Abstract
Background
Seventeen medical homes (MHs) were established in the Local Health Authority (LHA) of Parma (about 450,000 residents), Emilia Romagna, Italy, between 2011 and 2016.
Objective
To estimate the effects of MH implementation on healthcare utilization.
Design
We conducted a longitudinal cohort study (01/2011–12/2017) using the Parma LHA administrative healthcare database.
Participants
Residents for ≥1 year and older than 14 years of age with a documented primary care physician (PCP) in Parma LHA.
Intervention
MH exposure status was classified for each resident as either receiving care from a PCP that (1) eventually practices in an MH (pre-MH), (2) is currently in an MH (post-MH), or (3) does not join an MH (non-MH).
Main Outcome Measures
Risks of ordinary inpatient hospital admissions, day hospital admissions, admissions for ambulatory care sensitive conditions (ACSCs), all-cause emergency department (ED) visits, and deferrable ED visits were compared using Cox proportional hazards regression and risks of all-cause 30- and 90-day readmissions for congestive heart failure (CHF) or chronic obstructive pulmonary disease (COPD) were compared using logistic regression.
Key Results
Prior to MH implementation, the risk of all-cause ED visits for pre-MH residents was 0.93 (95% CI: 0.92–0.94) that of non-MH residents. After MH implementation, the relative risk for post-MH versus non-MH was 0.86 (95% CI: 0.85–0.87) and, over time, post-MH versus pre-MH was 0.93 (95% CI: 0.92–0.94). Hospitalization risks were generally lower among the pre-MH and post-MH, compared to non-MH. However, hospitalizations and HF or COPD readmissions were not generally lower post-MH compared to pre-MH.
Conclusions
This MH initiative was associated with a 7% reduction in risk of ED visits. More research is necessary to understand if ED visit risk will continue to improve and how other aspects of healthcare utilization might change as more MHs open and the length of exposure to MHs increases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Despite differences in organizational settings, cultural context, and policymaking considerations between the USA and Europe, they share the common priority to implement effective primary care models that provide continuous, comprehensive, coordinated care and serve as the first point of contact for most healthcare needs.1,2 In the USA and Europe, the medical home (MH) model is one of the most promising approaches to reforming primary care delivery. MHs aim to better manage populations with high-quality ambulatory and preventative care services, payment systems that recognize value conferred to local residents, and ultimately avoid adverse events that result in high-cost acute utilization.1,2 The MH model is based on primary care physician (PCP)–led multidisciplinary care teams assuming responsibilities for comprehensive care of residents through coordination with other qualified professionals.
Primary care has a central role in the Italy’s National Health Service (NHS), which provides universal coverage to all citizens and legal foreign residents.3 The 20 regions are responsible for delivering care through geographically defined Local Health Authorities (LHAs), which deliver primary care, hospital care, outpatient specialist care, public health care, and health services related to social care. Each citizen is required by law to enroll with a PCP or pediatrician (for children up to 14 years old) within a specific LHA. 4 They may choose any PCP or pediatrician having fewer than the maximum number of patients allowed (1500 for PCPs, 800 for pediatricians) and may switch at any time.
The services of the PCPs and pediatricians are free at the point of use. PCPs and pediatricians act as “gatekeepers” for the system, assessing patient needs, prescribing pharmaceuticals, and ordering diagnostic procedures, and referrals to specialists and hospitals. They are self-employed and paid on a capitation basis depending on the number of patients on their list. LHAs can also remunerate them for additional care to specific patients, such as home care to chronically ill patients, or for reaching targets related to quality or spending levels.
Traditionally, PCPs and pediatricians have worked in solo practices with minimal to no auxiliary staff or structured, formal relations with other PCPs. With the belief that a strong primary care system is conducive to improving population health, in the last 20 years the Italian NHS initiated a restructuring which introduced reforms that incentivized PCPs and pediatricians to organize into collaborative arrangements. As such, group practices have become more common, particularly in the northern part of the country. As a further evolution, in 2007 the Italian NHS announced plans for the Italian MH model.5 They included investments in infrastructure and care coordination and management to increase continuity of care, establish a single access point for health and social services, provide team-based care, empower residents, foster interdisciplinary collaboration, improve communication strategies, develop prevention programs to be applied across the life course, improve quality and access to care, and deliver continuing education for health professionals. Because each of Italy’s 20 regions plans, administers, and reimburses healthcare services for their residents, the development of the MH model has taken distinct paths within each region.
