Abstract
Background
Hospitals serving a disproportionate share of racial/ethnic minorities have been shown to have poorer quality outcomes. It is unknown whether efficiencies in inpatient care, measured by length of stay (LOS), differ based on the proportion patients served by a hospital who are minorities.
Objective
To examine the association between the racial/ethnic diversity of a hospital’s patients and disparities in LOS.
Design
Retrospective cross-sectional study.
Participants
One million five hundred forty-six thousand nine hundred fifty-five admissions using the 2017 New York State Inpatient Database from the Healthcare Cost and Utilization Project.
Main Measure
Differences in mean adjusted LOS (ALOS) between White and Black, Hispanic, and Other (Asian, Pacific Islander, Native American, and Other) admissions by Racial/Ethnic Diversity Index (proportion of non-White patients admitted to total patients admitted to that same hospital) in quintiles (Q1 to Q5), stratified by discharge destination. Mean LOS was adjusted for patient demographic, clinical, and admission characteristics and for individual intercepts for each hospital.
Key Results
In both unadjusted and adjusted analysis, Black-White and Other-White mean LOS differences were smallest in the most diverse hospitals (Black-White: unadjusted, −0.07 days [−0.1 to −0.04], and adjusted, 0.16 days [95% CI: 0.16 to 0.16]; Other-White: unadjusted, −0.74 days [95% CI: −0.77 to −0.71], and adjusted, 0.01 days [95% CI: 0.01 to 0.02]). For Hispanic patients, in unadjusted analysis, the mean LOS difference was greatest in the most diverse hospitals (−0.92 days, 95% CI: −0.95 to −0.89) but after adjustment, this was no longer the case. Similar patterns across all racial/ethnic groups were observed after analyses were stratified by discharge destination.
Conclusion
Mean adjusted LOS differences between White and Black patients, and White and patients of Other race was smallest in most diverse hospitals, but not differences between Hispanic and White patients. These findings may reflect specific structural factors which affect racial/ethnic differences in patient LOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Length of stay (LOS)—as the time from a patient’s admission to discharge—is used as a management tool to understand operational aspects of patient treatment in hospital, and the resources required for safe discharge.1 To ensure operational viability against high bed occupancy rates,2 hospitals have found the need to actively manage LOS not only for the financial well-being of their systems, but also because of the increasing evidence linking adverse health outcomes associated to emergency department boarding,3 ambulance diversion to manage occupancy issues,4 and delays in discharge.5 Reflecting its important role, the Center of Medicare and Medicaid Service’s (CMS) added LOS as a risk-adjusted quality metric to the Physician Value-Based Payment Modifier (PVBPM) Program in 2017.
Using an adjustment method to account for patient’s age, disease severity, and diagnosis, hospital-based physicians are subject to potential penalties in the PVBPM if a patient’s observed LOS exceeded the risk-adjusted LOS. However, there is growing evidence that race/ethnicity6,7 and socioeconomic status8,9 may play a role in a patient’s LOS, although mechanisms remain unclear.
One important, yet unstudied, factor may involve the racial/ethnic composition of hospitals. In studies examining 30- and 90-day mortality rates of acute myocardial infarction, heart failure, and pneumonia, hospitals with a disproportionate share of Black patients have been shown to have a 9–11% increased risk of mortality, compared to hospitals with smaller shares of Black patients.10,11 These differences may be attributable to underlying characteristics of hospitals such as safety-net status. However, there is increasing recognition that structural inequities may play an important role in creating adverse health outcomes for historically disenfranchised minority groups through discrimination, and segregation.12 In this study, we analyzed a comprehensive state-wide admissions-level dataset to explore the association between racial/ethnic hospital composition and racial/ethnic differences in LOS.
METHODS
Data Sources and Study Cohort
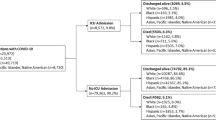
We created an analytical file of all-payer inpatient discharges using the 2017 New York State Inpatient Database from the Healthcare Cost and Utilization project, created by the Agency of Healthcare Research and Quality. Using the Centers for Medicare and Medicaid Services Diagnosis-Related Group (DRG) listing as guide, we categorized DRGs by whether they are more likely to managed on a medical or surgical ward, excluding obstetric, pediatric, and psychiatric diagnoses using the CMS categorization of DRGs as either medical or surgical.13
We excluded from the study cohort individuals under the age of 18 years, those who died during their inpatient stay, patients admitted to non-acute care hospitals (e.g., psychiatric hospitals) or critical access hospitals (because of their federally mandated LOS requirements),14 admissions who were not likely to be admitted to a medical or surgical ward based on our categorization, and patients admitted to hospitals who admitted only White patients or non-White patients (because there would prevent in-hospital racial/ethnic comparisons).
