Abstract
Background
Cross-sectional studies have found that health-related quality of life and mental health are worse among food-insecure compared with food-secure individuals. However, how these outcomes change as food insecurity changes is unclear.
Objective
To evaluate how common patient-reported health-related quality of life and mental health scales change in response to changes in food security.
Design
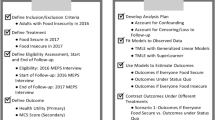
Retrospective cohort study using data representative of the civilian, adult, non-institutionalized population of the USA.
Participants
Food insecure adults who completed the 2016–2017 Medical Expenditure Panel Survey.
Main Measures
Mental health, as measured by the mental component score of the Veterans Rand 12-Item Health Survey (VR-12) (primary outcome), along physical health (physical component score of the VR-12), self-rated health status, psychological distress (Kessler 6), depressive symptoms (PHQ2), and the SF-6D measure of health utility. We fit linear regression models adjusted for baseline outcome level, age, gender, race/ethnicity, education, health insurance, and family size followed by predictive margins to estimate the change in outcome associated with a 1-point improvement in food security.
Key Results
A total of 1,390 food-insecure adults were included. A 1-point improvement in food security was associated with a 0.38 (95%CI 0.62 to 0.14)-point improvement in mental health, a 0.15 (95%CI 0.02 to 0.27)-point improvement in psychological distress, a 0.05 (95%CI 0.01 to 0.09)-point improvement in depressive symptoms, and a 0.003 (95%CI 0.000 to 0.007)-point improvement in health utility. Point estimates for physical health and self-rated health were in the direction of improvement, but were not statistically significant.
Conclusions
Improvement in food insecurity was associated with improvement in several patient-reported outcomes. Further work should investigate whether similar changes are seen in food insecurity interventions, and the most useful scales for assessing changes in health-related quality of life and mental health in food insecurity interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Food insecurity—insufficient or uncertain access at all times to enough food for an active healthy life—affected American households encompassing over 38 million people in 2020.1 Food insecurity is associated with a number of poor health outcomes, including increased hemoglobin A1c for people with diabetes, increased incidence of chronic kidney disease, greater number of emergency department visits, and greater healthcare expenditures.2,3,4,5,6,7,8,9 For these reasons, food insecurity is increasingly targeted by interventions meant to address health-related social needs in order to improve health.10, 11 To date, food insecurity interventions have often aimed at reducing healthcare utilization and cost, or improving biomarkers of disease control, such as hemoglobin A1c.12,13,14
Another aspect of health that food insecurity may affect is patient-reported outcomes, particularly with regard to well-being, health-related quality of life, and mental health.15, 16 Both cross-sectional quantitative research and qualitative research have examined associations between food insecurity, health-related quality of life, and mental health.17,18,19,20,21,22,23,24,25 Despite clear differences in health-related quality of life and mental health between people who do and do not experience food insecurity, it is unclear to what extent these outcomes change when food insecurity changes. Answering this question is critical for understanding the impact on health that food insecurity interventions could have. Therefore, we sought to examine changes in patient-reported outcome measures associated with changes in food security in a nationally representative cohort. Based on a previously published conceptual model26, we hypothesized that mental health outcomes, particularly mental health-related quality of life, would improve as food insecurity improved.
METHODS
Data Source and Setting
This study used data from Panel 21 of the Medical Expenditure Panel Survey (MEPS).27 MEPS is a nationally representative probability sample of the civilian non-institutionalized population of the USA, conducted by the Agency for Healthcare Research and Quality (AHRQ).27 MEPS participants are drawn from participants in the National Health Interview Survey and complete five interviews over a 2-year period. Panel 21 completed their interviews in 2016 and 2017, and is the only MEPS panel, to date, to have completed food insecurity assessment at two time points. For this study, we used the MEPS longitudinal data file and the food security files for Panel 21.
The institutional review board at the UNC determined that this secondary use of de-identified data was not human subjects research.