The Emilia-Romagna region has established 107 MHs as of 2019 across its 8 LHAs.6 In Emilia-Romagna, the MH initiative has involved investments in infrastructure (e.g., disease registries, population health management, new physical facilities that promote team-based care) and efforts aimed at redesigning care delivery including care coordination and care management, resident empowerment, and expanded access to care (e.g., longer hours of operation, open scheduling, electronic messaging). Value-based payment models have also been implemented to better align the goal of population health management with physician compensation. To guarantee continuity of care, an MH in Emilia-Romagna should at minimum have a multidisciplinary team made of a PCP, a pediatrician, a nurse, a social worker, a midwife, and at least a specialist.7 In light of the historical solo practice model of primary care in Italy and our prior documentation of pockets of antipathy towards interprofessional collaboration among physicians and nurses in Parma LHA, the cultural changes necessary for effective team-based care within the primary care setting were expected to develop gradually.8
Between 2011 and 2016, 17 MHs were established in the LHA of Parma, Emilia-Romagna. We conducted a preliminary cross-sectional comparison of healthcare use among residents receiving care in MHs with those in traditional practices (solo practices or other collaborative arrangements) in the LHA of Parma, Emilia-Romagna, during 2015.9 Utilization in MHs was associated with lower rates of emergency department (ED) visits and hospitalizations for chronic ambulatory care sensitive conditions, though we recognize the potential for selection bias in cross-sectional designs.
This study presents longitudinal data that characterizes changes in healthcare utilization over time and accounts for how physicians that provide care in an MH and their patients might be distinct from those that do not. We hypothesized that MHs were associated with reductions in utilization, possibly depending on how long the PCPs had practiced in their MH, when their MH was implemented, and the complexity of their MH.
METHODS
Population and Data Sources
The study sample included residents aged 14 years or older assigned to a Parma LHA PCP for at least 1 year during the study period. Information on their hospital, emergency department, and specialty utilizations were available from the LHA’s administrative healthcare database as well as demographics, laboratory orders, and pharmacy data. Residents’ encounters with PCPs are not recorded in the database.
Study Design
This was a cohort study from January 1, 2011, to December 31, 2017. Follow-up began the earliest date and all inclusion criteria were satisfied and completed at the first of either the end of the study period, death, exit from Parma LHA, end of care from a PCP in Parma LHA, or long-term hospitalization (>30 days).
According to the comprehensiveness of services provided, Emilia-Romagna regional healthcare system classifies MHs into two categories or levels of complexity depending on the range of services offered: low complexity and medium/high complexity.7 In addition to the minimum multidisciplinary team present in a low complexity MH, the medium/high complexity MH offers services on at least a 12-h basis (8 am to 8 pm), including diagnostics, family counseling, home care, prevention and public health, cognitive disorder services, and a wider range of medical specialties (Supplemental Table S1).
The original LHA Parma MH Development Plan delineated the establishment of 26 MHs.10 Because of the geographic characteristics of the LHA territory, in the mountain and hill areas with a low population density the LHA Parma MH Development Plan forecasts to set up essentially low complexity MHs, as opposed to medium/high complexity MHs planned in urban areas. As of 2021, the establishment of the 26 MHs has not been completed. In fact, the success and rapidity of the process have been influenced by a number of concomitant factors, including the resources needed for the acquisition/creation of the physical MH space, the willingness of PCPs/pediatricians and other professionals to join an MH, and the local ability to integrate existing healthcare and social services within the MH initiative. No MHs were active when our study began, the first MHs opened in December 2011, and 17 were active with at least 1 year of follow-up by the end of the study period in December 2017 (Fig. 1).
Exposure
Each resident’s PCP assignment was updated continuously throughout the study period. Exposure to MH care on a given date depended on whether their PCP was currently affiliated with an MH. Exploratory data analyses suggested that, compared to PCPs who would not be affiliated with an MH during the study period, PCPs who would tended to have distinct healthcare utilization rates among their patients preexisting their MH. To adjust for this, we constructed a three-group MH exposure variable to estimate changes in utilization associated with MH initiation. Specifically, each day of follow-up was categorized for each resident as either
-
1.
Pre-MH (i.e., assigned to a PCP that will be affiliated with an MH at a future date),
-
2.
Post-MH (i.e., assigned to a PCP presently practicing in an MH), or
-
3.
Non-MH (i.e., assigned to a PCP that will not be affiliated with an MH).
