Abstract
Background
During the COVID-19 pandemic, people with Down syndrome (DS) have experienced a more severe disease course and higher mortality rates than the general population. It is not yet known whether people with DS are more susceptible to being diagnosed with COVID-19.
Objective
To explore whether DS is associated with increased susceptibility to COVID-19.
Design
Matched-cohort study design using anonymised primary care electronic health records from the May 2021 release of Clinical Practice Research Datalink (CPRD) Aurum.
Setting
Electronic health records from approximately 1400 general practices (GPs) in England.
Participants
8854 people with DS and 34,724 controls matched for age, gender and GP who were registered on or after the 29th January 2020.
Measurements
The primary outcome was COVID-19 diagnosis between January 2020 and May 2021. Conditional logistic regression models were fitted to estimate associations between DS and COVID-19 diagnosis, adjusting for comorbidities.
Results
Compared to controls, people with DS were more likely to be diagnosed with COVID-19 (7.4% vs 5.6%, p ≤ 0.001, odds ratio (OR) = 1.35; 95% CI = 1.23–1.48). There was a significant interaction between people with DS and a chronic respiratory disease diagnosis excluding asthma and increased odds of a COVID-19 diagnosis (OR = 1.71; 95% CI = 1.20–2.43), whilst adjusting for a number of comorbidities.
Conclusion
Individuals with DS are at increased risk for contracting COVID-19. Those with underlying lung conditions are particularly vulnerable during viral pandemics and should be prioritised for vaccinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The COVID-19 pandemic caused by SARS-CoV-2 infection has disproportionately affected people with intellectual disabilities with increased hospital admissions for severe disease and mortality.1 Down syndrome (DS), caused by trisomy of part or all of chromosome 21, is the most common genetic cause for intellectual disability, with a worldwide prevalence of approximately 1:1000.2 Individuals with DS often present with a range of comorbidities that may increase the risk for developing more severe COVID-19 infection, including congenital heart conditions, a higher prevalence of obesity, respiratory tract infections and sleep apnoea,3,4 and Alzheimer’s disease.5 In addition, it has been proposed that elevated levels of the proinflammatory cytokines IL-6 and TNF-α, and enhanced interferon signalling associated with IFNAR1, IFNAR2 and IFNGR2 overexpression, may increase risk for severe outcomes for COVID-19 by increasing the likelihood of an abnormal cytokine response.6
Some triplicated genes and their knock-on effects in individuals with DS may increase the susceptibility for viral infection, including for SARS-CoV-2. Triplication of TMPRSS2, located on chromosome 21, may enhance viral entry in DS and thus increase the likelihood of infection with SARS-CoV-2 as it interacts with the viral S protein to allow SARS-CoV-2 entry into the host cells.7 Viral diseases that use ACE-2-receptor/TMPRSS2 for cell binding/cell entry include influenza, SARS-CoV-1, metapneumovirus and MERS. Social and behavioural factors, including lower adherence to social distancing and handwashing recommendations, might also contribute to SARS-CoV-2 transmission in DS. Many individuals with DS, and particularly older adults, may be at higher risk for infection due to increased exposure through living in care settings and through contact with rotating care teams.8
Research shows that people with DS are more likely to have severe COVID-19 outcomes, with hospitalisation rates approximately 5 times higher than those of the general population9. Mortality rates are approximately 3 times higher than those of controls even after adjusting for known risk factors for COVID-19 mortality.10 Furthermore, COVID-19 patients with DS present with significantly higher rates of medical complications, particularly lung complications such as pneumonia and acute respiratory distress syndrome.10
Whether DS is associated with increased susceptibility to SARS-CoV-2 infection is unknown but could have important implications for prevention of infection given the increased risk for poor outcomes. We aimed to establish if individuals with DS of all ages were more likely to be diagnosed with COVID-19 compared to age- and gender-matched peers in a population-based cohort study drawing on primary care electronic health records from the UK from January 2020 to May 2021. We aimed to identify comorbidities associated with risk, as well as to explore the potential role of other associated factors such as living situation.