Furthermore, the degree of missingness within important covariates in our analytical file was examined. There was no missingness observed in the race/ethnicity data. Additional analyses to detect patterns across hospitals by racial/ethnic were undertaken, and these results are summarized in the exclusion cascade in the Supplement. Our final analytical cohort consisted of 1,546,955 admissions.
Racial/Ethnic Diversity Index
We created the Racial/Ethnic Diversity Index (RDI) to identify each hospital’s racial/ethnic patient population. The RDI was calculated by dividing the number of unique adult non-White (Black, Hispanic, and Other [Asian, Pacific Islander, Native American, and Other]) patients admitted by the number of all unique adult patients admitted in that same hospital. As the RDI of a hospital increased, the number of non-White admissions increased as a proportion of total admissions during the 2017 calendar year. Observations were then segmented into quintiles of RDI.
Study Outcome
Our primary outcome was the difference in mean adjusted LOS (ALOS) between White and Black, Hispanic, and patients admitted of Other race/ethnicity across RDI quintiles. A secondary analysis stratified this outcome by discharge destination (home vs non-home destinations [i.e., acute rehabilitation, skilled nursing facilities, long-term acute care hospitals]). We stratified by admissions discharged to home vs non-home destinations because discharge to non-home destinations may be related to LOS if admissions decondition during their hospitalization, and require rehabilitation to regain premorbid function,15 and because potential penalties apply for hospitals discharging patients to post-acute care subject to the CMS Post-Acute-Care Transfer Policy.16
Modeling Strategy
We operationalized an evidence-based conceptual model depicting the factors affecting patient LOS to model the mean ALOS by RDI quintile. This conceptual framework, described elsewhere,13 highlights how patient demographic characteristics such as age, sex, race/ethnicity, and their condition (both diagnoses and severity), as well as admission-related characteristics such as time of day of admission and type of admission (i.e., elective vs non-elective), hospital characteristics, and discharge disposition all influence patient LOS.
In line with the same modeling strategy used in previous work,17,18 we modeled LOS in days and hours using multivariate generalized linear models, treating LOS as a gamma-distributed dependent variable because of its non-negative, right-skewed distribution.17 Our model’s exposure was race/ethnicity (using White as the reference group). Control covariates of the adjustment model included the following admission-level characteristics: age, sex, median household income by patient zip code (in quartiles), and health insurance status (Medicare, Medicaid, private insurance, self-pay, no charge, other), the number of chronic diseases, and Elixhauser-related mortality score.19 In addition, the model incorporated separate intercepts for each DRG and each hospital to account for differences between DRGs, and allow within-hospital comparisons (i.e., hospital fixed effects and DRG fixed effects).20 Variables were checked for multicollinearity using variation inflation factors in a stepwise fashion. Standard errors were clustered at the level of the hospital.
Statistical Analysis
First, across RDI quintiles, we summarized continuous variables with means and standard deviations, or medians and interquartile ranges (IQRs) where appropriate, and categorical variables with percentages.
Then, we calculated the mean observed LOS overall, and then stratified by discharge destination for each RDI quintile. Following this, we calculated the mean ALOS differences by race/ethnicity using the modeling strategy previously described. A two-sided α of 0.05 was used throughout. Analysis was performed in STATA (Version 16) and R (version 3.5.2).
This research was approved by the institutional review board of the author’s institution.
Sensitivity Analyses
A sensitivity analysis was performed. This analysis included patients who died during their hospital stay, and employed same modeling strategy as the primary analysis.