Healthcare Utilization Measures
Healthcare utilization measures were chosen based on a literature review and available data. All-cause hospital admissions included ordinary inpatient hospital admissions and day hospital admissions included outpatient assessment, treatment, or rehabilitation. Admissions for ambulatory care sensitive conditions (ACSCs) were indicators of outpatient care quality and defined by ICD-9 codes for an ACSC in the primary position on the hospital claim for diabetes, chronic obstructive pulmonary disease (COPD), hypertension, congestive heart failure (CHF), bacterial pneumonia, urinary tract infection (UTI), angina, asthma, and dehydration. All-cause and deferrable ED use visits were defined as potentially avoidable through effective ambulatory care. A deferrable ED visit was defined as “non-urgent” or “urgent-deferrable,” in which the resident arrived at the ED through their own means of transportation and did not result in a hospital admission. All-cause readmissions within 30 days and 90 days of the hospital discharge date for CHF or COPD were potential indicators of quality of coordination between inpatient and outpatient settings during care transitions for residents with chronic conditions.
Statistical Analysis
Demographic characteristics were summarized as of the time of study entry. Additionally, since residents’ affiliation with MHs could change over time, characteristics of residents exposed to and not exposed to MHs were summarized by the amount of time contributed to each exposure group.
To assess the association of MH exposure and study outcomes, recurrent events Cox proportional hazards models were adjusted for time-fixed covariates for the sex of the resident and their PCP and time-dependent covariates for age, geographic location (mountain, hill, or plain; a proxy for population density), median household income in their commune of residence (the smallest administrative geographic unit in Italy), driving time to nearest hospital, and their PCP’s age. Because the diagnoses observed on claims over time may result from medical management changing over time and not preexisting disease burden, clinical conditions were not considered potential confounders as that would falsely attribute at least some of the MH effect to confounding. Empirically, the potential for confounding appeared minimal as the prevalence of chronic conditions was similar among exposed and unexposed residents.9
Each utilization outcome was modeled separately. From these models, we focused on three utilization risk or odds comparisons:
-
A.
Pre-MH vs. non-MH,
-
B.
Post-MH vs. non-MH, and
-
C.
MH Gain: B. vs. A.
That is, C. estimates the gains, in terms of reducing utilization risk or odds, after the introduction of the MHs. This approach of contemporaneous comparisons to the same non-MH PCPs in A. and B. effectively controlled C. for secular trends broadly affecting utilization risk across different calendar times.
Similarly, for CHF and COPD readmissions, we analyzed GEE logistic regression models of multiple index hospitalizations per patient over time adjusted for time-fixed and time-dependent covariates. The within-patient correlation of observations over time was modeled using a first-order autoregressive structure.
Three additional analyses explored heterogeneity in the exposure-risk relationships associated with:
-
1)
MH recency (MH care within its first year of operation vs. afterward),
-
2)
Early vs. later MH (MHs implemented in 2011–2012 vs. 2013–2016), and
-
3)
MH complexity (i.e., MH care in lower vs. higher complexity MHs).
All analyses were performed in SAS 9.4 (SAS Institute Inc., Cary, NC).
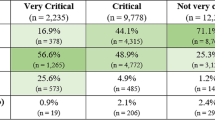
RESULTS
Among the 431,378 residents of Parma (median follow-up=7 years), 135,657 contributed to the post-MH group (median follow-up=4.5 years). Demographic characteristics of residents and the 371 PCPs are summarized in Table 1.
To illustrate how differences in deferrable ED visit and ordinary hospital admission rates tracked with PCPs and the timing of their MH affiliation, crude utilization rates are presented for patients of non-MH PCPs, patients of PCPs eventually or currently affiliated with an early MH, and patients of PCPs eventually or currently affiliated with a later MH in Figure 2. Throughout the study period, rates of ordinary admissions and deferrable ED visits were persistently higher among non-MH patients of non-MH PCPs compared to patients of PCPs eventually or currently affiliated with an MH. The variability between these rates for patients of early and later MH PCPs was modest.
Compared to non-MH patients, the adjusted risk of all-cause ED visits was 7% lower (HR=0.93, 95% CI: 0.92–0.94) among pre-MH patients and 14% lower among post-MH patients (HR=0.86, 95% CI: 0.85–0.87), suggesting there was a 7% gain in terms of reducing the relative risk of ED visits associated with MH (HR=0.93, 95% CI: 0.92–0.94) (Table 2). Similar gains were observed for deferrable and for ACSC ED visits. Estimates for hospitalization risks generally favored MH PCP patients consistently before and after MH implementation compared to non-MH PCP patients, reflecting little MH gains. Before MH implementation, the risk for ACSC hospitalization among pre-MH patients was 8% lower (HR=0.92, 95% CI: 0.87–0.97) than among non-MH patients, though we detected no MH gain (HR=0.99, 95% CI: 0.93–1.05). MH care was not associated with 30-day or 90-day hospital readmissions for CHF or COPD (Table 3).