METHODS
Study Population and Data Sources
We conducted a cohort study using anonymised primary care electronic health records from the May 2021 release of Clinical Practice Research Datalink (CPRD) Aurum, which is a population-based database of the electronic health records for approximately 1400 general practices (GPs) in England. CPRD Aurum was made available for research purposes in 2018 and, as of March 2021, consists of data from over 39 million patients with over 13 million currently registered. The database contains data from GPs in England using the EMIS clinical systems and includes data on diagnoses, symptoms, prescriptions, referrals and tests.11,12 Previous studies have confirmed the quality of data from CPRD Aurum.13,14,15 This study protocol was approved by the CPRD Independent Scientific Advisory Committee (ISAC application number 20_099).
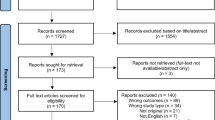
We utilised a matched-cohort study design.16 Patients with DS ever recorded were eligible if they were registered at a GP on or after the 29th of January 2020, the date of the UK’s first confirmed COVID-19 case. DS patients aged 80 and over were excluded as this exceeds the typical life expectancy of individuals with DS.17,18 Up to four control participants without DS were sampled with replacement from the list of all patients registered in May 2021 release of CPRD Aurum. Controls were matched for year of birth, sex and GP and if their start of record was no later than 18 months after that of the matched DS participant. The final cohort comprised 8854 DS patients (4639 males) who were matched to 34,724 controls (18,276 males).
Main Measures
We identified COVID-19 diagnosis using Read codes for confirmed or suspected COVID-19 from patients’ clinical records as reported by CPRD.12 Suspected diagnoses were included because of the limited availability of testing during the first wave of the pandemic. We excluded COVID-19 diagnoses dated before the 29th of January 2020. We evaluated comorbidities from patients’ clinical records using Read codes from the OpenSAFELY study19 and code lists created for DS-specific conditions. These Read code lists were created and then verified by a second reviewer for consensus. If consensus was not met, an external third reviewer with expertise in the area was consulted for their input.
Read codes for the following diagnoses were created: congenital heart disease, dementia, hypothyroidism, other chronic inflammatory conditions/other autoimmune conditions (including rheumatoid arthritis, alopecia and psoriasis), chronic respiratory disease excluding asthma (including chronic obstructive pulmonary disease, pneumonias and cystic fibrosis), asthma, cerebrovascular accident, ischaemic heart disease/peripheral vascular disease, hypertension, other cardiovascular diseases (including conduction and rhythm disorders, cardiomyopathies and valvular disease), chronic liver disease, chronic kidney disease, obesity, diabetes (both type 1 and type 2), epilepsy, anxiety disorders, depression, sleep disorders, cancer (including solid tumours, skin cancers and metastatic disease) and haematological malignancy, as well as for smoking status and living situation (living in residential or care settings).
Statistical Analysis
We fitted conditional logistic regression models to estimate associations between DS and COVID-19 diagnosis, compared to general population controls, reporting odds ratios (OR) with 95% confidence intervals (95% CI). We adjusted for DS-specific and non-specific comorbidities in the models. Interaction analyses were conducted between DS and clinically relevant comorbidities, in this instance, chronic respiratory disease (except asthma), dementia and asthma, to examine how these might impact susceptibility to COVID-19 diagnosis. We fitted conditional logistic regression models to explore the associations between multimorbidity and susceptibility to COVID-19 diagnosis. Multimorbidity was fitted as a factor ranging from 1 to 7 and 8+ comorbidities. Finally, an exploratory logistic regression model was used to examine the potential impact of living situation on susceptibility to COVID-19 diagnosis in a sub-sample of patients with living situation data. In this model, we adjusted for age group, gender and DS-specific and non-specific comorbidities.
RESULTS
We analysed data for the period January 2020 to May 2021 and the cohort comprised 43,578 patients.