Food Insecurity
Food insecurity in MEPS was assessed using the 10-item USDA Adult Food Security Survey Module, with a 30-day lookback period.28 MEPS participants completed food insecurity assessment in both 2016 and 2017. The food security survey module has excellent reliability (Cronbach’s α > 0.85)29, 30 and was scored in the standard fashion.28, 31 Scoring instructions state: “Responses of “yes,” “often,” “sometimes,” “almost every month,” and “some months but not every month” are coded as affirmative. The sum of affirmative responses to the 10 questions in the Adult Food Security Scale is the household’s raw score on the scale.”28 This produces a raw score (range: 0 to 10), with higher scores indicating worse food insecurity. The food security survey module was developed using a Rasch model, which supports an interval interpretation of the score.32, 33
The primary exposure for this study was the change in food insecurity between 2016 and 2017. This was calculated by taking a respondent’s 2017 food security raw score and subtracting from it their 2016 food security raw score. In constructing the exposure in this way, a negative-valued score indicates that food insecurity has improved, a score of 0 indicates no change, and a positive-valued score indicates food insecurity has worsened.
Patient-Reported Outcome Measures
We used several patient-reported outcome measures in this study. The primary outcome was the mental component score (MCS) derived from the Veterans Rand 12-Item Health Survey (VR-12), measured in 2017. The VR-12 is a generic health-related quality of life instrument that is similar to the 12-item Short Form Survey version 2 (SF-12v2).34, 35 The MCS score uses data from all 12 VR-12 items, weighting more heavily mental health components in its scoring algorithm. We selected the MCS as the primary outcome given prior empirical evidence and conceptual models that suggest changes in food insecurity may particularly affect mental health.19, 23, 26, 36, 37 The MCS scoring algorithm is designed to have a mean of 50 and a standard deviation of 10 in the US population. Higher scores indicate better mental health.
We used several other patient-reported outcome measures (all assessed in 2017) as secondary outcomes. These were the following: the physical component score (PCS) from the VR-12 (which also uses all 12 items, has a mean of 50, standard deviation of 10, and higher scores indicate better physical health)34, 35, 1-item self-rated health (scored as 1=excellent, 2=very good, 3=good, 4=fair, or 5=poor)38, the Kessler 6 (K6) measure of non-specific psychological distress (range 0–24 with higher scores indicating more distress)39, the Patient Health Questionnaire 2-item (PHQ2) measure of depressive symptoms (range: 0–6 with higher scores indicating more depressive symptoms)40, and the SF-6D (Short Form – Six Dimension) measure of health utility (range 0.345 to 1, with higher scores indicating better health utility).41, 42 Health utility is a summary score that relates a health state to a general population’s preferences about health-related quality of life. Health utility measures are constructed such that “dead” is anchored at 0 and “full health” is anchored at 1.
Scoring Baseline Outcomes
For the self-rated health, K6, and PHQ2 outcomes, these were collected identically in 2016 and 2017. For the MCS and PCS scores, in 2016, MEPS administered the SF-12v2 rather than the VR-12.43 MCS and PCS scores can be calculated from both the SF-12v2 and VR-12, and in releasing data, AHRQ explicitly used a scoring algorithm to help ensure that the 2016 and 2017 MCS and PCS scores were aligned with each other.44 Similarly, the SF-12v2 and the VR-12 each contain the 7 questions used in the SF-6D valuation set and scoring algorithm. To ensure consistency across years, we applied the same scoring algorithm to each questionnaire to calculate the SF-6D score.42
Covariates
We extracted data from MEPS on several covariates that may confound the relationship between changes in food insecurity and patient-reported outcome measures. For sociodemographic factors, these were age in years at the start of MEPS, gender, educational attainment (categorized as less than high school diploma, high school diploma, or greater than high school diploma), household size (as household size has previously been related to different experiences of food insecurity), and 2016 health insurance (categorized as uninsured, private insurance, Medicare insurance including dual eligible, and other public health insurance). As possible indicators for the experience of racism, which may affect both change in food insecurity and study outcomes, we included a race/ethnicity variable, categorized as Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and non-Hispanic Multiple Race or Other. These were the most detailed categorizations feasible with the available sample size. Finally, analyses were adjusted for the baseline (2016) versions of the patient-reported outcome measures, which helps account for reverse causation (that is, baseline levels of the outcome affecting food insecurity).