RESULTS
Baseline Characteristics
Our cohort consisted of 1,546,955 discharges (Table 1). As hospitals’ patient population became more diverse, the proportion of Medicaid-insured admissions increased (RDI quintile 1 [Q1]: 12.5% to Q5: 40.6%), the mean number of chronic conditions decreased (Q1: 7.2 to Q5: 6.1), the proportion of elective admissions also declined (Q1: 24.0% to Q5: 8.9%), and the proportion of non-home discharges increased (Q1: 24.1% to Q5: 17.7%).
The racial/ethnic mix of hospitals in Q1 was 90.5% White, 4.3% Black, 2.2% Hispanic, and 3.0% Other. In Q2, this shifted to 79.1% White, 10.8% Black, 4.5% Hispanic, and 5.5% Other; the racial/ethnic mix in Q3 was 63.6% White, 15.8% Black, 10.3% Hispanic, and 10.4% Other. In Q4, this became 38.4% White, 17.2% Black, 14.5% Hispanic, and 29.2% Other, and in hospitals with the most diverse patient populations (Q5) the racial/ethnic mix was 11.2% White, 37.9% Black, 26.2% Hispanic, and 24.7% Other.
Unadjusted Analysis
Results from the unadjusted analysis are reported in Table 2. As hospitals’ patient populations become more diverse, overall mean observed LOS differences between Black and White patients, and Hispanic and White patients, declined (Black-White Q1: 0.68 days [95% CI: 0.58 to 0.79] to Q5: −0.07 days [−0.1 to −0.04; Hispanic-White Q1: −0.17 days [95% CI: −0.33 to 0] to Q5: −0.92 days [−0.95 to −0.89]), but not between Other and White patients. However, across all racial/ethnic groups, the smallest overall mean LOS difference compared to White patients was observed in RDI quintile 5, which represented the most diverse hospitals. When stratified by discharge destination, this finding—that the smallest mean LOS difference compared to White was observed in RDI Q5—persists across all race/ethnic groups only for patients discharged home (Black-White: 0.09 days, 95% CI: 0.07 to 0.12; Hispanic-White: −0.39 days, 95% CI: −0.42 to 0.37; and Other-White: −0.4 days, 9% CI: −0.42 to −0.38), but not for those discharged to non-home destinations.
Adjusted Analysis
In adjusted analysis (Table 3), the consistent declines in Black-White and Hispanic-White mean ALOS differences are no longer seen when compared to the unadjusted analysis. For Black and Other patients, the greatest overall mean ALOS differences are seen consistently in the most diverse hospitals (RDI quintile 5): Black-White 0.16 days, 95% CI: 0.16 to 0.16, and Other-White, 0.01 days, 95% CI: 0.01 to 0.02, and similar findings are noted in stratified analysis by discharge destination. However, for Hispanic patients compared to White patients, this is not the case with the smallest mean ALOS difference noted in quintile 4 overall (mean ALOS difference: −0.07 days; 95% CI: −0.12 to −0.02) and by discharge destination (discharge home: −0.06 days; 95% CI: −0.08 to −0.05; discharge to non-home destination: −0.09 days; 95% CI: −0.14 to −0.04).
Sensitivity Analysis
In the sensitivity analyses which included patients who died during their hospital stay, estimates are largely consistently with those from the primary analyses (Supplement).
DISCUSSION
In this study of the association between in-hospital patient diversity and racial/ethnic differences in adjusted LOS, we found that compared to White patients, mean LOS differences across all minority groups were smallest in the most diverse hospitals. However, after adjusting for demographic, clinical, admission-related, and hospital-related factors, these findings remained true for Black-White and Other-White, but not Hispanic-White mean ALOS differences.
To our knowledge, this is the first study to examine the relationship between racial/ethnic inpatient composition and LOS in an all-payer state-wide inpatient dataset. In general, despite the importance of LOS as a measure for hospital operational efficiency, racial/ethnic differences in LOS have not been well-studied. The few that have studied racial/ethnic differences demonstrate notable racial/ethnic LOS differences in various surgical procedures, 7,21,22 and across various different diagnoses.13,18 Meaningful managerial attempts to shorten LOS through operational efficiencies typically yield an improvement of 0.3–0.7 days on average,23 and hospitalists (i.e., physicians who work exclusively in the inpatient setting) yield LOS improvements of 0.69 days.24 Our findings show that unadjusted racial/ethnic differences in LOS may equal or even exceed these improvements, although after adjustment, racial/ethnic disparities in LOS exist but are attenuated.
