Tuchman E. Women’s injection drug practices in their own words: a qualitative study. Harm Reduct J. 2015;12(1). doi:https://doi.org/10.1186/S12954-015-0041-6
Roberts A, Mathers B, Degenhardt L. Women who inject drugs: a review of their risks, experiences and needs. Sydney, Australia; 2010. https://www.unodc.org/documents/hiv-aids/Women_who_inject_drugs.pdf.
Iversen J, Page K, Madden A, Maher L. HIV, HCV, and health-related harms among women who inject drugs: implications for prevention and treatment. J Acquir Immune Defic Syndr. 2015;69:S176-S181. doi:https://doi.org/10.1097/QAI.0000000000000659
Lutfiyya MN, McCullough JE, Haller I V., Waring SC, Bianco JA, Lipsky MS. Rurality as a root or fundamental social determinant of health. Disease-a-Month. 2012;58(11):620-628. doi:https://doi.org/10.1016/J.DISAMONTH.2012.08.005
Thomas N, van de Ven K, Mulrooney KJD. The impact of rurality on opioid-related harms: a systematic review of qualitative research. Int J Drug Policy. 2020;85(December 2019):102607. doi:https://doi.org/10.1016/j.drugpo.2019.11.015
Anderson TJ, Saman DM, Lipsky MS, Lutfiyya MN. A cross-sectional study on health differences between rural and non-rural U.S. counties using the County Health Rankings. BMC Heal Serv Res 2015 151. 2015;15(1):1-8. doi:https://doi.org/10.1186/S12913-015-1053-3
Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. 2004;94(10):1682-1686. doi:10.2105/AJPH.94.10.1682
Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw Open. 2019;2(6). doi:https://doi.org/10.1001/jamanetworkopen.2019.6373
Joudrey PJ, Chadi N, Roy P, et al. Pharmacy-based methadone dispensing and drive time to methadone treatment in five states within the United States: a cross-sectional study. Drug Alcohol Depend. 2020;211(March). doi:https://doi.org/10.1016/j.drugalcdep.2020.107968
Ezell JM, Walters S, Friedman SR, et al. Stigmatize the use, not the user? Attitudes on opioid use, drug injection, treatment, and overdose prevention in rural communities. Soc Sci Med. 2021;268(October 2020):113470. doi:https://doi.org/10.1016/j.socscimed.2020.113470
Richard EL, Schalkoff CA, Piscalko HM, et al. “You are not clean until you’re not on anything”: perceptions of medication-assisted treatment in rural Appalachia. Int J Drug Policy. March 2020:102704. doi:https://doi.org/10.1016/j.drugpo.2020.102704
Heil SH, Melbostad HS, Rey CN. Innovative approaches to reduce unintended pregnancy and improve access to contraception among women who use opioids. Prev Med (Baltim). 2019;128(August):105794. doi:https://doi.org/10.1016/j.ypmed.2019.105794
Jenkins R, Whitney B, Nance R, et al. The Rural Opioid Initiative: cohort description. Under Rev - Am J Public Heal. 2021.
Joseph HA, Pan Y, Mendoza M, et al. HIV acquisition and transmission potential among African American men who have sex with men and women in three U.S. cities. Arch Sex Behav. 2018;47(1):183-194. doi:https://doi.org/10.1007/s10508-017-1052-z
Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44(2):174-199. doi:https://doi.org/10.1525/sp.1997.44.2.03x0221m
Volz E, Heckathorn D. Probability based estimation theory for respondent driven sampling. J Off Stat. 2008;24(1):79-97.
National Center for Health Statistics. Public Use Data File Documentation 2017-2019 National Survey of Family Growth User’s Guide. Hyattsville, MD; 2020. http://www.cdc.gov/nchs/nsfg/nsfg_2017_2019_puf.htm.
National Center for Health Statistics. 2017-2019 National Survey of Family Growth Public-Use Data and Documentation. Hyattsville, MD; 2020. http://www.cdc.gov/nchs/nsfg/nsfg_2017_2019_puf.htm.
Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90-96. doi:https://doi.org/10.1363/3809006
Smith C, Morse E, Busby S. Barriers to reproductive healthcare for women with opioid use disorder. J Perinat Neonatal Nurs. 2019;33(2):E3-E11. doi:https://doi.org/10.1097/JPN.0000000000000401
Elko A, Jansson LM. Contraception in drug-dependent women: a novel approach. Soc Work Ment Health. 2011;9(6):445-455. doi:https://doi.org/10.1080/15332985.2011.575723
Charron E, Mayo RM, Heavner-Sullivan SF, et al. “It’s a very nuanced discussion with every woman”: health care providers’ communication practices during contraceptive counseling for patients with substance use disorders. Contraception. 2020;102(5):349-355. doi:https://doi.org/10.1016/j.contraception.2020.09.002
Paris R, Herriott AL, Maru M, Hacking SE, Sommer AR. Secrecy versus disclosure: women with substance use disorders share experiences in help seeking during pregnancy. Matern Child Health J. 2020;24(11):1396-1403. doi:https://doi.org/10.1007/s10995-020-03006-1
Cockroft JD, Adams SM, Bonnet K, Matlock D, McMillan J, Schlundt D. “A scarlet letter”: stigma and other factors affecting trust in the health care system for women seeking substance abuse treatment in a community setting. Subst Abus. 2019;40(2):170-177. doi:https://doi.org/10.1080/08897077.2018.1544184
Macafee LK, Dalton V, Terplan M. Pregnancy intention, risk perception, and contraceptive use in pregnant women who use drugs. J Addict Med. 2019;13(3):177-181. doi:https://doi.org/10.1097/ADM.0000000000000471
Morse JE, Ramesh S, Jackson A. Reassessing unintended pregnancy: toward a patient-centered approach to family planning. Obstet Gynecol Clin North Am. 2017;44(1):27-40. doi:https://doi.org/10.1016/j.ogc.2016.10.003
Martin CE, Han JJ, Serio-Chapman C, Chaulk P, Terplan M. Injectable contraceptive continuation among female exotic dancers seeking mobile reproductive health services. J Health Care Poor Underserved. 2014;25(3):1317-1327.