Analytic Samples
Our aim was to examine, from the perspective of conducting a food insecurity intervention, how changes in food insecurity are associated with changes in self-reported health outcomes. Therefore, we sought to include individuals who reported food insecurity at baseline (as might enroll in a food insecurity intervention). Thus, the primary analytic sample included adults (aged 18 years or older) categorized as food insecure at baseline (2016 food security raw score > 2) alive for complete follow-up in 2017.
We constructed three additional samples to examine other aspects of our research questions. First, we constructed a cross-sectional analytic sample to compare patient-reported outcomes between those who were food secure and food insecure in 2016. This sample consisted of all adults (age ≥ 18 years). We also considered different ways of classifying who might be eligible for a food insecurity intervention. For sensitivity analyses, we created a sample with food insecure and marginally food secure participants (2016 food secure raw score > 0)28, and a Hunger Vital Sign45 sample (affirmative responses to either [or both] of the first two items from the 2016 adult food security survey module, which correspond to screening positive on the Hunger Vital Sign screening instrument).45
Statistical Analysis
We first conducted descriptive statistics. Next, we sought to better understand the appropriate functional form with which to model the relationship between change in food security score and study outcomes. Analyses used to do this and their results are described in more detail in the Technical Appendix (including eTable 1 and eFigures 1–6). Ultimately, we concluded that a linear relationship was a reasonable approximation, although we included other functional forms as part of sensitivity analyses as described below.
The next step was to conduct regression analyses that use representativeness weights and design-corrected standard errors, in order to assess whether changes in food insecurity were statistically significantly associated with changes in study outcomes. These models adjusted for age, gender, race/ethnicity, education, household size, and the 2016 measurement of the outcome. By including the 2016 version of the outcome, this has the effect of adjusting for time-invariant confounding from both unmeasured and measured factors that would affect the outcome in both 2016 and 2017. Because food insecurity interventions often reduce food insecurity by increasing income, we did not want to adjust for income as that would produce estimates of changes in study outcome independent of the income pathway. In other words, we were not interested in estimating how changes in food insecurity might relate to study outcomes independent of income. Results from these models should not be interpreted as estimating the causal effect of a change in food insecurity alone on study outcomes. Instead, they should be interpreted as estimates of how changes in food insecurity (which may occur for multiple reasons) are associated with changes in study outcomes.
As noted above, our primary models were fit using linear regression. As an additional check on functional form, we re-fit each of the models using Poisson regression. Finally, for two outcome scales that contain only a small number of possible values (self-rated health status and PHQ2 score), we fit generalized ordered logistic regression models as an additional sensitivity analysis.46 These models estimate the probability of transitioning from one level to a higher level, but do not impose a proportional odds assumption as a standard ordinal logistic model does. This means, for example, that a 1-point change in food security score could have a different association with the probability of moving from “good” to “excellent” health than it does with the probability of moving from “poor” to “fair” health.
After fitting these models, we used predictive margins47 to estimate change in each outcome per 1- and 5-point improvement in food security score, standardized over the distribution of model covariates. A two-sided p-value of < 0.05 indicated statistical significance. Analyses were conducted in SAS version 9.4 and Stata/MP Version 16.1.
RESULTS
There were 1,397 adults who reported food insecurity in 2016. Of these, 7 (0.5%) were excluded due to incomplete follow-up, yielding a primary analytic sample of 1,390 individuals. Demographic characteristics of the primary analytic sample are presented in Table 1. The mean change in food security score from 2016 to 2017 was −2.49 (SE 0.14, min: −10, max: 5; Figure 1).
Demographics for the additional analytic samples are presented as eTables 2 and 3. Comparing those who were food secure and food insecure in 2016, those who were food insecure had significantly worse scores for all study outcomes in both unadjusted and adjusted analyses (eTable 4).