Adjusting for factors which influence LOS had an important effect on racial/ethnic differences in mean LOS. We observed that the declines in Black-White and Hispanic-White differences in mean LOS disappeared, and that disparities in LOS persisted, although inconsistently in the most diverse hospitals. The nature of our study design—to compare the unadjusted to adjusted differences in mean LOS—aimed to explain the variation in the observed mean LOS differences using a modeling strategy which removed the confounding influence of various demographic, clinical, admission, and hospital-related factors. However, we were not able to control for several other important variables, which are known to influence patient LOS, and may explain the differences observed in the adjusted analysis. These include individual-level social factors such as marital status25 and the patient’s social network,26 or hospital-related factors including care coordination strategies and workflows,27 which may hasten a more speedy discharge from hospital. Importantly, among the factors which we were unable to control for, which may explain between-hospital differences adjusted LOS, include those which may be structurally determined by historical and political forces not captured in the SID dataset. These include residential segregation, redlining, and racial/ethnically discriminating factors.12 Nonetheless, that racial/ethnic differences in mean ALOS persist may suggest that these social forces continue to play a role both directly and indirectly in the management of minority patients in the hospitalized setting. Future research is required to explore this more rigorously.
This study has four limitations. First, we used admissions-level data from New York State alone, and the results may not be generalizable to other states with high degrees of racially segregated populations. Nonetheless, New York represents a large, diverse state with a population of almost 20 million with large rural population.28 Second, our conceptual framework lacks a detailed understanding of the pre-hospitalization factors which are likely to influence LOS, factors which may relate to socio-political, economic, and historical undercurrents which structurally predispose minority groups to worse health outcomes. Given this conceptual framework is a summation of the prevailing literature on length of stay, this reflects a dearth of evidence focused on the social factors that influence LOS. Third, our development of the RDI is yet to be validated in the HCUP dataset, and with other datasets. By analyzing hospital patient diversity in this way, we presumed the factors influencing racial/ethnic differences in aALOS between White and Black, Hispanic and patients of Other race/ethnicity patients were the same. However, this is unlikely to be the case. Fourth, the closest measure of socioeconomic status available was median income by patient zip code, in quartiles. This was likely to be inadequate to reflect the nuance of socioeconomic forces which influence health and health-related outcomes in a myriad of ways. Lastly, in our modeling strategy, we employed individual intercepts for DRGs as disease controls, not individual diagnoses. However, while DRGs are imprecise tools to determine individual diagnoses, they represent diagnosis categories which allow a study of LOS at ward level. Analysis by ward type within each hospital allowed us to indirectly assess important ward-level effects such the role of discharge care coordination, and nursing care, all of which play important roles in the discharge process.15 Moreover, DRGs are the primary means of revenue generation for hospitals.
In conclusion, we found that compared to White patients, mean LOS differences across all minority groups was smallest in the most diverse hospitals. However, after adjusting for demographic, clinical, admission-related, and hospital-related factors, these findings remained true for Black-White and Other-White, but not Hispanic-White mean ALOS differences. These findings may reflect specific structural factors which affect racial/ethnic differences in patient LOS.
References
McDermott C, Stock G. Hospital operations and length of stay performance. International Journal of Operations & Production Management 2007;27:1020-1042.
National Center for Health Statistics. Occupancy Rates in Community Hospitals and Average Annual percent Change, by State: United States, Selected Years 1960—2015. In. Rockville, Md: Centers for Disease Control and Prevention; 2017
Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605-611.e606.
Shen YC, Hsia RY. Ambulance diversion associated with reduced access to cardiac technology and increased one-year mortality. Health Aff (Millwood) 2015;34(8):1273-1280.
Rojas-García A, Turner S, Pizzo E, Hudson E, Thomas J, Raine R. Impact and experiences of delayed discharge: A mixed-studies systematic review. Health Expectations 2018;21(1):41-56.
Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med 2009;16(5):403-410.
Elsamadicy AA, Koo AB, David WB, et al. Portending Influence of Racial Disparities on Extended Length of Stay after Elective Anterior Cervical Discectomy and Interbody Fusion for Cervical Spondylotic Myelopathy. World Neurosurgery. 2020
Moore L, Cisse B, Batomen Kuimi BL, et al. Impact of socio-economic status on hospital length of stay following injury: a multicenter cohort study. BMC Health Services Research 2015;15(1):285.