Additional Analyses
Analyses of the recency of MH implementation suggested patients of PCPs practicing in an MH after its first year of operation experienced 13% gain in reduced ACSC ED visit risk over pre-MH (HR=0.87, 95% CI: 0.81–0.93) representing a 9% greater gain (HR=0.91, 95% CI: 0.83–0.99) than patients of PCPs practicing in an MH in its first year of operation (Supplemental Table S2). Patients of PCPs practicing in an MH after its first year of operation experienced a 31% greater gain in reduced odds of 30-day hospital readmission for CHF compared to patients of PCPs practicing in an MH in its first year of operation (OR=0.69, 95% CI: 0.47–0.99) (Supplemental Table S3).
Patients of PCPs in later MHs (i.e., implemented after 2012) experienced a 13% gain in reduced chronic ACSC admissions risk compared to pre-MH (HR=0.87, 95% CI: 0.78–0.97; Supplemental Table S4). Patients of PCPs in later MHs experienced a 20% gain in reduced CHF admission risk compared to pre-MH (HR=0.80, 95% CI: 0.69–0.93) which was 36% greater than the gain among patients of PCPs in early MHs (HR=1.36, 95% CI: 1.11–1.67). There were no clear differences in CHF or COPD readmission odds or gains between early and later MHs before or after MH implementation (Supplemental Table S5).
Patients of PCPs in low and medium/high complexity MHs experienced significant gains in reduced all-cause ED visits risk (HRlow=0.91, 95% CI: 0.90–0.93; HRmedium/high=0.94, 95% CI: 0.93–0.95) (Supplemental Table S6). There were no clear differences in CHF or COPD readmission odds or gains by MH complexity (Supplemental Table S7).
DISCUSSION
In this large population-based evaluation of the first 6 years of Parma LHA’s MH initiative, our findings suggested that, while hospitalization and readmission utilizations generally remained stable after MH implementation, MH-based care was associated with net gains in reducing risks of all-cause, deferrable, and ACSC ED visits. Our results suggested PCPs who would later join MHs tended to perform better than non-MH physicians on most utilization measures prior to MH implementation, and that these advantages were preserved after joining their MH. Greater gains in reducing the risk of ACSC ED visits and the odds of 30-day CHF readmissions were associated with care from PCPs having practiced longer in an MH. Greater gains in reducing the risks of chronic ACSC admissions, CHF admissions, and all ED visits were also associated with care from PCPs practicing in later MHs (implemented after 2012). However, MH complexity did not strongly influence changes in risks or odds of utilizations associated with MHs. These early results support the continued expansion of MH-based care in Parma LHA.
The MH initiative in Parma LHA closely resembles the international model of primary care transformation. Consistent with accumulating early results of MH projects in the USA, our results were somewhat mixed.11,12 However, we emphasize important distinctions in context. Unlike in the USA, the single-payer system in Italy provides universal healthcare coverage and requires citizens to designate a PCP as their usual source of care. Accordingly, the utilization differences we observed are likely to be associated with the structural (e.g., new health information technology, centralization of professionals and services, expanded hours) and process (e.g., to manage and coordinate care) changes to the primary care delivery system rather than newly obtaining a usual source of primary care.
Although certain aspects of primary care transformation take effect upon opening a new MH (e.g., expanded office hours), incremental improvements associated with increasing experience operating as an MH are expected since it takes time for other aspects to improve patient outcomes.13,14,15,16,17 In our study, a longer time since MH implementation was associated with modest improvements in ACSC ED visit risk and odds of CHF rehospitalization, but other utilization metrics were comparable in the first year and in later years after implementation.