In linear regression models that incorporated representativeness weights and used survey design-corrected standard errors, we found that decreases in food insecurity were associated with significant improvement in MCS, K6 score, PHQ2 score, and SF-6D score (Table 2, full models in eTables 5–10). A 1-point improvement in food security was associated with a 0.38 (95%CI 0.62 to 0.14)-point improvement in MCS score, a 0.15 (95%CI 0.02 to 0.27)-point improvement in K6 score, a 0.05 (95%CI 0.01 to 0.09)-point improvement in PHQ2 score, and a 0.003 (95%CI 0.000 to 0.007)-point improvement in SF-6D score. Point estimates for PCS and self-rated health were in the direction of improvement, but were not statistically significant. Plots of the relationship between change in food security score and study outcomes are presented as eFigures 7–12.
Results from Poisson regression models were very similar to the results of linear regression models (eTable 11). Results were also similar in sensitivity analyses examining different analytic samples (eTables 12–13). For the two outcomes with restricted scales (self-rated health and PHQ2), generalized ordinal logistic regression models yielded results very similar to those in the main linear regression analyses (eTables 14–15 and eFigures 13–14).
DISCUSSION
In this cohort study of US nationally representative non-institutionalized adults, we found that improvements in food insecurity were associated with statistically significant improvements in MCS, psychological distress, depressive symptoms, and health utility. Further, in cross-sectional analyses, being food insecure, compared with being food secure, was associated with significantly worse indicators of health-related quality of life, mental health, and health utility. However, the improvements in outcomes seen with changes in food insecurity, albeit over a short timeframe, were small in magnitude relative to the differences between those who were food insecure and food secure in cross-sectional analyses.
Improvements in food insecurity were associated with improvements for most study outcomes. However, the magnitude of this change was often small. There are several possible explanations for this finding. First, it may be that food insecurity is a marker of poor well-being, but is not directly related to it. While certainly possible, existing qualitative research argues against this. Studies of individuals who have experienced food insecurity consistently find both that food insecurity is highly aversive and that its alleviation brings great relief.23, 24, 37, 48, 49. Alternatively, the instruments used in this study may not be very responsive to the ways in which alleviation of food insecurity improves health-related quality of life and/or mental health. This could indicate the need to develop new patient-reported outcome measures that are better attuned to the ways in which alleviating food insecurity improves health-related quality of life and mental health. Clarifying which of these explanations is most likely is an important goal for future research. Another important goal of future research is examining whether the experience of racism moderates the relationship between food insecurity and study outcomes.
When food insecurity improved, we did not observe statistically significant improvements in PCS and self-rated health. This may be because changes in food insecurity do not improve physical health. Alternatively, this may represent use of instruments that were relatively unresponsive50, 51, or that emphasized items (such as climbing flights of stairs) not closely connected to the ways in which changes in food insecurity may affect health-related quality of life.35
This study is consistent with prior studies and expands our knowledge in important ways. First, prior cross-sectional studies have found associations between food insecurity, worse mental health, and worse health-related quality of life.17,18,19,20,21,22,23,24,25 Second, as noted above, qualitative studies have supported the idea that food insecurity alleviation is experienced as an important improvement in mental health.23, 24, 37, 48, 49 This study adds quantitative evidence in a US nationally representative sample regarding changes in commonly used indicators of health-related quality of life and mental health associated with changes in food insecurity. Importantly, a prior study comparing different health-related quality of life indicators did find that different instruments were variably suited to measuring differences between those who were experiencing food insecurity and those who were food secure.22
The findings of this study have important implications for food insecurity research. In addition to the need to resolve questions of the magnitude of benefit in the domains that food insecurity interventions may offer, it is important to note that there does not seem to be a clearly “best” instrument to use when measuring health-related quality of life or mental health in food insecurity interventions. This suggests that, presently, investigators should think broadly about what aspects of these concepts might be affected by food insecurity alleviation, and select a wide array of instruments, possibly with overlap, to enhance the chance of identifying important changes.