Pattern of Infection Rates During the Pandemic
As Fig. 1 shows, the excess of COVID-19 diagnoses in DS individuals was more prominent during the peak periods of the pandemic in April/May 2020 and November/December 2020. The excess rates in people with DS in the second wave of the pandemic occurred despite enhanced awareness of protective measures such as wearing masks and limiting social contacts, suggesting that either these measures were not sufficient to protect this high-risk group or otherwise were not consistently applied.
Table 1 shows the demographic characteristics and comorbidities of DS cases and general population controls according to COVID-19 diagnosis. As expected, a higher proportion of people with DS were diagnosed with COVID-19 compared to controls (7.4% vs 5.6%, p ≤ 0.001).
In the DS group, people diagnosed with COVID-19 had higher rates of anxiety disorders, other chronic inflammatory conditions/other autoimmune conditions, cerebrovascular accidents, dementia, depression, diabetes (both type 1 and type 2), epilepsy, hypothyroidism, obesity, sleep disorders, asthma, chronic liver disease, chronic kidney disease and chronic respiratory disease compared to people with DS without a COVID-19 diagnosis. For controls, those with a COVID-19 diagnosis had higher rates of congenital heart disease, anxiety disorders, other chronic inflammatory conditions/other autoimmune conditions, depression, diabetes (both type 1 and type 2), hypertension, hypothyroidism, obesity, other cardiovascular diseases, sleep disorders, smoking, asthma and chronic respiratory disease compared to those without COVID-19.
Unadjusted for comorbidities listed in Table 1, we found that DS cases had an increased likelihood of receiving a COVID-19 diagnosis compared to controls (Table 2). In a model adjusted for comorbidities, COVID-19 diagnosis was most strongly associated with dementia (OR = 2.75, 95% CI 2.03–3.72), chronic respiratory disease excluding asthma, epilepsy, hypertension, asthma, depression, anxiety disorders and other chronic inflammatory conditions/other autoimmune conditions explaining increased susceptibility of COVID-19 diagnosis. DS was not independently associated with COVID-19 after adjusting for comorbidities.
Interactions Between Comorbidities and Susceptibility to COVID-19 Diagnosis
Comorbidities from our previous models were chosen based on their clinical relevance; these included chronic respiratory disease, asthma and dementia. We found evidence that the association of DS with COVID-19 varied by chronic respiratory disease status. People with DS who had a chronic respiratory disease were more susceptible to being diagnosed with COVID-19, OR = 1.71 (95% CI 1.20–2.43), p = 0.003. Interactions with asthma (p = 0.28) and dementia (p = 0.36) diagnosis did not improve goodness of fit.
Risk Associated with Multimorbidity
As Table 3 shows, multimorbidity was associated with increased susceptibility to a COVID-19 diagnosis compared to having no comorbidities. Adjusting for multimorbidity, people with DS were still more likely to receive a COVID-19 diagnosis compared to controls.
Impact of Living Situation on Susceptibility to COVID-19
To examine the effect of living situation on the DS and chronic respiratory disease diagnosis interaction, we fitted a standard logistic regression on a sub-sample of 4528 patients (10.4% of total sample) who had data on their living situation. Living situation data was coded as per the OpenSAFELY study20 comparing those living in residential or care settings with those in other living situations (living with relatives etc.).
When adjusting for the impact of living in residential or care settings, the DS and chronic respiratory disease diagnosis interaction was not significant, OR = 1.83 (95% CI 0.86–4.28), p = 0.14. In this model, age groups 50–59 (OR = 4.32; 95% CI 1.30–26.80; p = 0.04); 60–59 (OR = 4.70; 95% CI 1.38–29.49; p = 0.04) and 70–79 (OR = 5.02; 95% CI 1.29–33.37; p = 0.04), epilepsy (OR = 1.46; 95% CI 1.14–1.84; p = 0.002) and living in residential or care settings (OR = 1.60; 95% CI 1.27–2.01; p < 0.0001) were associated with increased likelihood of a COVID-19 diagnosis.