Healthcare delivery interventions are often implemented over a period of years rather than simultaneously due to practical reasons such as local readiness, resources, and capacity. We hypothesized that early adopters of MHs in Parma LHA might be predisposed to team-based care and their readiness for change correlated with higher quality of care.18 However, later adopters experienced greater net reductions in chronic ACSC admission, CHF, and ED visit rates. This larger gain associated with later MHs may suggest potential benefits from accumulated institutional knowledge and possible spillover effects from interprofessional interactions between providers in later MHs and high-performing early MHs.19,20,21,22
Rural practices often suffer workforce shortages and diminished access to specialists and hospitals.23 In Parma LHA, six MHs had low complexity and all six were located in the rural mountainous areas. Our results did not vary by MH complexity, suggesting that having relatively fewer services and a lack of diversity in on-site specialists in rural Italy did not attenuate the benefits associated with MHs. Conversely, the apparent lack of an advantage for high complexity MHs in preventing hospital admissions for ACSCs and readmissions for chronic conditions raises questions about the effectiveness of care coordination between their PCPs and specialist physicians and with local hospitals.
The present study addresses important limitations of our prior cross-sectional evaluation of MHs in Parma LHA. Compared with our cross-sectional study,9 which reported a 14% lower rate of ED utilization associated with MHs, after accounting for differences in utilization prior to MH implementation, our current study showed a 7% lower risk of ED utilization. Due to capitation payment systems for PCPs in Parma LHA, our database lacked information on the number of visits to PCPs, a metric that has been observed to increase in some earlier MH projects.24,25 However, in the present longitudinal study, the comparisons of interest were effectively controlled for this and other sources of confounding by including time-fixed and time-dependent covariates and making comparisons between pre-MH and MH care utilization over time offset, respectively, by contemporaneous non-MH care utilization. Regardless, we cannot identify what specifically caused the benefits apparently attributable to the implementation of MHs.
Our assessment of the MH initiative in the Parma LHA took into consideration key outcomes of healthcare utilization. However, other quantitative and qualitative analyses could certainly offer valuable insights into the implementation of the MH model and provide context for generalizing findings. For instance, evaluations of patient experience in terms of access, empowerment, and behavioral health attitude, as well as healthcare professional experience in terms of workforce and cooperativeness, should be undertaken for a more comprehensive assessment of the MH implementation.
CONCLUSIONS
The MH initiative in Parma LHA was associated with modest improvements in healthcare utilizations, particularly with lower risk of ED utilization. More research is necessary to understand if ED visit risk will continue to improve and how other aspects of healthcare utilization which may require long-standing effective primary care to improve might change as more MHs open and the length of exposure to MHs increases.
Data Availability
Data for this study was retrieved from the healthcare administrative database of the Local Health Authority of Parma, Italy.
References
American Academy of Family P. Joint principles of the patient-centered medical home. Del Med J. 2008;80(1):21-22.
Lionis C, Petelos E. The patient-centered medical home model within an integrated primary care system: towards a European model? In: O’donohue W. MA, ed. Integrated Primary and Behavioral Care. Springer; 2015.
Ferre F, de Belvis AG, Valerio L, et al. Italy: health system review. Health Syst Transit. 2014;16(4):1-168.
Donatini A. The Italian Health Care System. The Commonwealth Fund. https://international.commonwealthfund.org/countries/italy/. Published 2016. Accessed May 14, 2020.
Italy Ministry of Health. Ministerial Decree 10 July 2007. Projects implementing the National Health Plan - Guidelines for access to co-financing to the regions and autonomous provinces of Trento and Bolzano. http://www.salute.gov.it/imgs/C_17_normativa_1471_allegato.pdf. Published 2007. Accessed February 17, 2020.
Regione Emilia-Romagna. Case della Salute. http://salute.regione.emilia-romagna.it/cure-primarie/case-della-salute. Accessed April 10, 2020.
Regione Emilia-Romagna. Dettaglio Atto Amministrativo. http://servizissiir.regione.emilia-romagna.it/deliberegiunta/servlet/AdapterHTTP?action_name=ACTIONRICERCADELIBERE&operation=leggi&cod_protocollo=GPG/2016/2253&ENTE=1. Accessed April 10, 2020.
Alcusky M, Ferrari L, Rossi G, Liu M, Hojat M, Maio V. Attitudes toward collaboration among practitioners in newly established medical homes: a survey of nurses, general practitioners, and specialists. Am J Med Qual. 2016;31(6):526-535.
Alcusky M, Singer D, Keith SW, et al. Evaluation of care processes and health care utilization in newly implemented medical homes in Italy: a population-based cross-sectional study. Am J Med Qual. 2020;35(3):265-273.