The results of this study should be interpreted in the context of important limitations. First, because we do not have information on why food security scores changed between baseline and follow-up, we should not interpret changes in study outcomes associated with changes in food security scores causally. There may have been residual confounding that explains the covariation between food security scores and study outcomes. However, we did adjust for a robust set of potential confounders, including the baseline version of the study outcome, which provides protection against time-invariant confounding and reverse causation by baseline levels of the study outcome. Nevertheless, the possibility of time-varying confounding cannot be excluded. Next, we had scores for only a small set of instruments. There are other instruments that focus on domains more greatly affected by food insecurity, such as the ability to participate in social roles, or stress. It would have been desirable to include these had data been available. Next, it is not clear what reduction in food insecurity scores a food insecurity intervention typically achieves. These limitations were balanced by several strengths. First, the included measures covered a broad range of domains, including both mental and physical health-related quality of life, psychological distress, depressive symptoms, and health utility. Next, the use of nationally representative longitudinal data is an important advance relative to prior quantitative work in this area.
Food insecurity is an important threat to health in a number of ways, including cardiometabolic risk, health-related quality of life, and mental health. It is clear that measuring a broad range of outcomes is needed to fully assess the potential benefits of food insecurity interventions. Given the important role that food insecurity plays in both health overall and health inequity more specifically, improving our ability to address food insecurity and understand the effect of doing so on health is imperative.
References
Coleman-Jensen A, Rabbitt MP, Gregory C A, Singh A. Household Food Security in the United States in 2020. Accessed October 5, 2021. http://www.ers.usda.gov/publications/pub-details/?pubid=102075
Gundersen C, Ziliak JP. Food Insecurity And Health Outcomes. Health Aff Proj Hope. 2015;34(11):1830-1839. https://doi.org/10.1377/hlthaff.2015.0645
Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093-3099. https://doi.org/10.2337/dc13-0570
Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238. https://doi.org/10.2337/dc11-1627
Crews DC, Kuczmarski MF, Grubbs V, et al. Effect of food insecurity on chronic kidney disease in lower-income Americans. Am J Nephrol. 2014;39(1):27-3510.1159/000357595
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
Dean EB, French MT, Mortensen K. Food insecurity, health care utilization, and health care expenditures. Health Serv Res. 2020;55(S2):883-893. https://doi.org/10.1111/1475-6773.13283
Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011-2013. Health Serv Res. Published online June 13, 2017. https://doi.org/10.1111/1475-6773.12730
Johnson KT, Palakshappa D, Basu S, Seligman H, Berkowitz SA. Examining the bidirectional relationship between food insecurity and healthcare spending. Health Serv Res. Published online February 17, 2021. https://doi.org/10.1111/1475-6773.13641
Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities--Addressing Social Needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. https://doi.org/10.1056/NEJMp1512532
Bibbins-Domingo K. Integrating Social Care Into the Delivery of Health Care. JAMA. Published online September 25, 2019. https://doi.org/10.1001/jama.2019.15603
Seligman HK, Smith M, Rosenmoss S, Marshall MB, Waxman E. Comprehensive Diabetes Self-Management Support From Food Banks: A Randomized Controlled Trial. Am J Public Health. Published online July 19, 2018:e1-e8. https://doi.org/10.2105/AJPH.2018.304528
Verma S. CMS Approves North Carolina’s Innovative Medicaid Demonstration To Help Improve Health Outcomes. Published October 1, 2018. . https://www.healthaffairs.org/do/10.1377/hblog20181024.406020/full/
Massachusetts Delivery System Reform Incentive Payment Program | Mass.gov. Accessed July 15, 2021. https://www.mass.gov/info-details/massachusetts-delivery-system-reform-incentive-payment-program