DISCUSSION
This analysis of large-scale population-level UK primary care data identified that people with DS had a significantly increased likelihood of receiving a COVID-19 diagnosis compared to controls (OR = 1.35; 95% CI 1.23–1.48), and this was not entirely explained by multimorbidity. We found that susceptibility to COVID-19 diagnosis across the cohort was associated with specific comorbidities including anxiety disorders, other chronic inflammatory conditions/other autoimmune conditions, dementia, depression, epilepsy, hypertension, asthma and chronic respiratory disease excluding asthma. In particular, people with DS and a chronic respiratory disease diagnosis were significantly more susceptible to COVID-19 (OR = 1.71; 95% CI 1.20–2.43). However, this did not remain significant when controlling for exposure through living situation in a smaller sub-sample of patients with data available on living situation.
Our findings of an interaction between chronic respiratory conditions in DS and risk of COVID-19 diagnosis may indicate a common mechanism for increased risk for respiratory conditions in general in DS individuals, or alternatively that existing respiratory vulnerability (excluding asthma) may be associated with increased susceptibility to infection with SARS-CoV-2. DS is associated with certain anatomical differences, facial and airway tract features that may increase risk for respiratory infections, such as macroglossia, a narrow nasopharynx and a shortened palate, further complicated by generalised hypotonia.21 These may be associated with increased risk for ear, nose and throat infections22 and obstructive sleep apnoea.23 Furthermore, a higher prevalence of congenital cardiac anomalies and pulmonary hypertension24 may further increase the risk for respiratory infections in people with DS.
Ultimately, respiratory infections are a significant source of increased morbidity and mortality in children and adults with DS.25 Approximately 40% of children and young adults (aged < 30 years) with DS experience at least one episode of pneumonia.26 Pneumonia was associated with higher risk of inpatient mortality when adjusting for age, gender and ethnicity for adults with DS compared to controls using data from the UK.27
Type 1 interferons (IFNs) help to regulate the activity of the immune system. Trisomy 21 is characterised by enhanced IFN-1 signalling due to overexpression of IFN genes on chromosome 21 (IFNAR1, IFNAR2 and IFNGR2). The effect on respiratory infections are difficult to predict, though may have both positive and negative effects by enhancing anti-viral response and overactivation of the immune system with risk for a cytokine storm.7 Individuals with DS may also have reduced lymphocyte numbers.28 Immune dysregulation has been proposed to be a syndromic feature,29 and the cell-mediated immunodeficiency combined with impaired antibody response to pathogens may explain the increased risk for and mortality associated with pneumonia and other respiratory diseases in children with DS.
Given the biological risk associated with increased viral entry, individuals with DS may also have a particular predisposition for viral respiratory infections in general, rather than specifically for SARS-CoV-2. TMPRSS2 belongs to the type II transmembrane serine protease family and is commonly expressed in epithelial tissues such as those lining the upper airways, bronchi and lung.30,31 Influenza viruses and other coronaviruses all critically depend on TMPRSS2 for viral activation and cellular infection.31,32 Viruses such as influenza virus, respiratory syncytial virus (RSV) and parainfluenza virus likely account for most of the respiratory infections in DS,22,33 and those with congenital cardiac conditions or pulmonary hypertension may be particularly vulnerable.
Obesity is a common comorbidity in DS, and associated with increased disease severity when diagnosed with COVID-19 in the general population, probably through its association with decreased lung reserve volume and capacity, as well as reduced pulmonary function in bed-bound patients. Obesity is also associated with higher levels of inflammatory cytokines, which may contribute to higher mortality rates in obese individuals with COVID-19.34 In the present study, obesity was not associated with increased susceptibility to COVID-19 when adjusting for other comorbidities. This suggests that the increased risk associated with obesity may be related to complications and treatment outcomes rather than susceptibility to infection. Additionally, congenital heart disease may be associated with higher risk for hospitalisation in those with COVID-19 infection,10 but although 35% of DS participants had a diagnosis of congenital heart conditions in our study, it was not associated with increased susceptibility to infection.