Azienda Unità Sanitaria Locale di Parma. Bilancio di Missione 2011. https://salute.regione.emilia-romagna.it/normativa-edocumentazione/rapporti/archivio/bilanci-di-missione-delle-aziende-sanitarie/ausl_pr_bm2011.pdf. Accessed July 22, 2021.
Jabbarpour Y, DeMarchis E, Bazemore A, Grundy P. The impact of primary care practice transformation on cost, quality, and utilization – a systematic review of research published in 2016. Patient-Centered Primary Care Collaborative. 2017.
Sinaiko AD, Landrum MB, Meyers DJ, et al. Synthesis of research on patient-centered medical homes brings systematic differences into relief. Health Aff (Millwood). 2017;36(3):500-508.
Bronstein JM, Morrisey MA, Sen B, Engler S, Smith WK. Initial impacts of the patient care networks of Alabama initiative. Health Serv Res. 2016;51(1):146-166.
Cuellar A, Helmchen LA, Gimm G, et al. The CareFirst patient-centered medical home program: cost and utilization effects in its first three years. J Gen Intern Med. 2016;31(11):1382-1388.
Maeng DD, Khan N, Tomcavage J, Graf TR, Davis DE, Steele GD. Reduced acute inpatient care was largest savings component of Geisinger Health System’s patient-centered medical home. Health Aff (Millwood). 2015;34(4):636-644.
Peikes D, Anglin G, Taylor E, et al. Evaluation of the comprehensive primary care initiative: third annual report. Math Policy Res. 2016. https://innovation.cms.gov/files/reports/cpci-evalrpt3.pdf. Accessed July 22, 2021.
Shane DM, Nguyen-Hoang P, Bentler SE, Damiano PC, Momany ET. Medicaid health home reducing costs and reliance on emergency department: evidence from Iowa. Med Care. 2016;54(8):752-757.
Moureaux C, Perelman J, Mendes da Costa E, et al. Impact of the medical home model on the quality of primary care: the Belgian experience. Med Care. 2015;53(5):396-400.
Alidina S, Schneider EC, Singer SJ, Rosenthal MB. Structural capabilities in small and medium-sized patient-centered medical homes. Am J Manag Care. 2014;20(7):e265-277.
Flieger SP. Impact of a patient-centered medical home pilot on utilization, quality, and costs and variation in medical homeness. J Ambul Care Manage. 2017;40(3):228-237.
Hinde JM, West N, Arbes SJ, 3rd, Kluckman M, West SL. Did Arkansas’ Medicaid patient-centered medical home program have spillover effects on commercially insured enrollees? Inquiry. 2020;57:46958019900753.
Timbie JW, Hussey PS, Setodji CM, et al. Association between patient-centered medical home capabilities and outcomes for Medicare beneficiaries seeking care from federally qualified health centers. J Gen Intern Med. 2017;32(9):997-1004.
Doescher SM, Skillman MA, Rosenblatt RA. Policy brief: the crisis in rural primary care. Seattle, WA: WWAMI Rural Health Research Center, University of Washington, Apr 2009. https://depts.washington.edu/uwrhrc/uploads/Rural_Primary_Care_PB_2009.pdf. Accessed July 22, 2021.
Baughman AW, Brawarsky P, Onega T, et al. Medical home transformation and breast cancer screening. Am J Manag Care. 2016;22(11):e382-e388.
Kohler RE, Goyal RK, Lich KH, Domino ME, Wheeler SB. Association between medical home enrollment and health care utilization and costs among breast cancer patients in a state Medicaid program. Cancer. 2015;121(22):3975-3981.
Acknowledgements
The authors thank Elena Saccenti, JD, and Giuseppina Frattini, MD, from the Local Health Authority, Parma, Italy.
Funding
The study was supported through a collaborative agreement between the Local Health Authority of Parma and Thomas Jefferson University. The authors’ work was independent of the funders, and this article accurately represents the study results.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
This study was conducted under the auspices of regulation of privacy of the Emilia-Romagna Region N.3 of 24 April 2006 (title: Processing of sensitive data) of act N.1 of 30 May 2014 still in force. This study has been reviewed by the Thomas Jefferson University Institutional Review Board and determined not to constitute human subjects research.
Transparency Statement
Drs. Keith and Maio affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 75 kb)
Rights and permissions
About this article
Cite this article
Keith, S.W., Waters, D., Alcusky, M. et al. The Medical Home Initiative in Italy: an Analysis of Changes in Healthcare Utilization. J GEN INTERN MED 37, 1380–1387 (2022). https://doi.org/10.1007/s11606-021-07040-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07040-9