Baicker K, Allen HL, Wright BJ, Taubman SL, Finkelstein AN. The Effect of Medicaid on Management of Depression: Evidence From the Oregon Health Insurance Experiment. Milbank Q. 2018;96(1):29-56. https://doi.org/10.1111/1468-0009.12311
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science. 2020;370(6522). https://doi.org/10.1126/science.aay0214
Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household Food Insecurity Is Positively Associated with Depression among Low-Income Supplemental Nutrition Assistance Program Participants and Income-Eligible Nonparticipants. J Nutr. 2015;145(3):622-627. https://doi.org/10.3945/jn.114.199414
Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The Relationship Between Food Insecurity and Depression, Diabetes Distress and Medication Adherence Among Low-Income Patients with Poorly-Controlled Diabetes. J Gen Intern Med. 2015;30(10):1476-1480. https://doi.org/10.1007/s11606-015-3351-1
Palar K, Frongillo EA, Escobar J, et al. Food Insecurity, Internalized Stigma, and Depressive Symptoms Among Women Living with HIV in the United States. AIDS Behav. 2018;22(12):3869-3878. https://doi.org/10.1007/s10461-018-2164-8
Frongillo EA, Nguyen HT, Smith MD, Coleman-Jensen A. Food Insecurity Is Associated with Subjective Well-Being among Individuals from 138 Countries in the 2014 Gallup World Poll. J Nutr. 2017;147(4):680-687. https://doi.org/10.3945/jn.116.243642
Martin MS, Maddocks E, Chen Y, Gilman SE, Colman I. Food insecurity and mental illness: disproportionate impacts in the context of perceived stress and social isolation. Public Health. 2016;132:86-91. https://doi.org/10.1016/j.puhe.2015.11.014
Hanmer J, DeWalt DA, Berkowitz SA. Association between Food Insecurity and Health-Related Quality of Life: a Nationally Representative Survey. J Gen Intern Med. Published online January 6, 2021. https://doi.org/10.1007/s11606-020-06492-9
Berkowitz SA, Shahid NN, Terranova J, et al. “I was able to eat what I am supposed to eat”-- patient reflections on a medically-tailored meal intervention: a qualitative analysis. BMC Endocr Disord. 2020;20(1):10. https://doi.org/10.1186/s12902-020-0491-z
Stotz SA, Ricks KA, Eisenstat SA, Wexler DJ, Berkowitz SA. Opportunities for Interventions That Address Socioeconomic Barriers to Type 2 Diabetes Management: Patient Perspectives. Sci Diabetes Self-Manag Care. Published online February 28, 2021:0145721721996291. https://doi.org/10.1177/0145721721996291
Lund JJ, Chen TT, LaBazzo GE, Hawes SE, Mooney SJ. The association between three key social determinants of health and life dissatisfaction: A 2017 behavioral risk factor surveillance system analysis. Prev Med. Published online July 13, 2021:106724. https://doi.org/10.1016/j.ypmed.2021.106724
Te Vazquez J, Feng SN, Orr CJ, Berkowitz SA. Food Insecurity and Cardiometabolic Conditions: a Review of Recent Research. Curr Nutr Rep. Published online June 21, 2021. https://doi.org/10.1007/s13668-021-00364-2
AHRQ. Medical Expenditure Panel Survey Home. Published June 26, 2020. Accessed June 26, 2020. https://meps.ahrq.gov/mepsweb/
United States Department of Agriculture Economic Research Service. Food Security Survey Module. Accessed January 17, 2018. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/
Frongillo EA. Validation of measures of food insecurity and hunger. J Nutr. 1999;129(2S Suppl):506S-509S. https://doi.org/10.1093/jn/129.2.506S
Hamilton WL, Cook JT, States U, et al. Household Food Security in the United States in 1995: Technical Report of the Food Security Measurement Project. Published online 1997. https://www.fns.usda.gov/household-food-security-united-states-1995-summary-report-food-securitymeasurement-project
Food Security Survey Module Scoring. Accessed October 5, 2021. https://www.ers.usda.gov/media/8279/ad2012.pdf
Nord M, Statistics Division. Introduction to Item Response Theory Applied to Food Security Measurement: Basic Concepts, Parameters and Statistics. FAO; 2014. . http://www.fao.org/publications/card/en/c/577f6a79-9cbd-49f5-b606-500ea42bf88e/
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Published online March 2000. . https://fns-prod.azureedge.net/sites/default/files/FSGuide.pdf