Our data and other research suggest that individuals with DS are particularly at risk for COVID-19 and other respiratory infections. Our data further emphasises the need to prioritise individuals with DS for COVID-19 vaccination. They should also be prioritised for surveillance of respiratory infections during high-risk periods,35 and for implementing additional safety measures during pandemics. This may include preventing and rapidly containing transmission in long-term care facilities, providing support to caregivers on close monitoring and safe care, and identification of symptoms that may indicate the need for assessment for admission to hospital. Active medical management to ensure access to oxygen therapy and drugs such as steroids and antibiotics when needed could prevent complications and hospital admissions. There may also be a rationale for offering pneumococcal vaccine in addition to flu vaccine to children and adults with DS. Other preventative measures include management of comorbidities such as obesity and treatment of sleep apnoea.36 Future studies on the contribution of TMPRSS2 triplication and developing therapies that may be particularly relevant to DS are needed.
This is the largest study to date of COVID-19 in individuals with DS, including nearly 9000 DS individuals, of whom 651 were diagnosed with COVID-19. We included data from the whole of 2020 and part of 2021, thus covering the initial and subsequent waves of the pandemic in the UK. Nevertheless, differential access to testing might have been a potential source of bias due to limited access to tests during the first wave of the pandemic.37 Whilst the probability of an infected person receiving a test might have been variable over time, it is unlikely to account for differences in rates between individuals with DS and general population controls since it affected all patients and GPs across the UK. It is possible that those with symptomatic infections were more likely to be tested and recorded with an infection by their primary care physicians than asymptomatic cases. Whether people with DS are less likely to experience asymptomatic infections is currently unknown. Our exploratory sub-analysis examining the impact of living situation on COVID-19 diagnosis found that living in residential or care settings may increase the likelihood of COVID-19 diagnosis. This finding is consistent with the excess mortality and infection rates reported in the UK38 and internationally39 for those living in residential or care settings. Whilst living situation was an important risk factor for COVID-19 diagnosis, this analysis was only conducted in 10% of the total sample with living situation data available and only 2.3% (800/34,724) of controls had data on this variable. Therefore, the interaction between living situation and chronic respiratory disease in those with DS could not be fully examined, and future studies with better recording of living situation data are needed. Further, it is not yet clear how multimorbidity and health-seeking behaviours may have influenced COVID-19 diagnosis. Multimorbidity is associated with increased primary care use40 which may have increased the likelihood of patients consulting with their GP for COVID-19 symptoms. Therefore, the relationship between COVID-19 diagnosis and multimorbidity warrants further investigation.
Individuals with DS have both increased susceptibility to COVID-19 infection and are more likely to experience severe outcomes. Susceptibility to COVID-19 is increased during peaks of the pandemic and associated with health comorbidities in individuals with DS, particularly chronic respiratory conditions. Although lockdowns and the associated measures to wear masks and social distancing appeared to have an effect in reducing the initial wave of the pandemic, it did not seem to prevent excess infections in DS individuals during the 2nd wave in the autumn winter of 2020, suggesting that these measures were not fully utilised for this group, or else that additional safeguards may be required. This has important public health implications to manage risk during the ongoing SARS-CoV-2 pandemic, as well as to manage the risk associated with respiratory infections in people with DS. Individuals with DS who have underlying lung conditions should take extra care to safeguard themselves during viral pandemics, and our findings suggest a strong rationale for them to be prioritised for vaccination with COVID-19, influenza and pneumococcal vaccines.
Data Availability:
Data are available upon reasonable request. Requests for access to data from the study should be addressed to martin.gulliford@kcl.ac.uk. All proposals requesting data access will need to specify planned uses with approval of the study team and CPRD before data release.
References
Williamson EJ, McDonald HI, Bhaskaran K, et al. Risks of covid-19 hospital admission and death for people with learning disability: population based cohort study using the OpenSAFELY platform. bmj 2021;374:n1592.
Antonarakis SE, Skotko BG, Rafii MS, et al. Down syndrome. Nat Rev Dis Primers 2020;6:9.