Wadhera RK, Choi E, Shen C, Yeh RW, Joynt Maddox KE. Trends, Causes, and Outcomes of Hospitalizations for Homeless Individuals: A Retrospective Cohort Study. Medical Care. 2019;57(1)
López L, Jha AK. Outcomes for whites and blacks at hospitals that disproportionately care for black Medicare beneficiaries. Health Serv Res 2013;48(1):114-128.
Srivastava PK, Fonarow GC, Bahiru E, Ziaeian B. Association of Hospital Racial Composition and Payer Mix With Mortality in Acute Coronary Syndrome. J Am Heart Assoc. 2019;8(21):e012831.
Bailey ZD, Feldman JM, Bassett MT. How Structural Racism Works — Racist Policies as a Root Cause of U.S. Racial Health Inequities. New England Journal of Medicine 2020;384(8):768-773.
Ghosh AK, Geisler BP, Ibrahim S. Racial/ethnic and socioeconomic variations in hospital length of stay: A state-based analysis. Medicine (Baltimore) 2021;100(20):e25976.
Schoenbaum M. Critical access hospitals: hubs for rural health care. Minn Med 2011;94(9):34-37.
Hoyer EH, Friedman M, Lavezza A, et al. Promoting mobility and reducing length of stay in hospitalized general medicine patients: A quality-improvement project. J Hosp Med 2016;11(5):341-347.
Joanne C. Medicare Improperly paid acute-care hospitals $54.4 million for inpatient claims subject to the Post-Acute-Care Transfer Policy. Washington DC: US Department of Heath and Human Services;2019. A-09-19-03007
Faddy M, Graves N, Pettitt A. Modeling length of stay in hospital and other right skewed data: comparison of phase-type, gamma and log-normal distributions. Value Health 2009;12(2):309-314.
Ghosh AK, Unruh MA, Soroka O, Shapiro M. Trends in Medical and Surgical Admission Length of Stay by Race/Ethnicity and Socioeconomic Status:A Time Series Analysis. Health Services Research and Managerial Epidemiology 2021;8:1-9.
Thompson NR, Fan Y, Dalton JE, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Medical care 2015;53(4):374-379.
Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care 2005;43(4):308-319.
Giglia MD, DeRussy A, Morris MS, et al. Racial disparities in length-of-stay persist even with no postoperative complications. J Surg Res 2017;214:14-22.
Peck CJ, Pourtaheri N, Shultz BN, et al. Racial Disparities in Complications, Length of Stay, and Costs Among Patients Receiving Orthognathic Surgery in the United States. J Oral Maxillofac Surg 2020.
Gonçalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2016;2016(1):Cd000313
Rachoin JS, Skaf J, Cerceo E, et al. The impact of hospitalists on length of stay and costs: systematic review and meta-analysis. Am J Manag Care. 2012;18(1):e23-30.
Konda SR, Gonzalez LJ, Johnson JR, Friedlander S, Egol KA. Marriage Status Predicts Hospital Outcomes Following Orthopedic Trauma. Geriatr Orthop Surg Rehabil 2020;11:2151459319898648.
Landeiro F, Leal J, Gray AM. The impact of social isolation on delayed hospital discharges of older hip fracture patients and associated costs. Osteoporos Int 2016;27(2):737-745.
Hajewski CJ, Shirey MR. Care coordination: a model for the acute care hospital setting. J Nurs Adm 2014;44(11):577-585.
United States Census Bureau. Table 1. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2010 to July 1, 2019 (NST-EST2019-01). 2020; https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html. Accessed June 29th 2020
Funding
Dr. Ghosh is supported by a National Center for Advancing Translational Sciences (NCATS) grant KL2-TR-002385 of the Clinical and Translational Science Center at Weill Cornell Medical College. Dr. Ibrahim is supported in part by a K24 Mid-Career Development Award from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (K24AR055259).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghosh, A.K., Unruh, M.A., Ibrahim, S. et al. Association Between Patient Diversity in Hospitals and Racial/Ethnic Differences in Patient Length of Stay. J GEN INTERN MED 37, 723–729 (2022). https://doi.org/10.1007/s11606-021-07239-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07239-w