Selim AJ, Rogers W, Fleishman JA, et al. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12). Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2009;18(1):43-52. https://doi.org/10.1007/s11136-008-9418-2
About the VR-36©, VR-12© and VR-6D© | SPH. Accessed July 15, 2021. https://www.bu.edu/sph/about/departments/health-law-policy-and-management/research/vr-36-vr-12-and-vr-6d/about-the-vr-36-vr-12-and-vr-6d/
Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S-1739S. https://doi.org/10.3945/ajcn.111.012070
Palar K, Napoles T, Hufstedler LL, et al. Comprehensive and Medically Appropriate Food Support Is Associated with Improved HIV and Diabetes Health. J Urban Health Bull N Y Acad Med. 2017;94(1):87-99. https://doi.org/10.1007/s11524-016-0129-7
Centers for Disease Control and Prevention. Measuring Healthy Days. Published online November 2000. Accessed January 17, 2018. https://www.cdc.gov/hrqol/pdfs/mhd.pdf
Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. https://doi.org/10.1001/archpsyc.60.2.184
Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284-1292. https://doi.org/10.1097/01.MLR.0000093487.78664.3C
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271-292. https://doi.org/10.1016/S0167-6296(01)00130-8
Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42(9):851-859. https://doi.org/10.1097/01.mlr.0000135827.18610.0d
Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-233. https://doi.org/10.1097/00005650-199603000-00003
Agency for Healthcare Research and Quality. MEPS HC-201 2017 Full Year Consolidated Data File. Accessed July 15, 2021. https://www.meps.ahrq.gov/data_stats/download_data/pufs/h201/h201doc.pdf
Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26-32. https://doi.org/10.1542/peds.2009-3146
Williams R. Generalized Ordered Logit/Partial Proportional Odds Models for Ordinal Dependent Variables. Stata J Promot Commun Stat Stata. 2006;6(1):58-82. https://doi.org/10.1177/1536867X0600600104
Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652-659. https://doi.org/10.1111/j.0006-341x.1999.00652.x
Whittle HJ, Palar K, Seligman HK, Napoles T, Frongillo EA, Weiser SD. How food insecurity contributes to poor HIV health outcomes: Qualitative evidence from the San Francisco Bay Area. Soc Sci Med 1982. 2016;170:228-236. https://doi.org/10.1016/j.socscimed.2016.09.040
Whittle HJ, Palar K, Hufstedler LL, Seligman HK, Frongillo EA, Weiser SD. Food insecurity, chronic illness, and gentrification in the San Francisco Bay Area: An example of structural violence in United States public policy. Soc Sci Med 1982. 2015;143:154-161. https://doi.org/10.1016/j.socscimed.2015.08.027
Diehr P, Williamson J, Patrick DL, Bild DE, Burke GL. Patterns of self-rated health in older adults before and after sentinel health events. J Am Geriatr Soc. 2001;49(1):36-44. https://doi.org/10.1046/j.1532-5415.2001.49007.x
Hanmer J, Kaplan RM. Update to the Report of Nationally Representative Values for the Noninstitutionalized US Adult Population for Five Health-Related Quality-of-Life Scores. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2016;19(8):1059-1062. https://doi.org/10.1016/j.jval.2016.05.019
Access to Data and Data Analysis
Seth A. Berkowitz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Role of the Funder
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding
Seth A. Berkowitz’s role in the research reported in this publication was supported by the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number K23DK109200. Deepak Palakshappa’s work on this project was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K23HL146902. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
SAB reports personal fees from the Aspen Institute, outside of the submitted work. All other authors report no conflicts.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation
None
Supplementary Information
ESM 1
(DOCX 2030 kb)
Rights and permissions
About this article
Cite this article
Berkowitz, S.A., Palakshappa, D., Seligman, H.K. et al. Changes in Food Insecurity and Changes in Patient-Reported Outcomes: a Nationally Representative Cohort Study. J GEN INTERN MED 37, 3638–3644 (2022). https://doi.org/10.1007/s11606-021-07293-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07293-4