Maris M, Verhulst S, Wojciechowski M, Van de Heyning P, Boudewyns A. Prevalence of obstructive sleep apnea in children with Down syndrome. Sleep 2016;39:699-704.
Startin CM, D’Souza H, Ball G, et al. Health comorbidities and cognitive abilities across the lifespan in Down syndrome. Journal of neurodevelopmental disorders 2020;12:1-13.
Sinai A, Bohnen I, Strydom A. Older adults with intellectual disability. Current opinion in psychiatry 2012;25:359-64.
Illouz T, Biragyn A, Frenkel-Morgenstern M, et al. Specific Susceptibility to COVID-19 in Adults with Down Syndrome. Neuromolecular medicine 2021:1-11.
De Toma I, Dierssen M. Network analysis of Down syndrome and SARS-CoV-2 identifies risk and protective factors for COVID-19. Scientific Reports 2021;11:1930.
Strydom A, Corcoran E, Rebillat A-S. The COVID-19 pandemic should be last orders for poor care of people with neurodevelopmental disorders. The British Journal of Psychiatry 2021;218:302-4.
Clift AK, Coupland CA, Keogh RH, Hemingway H, Hippisley-Cox J. COVID-19 mortality risk in Down syndrome: results from a cohort study of 8 million adults. Annals of internal medicine 2020.
Hüls A, Costa AC, Dierssen M, et al. Medical vulnerability of individuals with Down syndrome to severe COVID-19–data from the Trisomy 21 Research Society and the UK ISARIC4C survey. EClinicalMedicine 2021;33:100769.
Wolf A, Dedman D, Campbell J, et al. Data resource profile: clinical practice research Datalink (CPRD) aurum. International journal of epidemiology 2019;48:1740-g.
Data highlights. 2021. (Accessed 14 April 2021, at https://www.cprd.com/data-highlights.)
Gulliford MC, Sun X, Anjuman T, Yelland E, Murray-Thomas T. Comparison of antibiotic prescribing records in two UK primary care electronic health record systems: cohort study using CPRD GOLD and CPRD Aurum databases. BMJ Open 2020;10:e038767.
Jick SS, Hagberg KW, Persson R, et al. Quality and completeness of diagnoses recorded in the new CPRD Aurum Database: evaluation of pulmonary embolism. Pharmacoepidemiology and Drug Safety 2020;29:1134-40.
Persson R, Vasilakis-Scaramozza C, Hagberg KW, et al. CPRD Aurum database: Assessment of data quality and completeness of three important comorbidities. Pharmacoepidemiology and Drug Safety 2020;29:1456-64.
Cummings P, McKnight B, Greenland S. Matched cohort methods for injury research. Epidemiologic reviews 2003;25:43-50.
Bittles A, Glasson E. Clinical, social, and ethical implications of changing life expectancy in Down syndrome. Developmental medicine and child neurology 2004;46:282-6.
Glasson EJ, Jacques A, Wong K, Bourke J, Leonard H. Improved survival in Down syndrome over the last 60 years and the impact of perinatal factors in recent decades. The Journal of pediatrics 2016;169:214-20. e1.
Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584:430-6.
NHS England Care Homes residential status. 2021. (Accessed 01/06/2021, 2021
Kanamori G, Witter M, Brown J, Williams-Smith L. Otolaryngologic manifestations of Down syndrome. Otolaryngologic Clinics of North America 2000;33:1285-92.
Verstegen RH, van Hout RW, de Vries E. Epidemiology of respiratory symptoms in children with Down syndrome: a nationwide prospective web-based parent-reported study. BMC pediatrics 2014;14:1-5.
Horne RS, Wijayaratne P, Nixon GM, Walter LM. Sleep and sleep disordered breathing in children with down syndrome: Effects on behaviour, neurocognition and the cardiovascular system. Sleep medicine reviews 2019;44:1-11.
Bush D, Galambos C, Dunbar Ivy D. Pulmonary hypertension in children with Down syndrome. Pediatric pulmonology 2021;56:621-9.