Moore E, Han J, Serio-Chapman C, Mobley C, Watson C, Terplan M. Contraception and clean needles: feasibility of combining mobile reproductive health and needle exchange services for female exotic dancers. Am J Public Health. 2012;102(10):1833-1836. doi:https://doi.org/10.2105/AJPH.2012.300842
Joshi C, Skeer MR, Chui K, Neupane G, Koirala R, Stopka TJ. Women-centered drug treatment models for pregnant women with opioid use disorder: a scoping review. Drug Alcohol Depend. 2021;226(June):108855. doi:https://doi.org/10.1016/j.drugalcdep.2021.108855
Goodman DJ, Saunders EC, Frew JR, et al. Integrated vs nonintegrated treatment for perinatal opioid use disorder: retrospective cohort study. Am J Obstet Gynecol MFM. 2022;4(1):100489. doi:https://doi.org/10.1016/j.ajogmf.2021.100489
Clary E, Ribar C, Weigensberg E. Challenges in providing substance use disorder treatment to child welfare clients in rural communities. ASPE Res Br. 2020;(January):1-16.
Cheng WS, Garfein RS, Semple SJ, Strathdee SA, Zians JK, Patterson TL. Differences in sexual risk behaviors among male and female HIV-seronegative heterosexual methamphetamine users. Am J Drug Alcohol Abuse. 2009;35(5):295-300. doi:https://doi.org/10.1080/00952990902968585
Baker R, Leichtling G, Hildebran C, et al. ‘“ Like Yin and Yang ”’: perceptions of methamphetamine benefits and consequences among people who use opioids in rural communities. J Addict Med. 2020. doi:https://doi.org/10.1097/ADM.0000000000000669
Jones CM, Compton WM, Mustaquim D. Patterns and characteristics of methamphetamine use among adults — United States, 2015–2018. MMWR Morb Mortal Wkly Rep. 2020;69(12):317-323. doi:https://doi.org/10.15585/mmwr.mm6912a1
Centers for Disease Control and Prevention. U.S. Public Health Service - Preexposure Prophylaxis for the Prevention of HIV Infection in the United States - 2017 Update: A Clinical Practice Guideline.; 2018. doi:https://doi.org/10.1016/S0040-4039(01)91800-3
Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59(6):765-773. doi:https://doi.org/10.1093/cid/ciu447
Florsheim O, Ligten M Van, Augustine D, de Bocanegra HT, Perry R. P69 Addressing substance use disorder as a key component of contraceptive counseling for women who use injection drugs. Contraception. 2020;102(4):299. doi:https://doi.org/10.1016/j.contraception.2020.07.088
Harding C, Ritchie J. Contraceptive practice of women with opiate addiction in a rural centre. Aust J Rural Health. 2003;11(1):2-6. doi:https://doi.org/10.1046/j.1440-1584.2003.00477.x
Holliday CN, McCauley HL, Silverman JG, et al. Racial/ethnic differences in women’s experiences of reproductive coercion, intimate partner violence, and unintended pregnancy. J Women’s Heal. 2017;26(8):828-835. doi:https://doi.org/10.1089/jwh.2016.5996
Rosenthal L, Lobel M. Gendered racism and the sexual and reproductive health of Black and Latina Women. Ethn Heal. 2020;25(3):367-392. doi:https://doi.org/10.1080/13557858.2018.1439896
Acknowledgements
The authors thank the other ROI investigators and their teams, community and state partners, and the participants of the individual ROI studies for their valuable contributions. A full list of participating ROI institutions and other resources can be found at http://ruralopioidinitiative.org.
Funding
This publication is based upon data collected and/or methods developed as part of the Rural Opioid Initiative (ROI), a multi-site study with a common protocol that was developed collaboratively by investigators at eight research institutions and at the National Institute of Drug Abuse (NIDA), the Appalachian Regional Commission (ARC), the Centers for Disease Control and Prevention (CDC), and the Substance Abuse and Mental Health Services Administration (SAMHSA). Research presented in this manuscript is the result of secondary data harmonization and analysis and was supported by grant U24DA048538 from NIDA. Primary data collection was supported by grants UG3DA044829/UH3DA044829, UG3DA044798/UH3DA044798, UG3DA044830/UH3DA044830, UG3DA044823/UH3DA044823, UH3DA044822/UH3DA044822, UG3DA044831/UH3DA044831, UG3DA044825, UG3DA044826/UH3DA044826, and U24DA044801 co-funded by NIDA, ARC, CDC, and SAMHSA. XAL and RRC were supported by the AHRQ K12 HS026370. ESA was supported by the NIDA 0099148/00070029, NIDA UG1 DA050066-01, AHRQ 1R18HS027088-01, and NIDA 1U2CDA050098-01. KEL was supported by the NIDA K01DA048174.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations:
None at time of initial manuscript submission, plan to submit abstracts to Society of General Internal Medicine national meeting 2022 and College on Problems of Drug Dependence national meeting 2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Levander, X.A., Foot, C.A., Magnusson, S.L. et al. Contraception and Healthcare Utilization by Reproductive-Age Women Who Use Drugs in Rural Communities: a Cross-Sectional Survey. J GEN INTERN MED 38, 98–106 (2023). https://doi.org/10.1007/s11606-022-07558-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07558-6