Illouz T, Biragyn A, Iulita MF, et al. Immune Dysregulation and the Increased Risk of Complications and Mortality Following Respiratory Tract Infections in Adults With Down Syndrome. Frontiers in immunology 2021;12:2375.
Määttä T, Määttä J, Tervo-Määttä T, Taanila A, Kaski M, Iivanainen M. Healthcare and guidelines: a population-based survey of recorded medical problems and health surveillance for people with Down syndrome. Journal of Intellectual and Developmental Disability 2011;36:118-26.
Uppal H, Chandran S, Potluri R. Risk factors for mortality in Down syndrome. Journal of Intellectual Disability Research 2015;59:873-81.
MacLean GA, McEldoon J, Huang J, Allred J, Canver MC, Orkin SH. Downregulation of endothelin receptor B contributes to defective B cell lymphopoiesis in trisomy 21 pluripotent stem cells. Scientific reports 2018;8:1-10.
Huggard D, McGrane F, Lagan N, et al. Altered endotoxin responsiveness in healthy children with Down syndrome. BMC immunology 2018;19:1-10.
Bugge TH, Antalis TM, Wu Q. Type II transmembrane serine proteases. Journal of Biological Chemistry 2009;284:23177-81.
Iwata-Yoshikawa N, Okamura T, Shimizu Y, Hasegawa H, Takeda M, Nagata N. TMPRSS2 contributes to virus spread and immunopathology in the airways of murine models after coronavirus infection. Journal of virology 2019;93:e01815-18.
Stopsack KH, Mucci LA, Antonarakis ES, Nelson PS, Kantoff PW. TMPRSS2 and COVID-19: serendipity or opportunity for intervention? Cancer discovery 2020;10:779-82.
Chan M, Park JJ, Shi T, et al. The burden of respiratory syncytial virus (RSV) associated acute lower respiratory infections in children with Down syndrome: A systematic review and meta–analysis. Journal of global health 2017;7.
Dietz W, Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity (Silver Spring) 2020;28:1005.
Santoro SL, Chicoine B, Jasien JM, et al. Pneumonia and respiratory infections in Down syndrome: A scoping review of the literature. American Journal of Medical Genetics Part A 2021;185:286-99.
Trucco F, Chatwin M, Semple T, Rosenthal M, Bush A, Tan HL. Sleep disordered breathing and ventilatory support in children with Down syndrome. Pediatric pulmonology 2018;53:1414-21.
Griffith GJ, Morris TT, Tudball MJ, et al. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nature communications 2020;11:1-12.
Graham NS, Junghans C, Downes R, et al. SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes. Journal of Infection 2020;81:411-9.
Comas-Herrera A, Zalakaín J, Lemmon E, et al. Mortality associated with COVID-19 in care homes: international evidence. Article in LTCcovid org, international long-term care policy network, CPEC-LSE 2020;14.
Soley-Bori M, Ashworth M, Bisquera A, et al. Impact of multimorbidity on healthcare costs and utilisation: a systematic review of the UK literature. British Journal of General Practice 2021;71:e39-e46.
Funding
This study was supported by grants from the MRC (MR/S011277/1; MR/S005145/1; MR/R024901/1), the European Commission (H2020 SC1 Gene overdosage and comorbidities during the early lifetime in Down Syndrome GO-DS21- 848077) and Alzheimer’s Society (AS-CP-18-0020: fellowship to SP).
This study represents independent research partly funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
AS and MCG conceived and designed the project. AS, MCG and RAB planned the data analysis. RAB conducted the data analysis with help from MCG. All authors reviewed and contributed to the final draft.
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baksh, R.A., Strydom, A., Pape, S.E. et al. Susceptibility to COVID-19 Diagnosis in People with Down Syndrome Compared to the General Population: Matched-Cohort Study Using Primary Care Electronic Records in the UK. J GEN INTERN MED 37, 2009–2015 (2022). https://doi.org/10.1007/s11606-022-07420-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07420-9