Abstract
Background
Chronic non-cancer pain (CNCP) is highly prevalent in older adults and long-term opioid therapy (LTOT) has been used to manage chronic pain. However, the safety of LTOT among older adults with CNCP is not well-established and there is a need to identify therapy-related risk factors of opioid-related adverse events among older adults.
Objective
To evaluate the relationship between opioid dose and formulation and the risk of opioid-related adverse events among Medicare-eligible older adults on LTOT.
Design
Nested case-control study.
Participants
Older Medicare beneficiaries (N=35,189) who received > 3 opioid prescriptions with a total days-supply of >45 days within a 90-day period for CNCP between 2012 and 2016.
Main Measures
This study utilized Medicare 5% medical and prescription claims data. Outcome measures included opioid-induced respiratory depression (OIRD), opioid overdose, all-cause mortality, and a composite outcome, defined as the first occurrence of any of the previous three events. Key independent variables were opioid formulation and opioid dose (measured in morphine milligram equivalents (MME)) prescribed during LTOT.
Key Results
Seventy-four OIRD, 133 overdose, 982 all-cause mortality, and 1122 composite outcome events were observed during follow-up. In unadjusted analyses, the use of combination opioids (OR: 4.52 [95%CI: 1.51–13.47]) was significantly associated with OIRD compared to short-acting (SA) opioids. In adjusted analyses, opioid-related adverse events were significantly associated with the use of LA (overdose OR: 13.00 [95%CI: 1.30–130.16] and combination opioids (overdose OR: 6.27 [95%CI: 1.91–20.55]; mortality OR: 2.75 [95%CI: 1.87–4.04]; composite OR: 2.82 [95%CI: 2.01–3.96]) when compared to SA opioids. When compared to an average dose of less than 20 MME, outcomes were significantly associated with doses of 20–50 MME (mortality OR: 1.61 [95%CI: 1.24–2.10]; composite OR: 1.59 [95%CI: 1.26–2.01]) and >50 MME (mortality OR: 1.99 [95%CI: 1.28–3.10]; composite OR: 2.09 [95%CI: 1.43–3.04]).
Conclusions
Older adults receiving medically prescribed opioids at higher doses and those using LA and combination of LA and SA opioids are at increased risks for opioid-related adverse events, highlighting the need for close patient supervision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Chronic non-cancer pain (CNCP) is highly prevalent and often disabling in the older population.1,2,3,4,5,6,7,8,9 Research has shown that more than 3–4% of adults in the USA receive long-term opioid therapy (LTOT) for chronic pain.10 Patients taking high daily doses are more likely to have an overdose event11 and about 3% of the older adults were reported to receive high daily doses (>120 mg morphine equivalents (MME) per day).12 Research has also shown that opioid use in adults of any age is associated with potentially dangerous overdose and other adverse events,11,13,14,15 and the risks can be even higher for older adults.10,16 Recent studies among adults treated for chronic pain have shown a dose-dependent association between opioid use and adverse outcomes, including opioid overdose and opioid-induced respiratory depression (OIRD), which may result in opioid-related mortality.11,17,18,19 Older adults often have reduced renal or hepatic function and reduced respiratory function leading to altered metabolism of opioid drugs, increasing the likelihood of opioid-related adverse outcomes.10,13,20,21
For individuals with chronic pain, the use of long-acting (LA) opioids has increased steadily.22 Musich et al.12 reported that 11.7% of all older adults who utilized LA opioids and high dose opioid users (>120 MME/day) were more likely to use LA opioids compared to lower dose users (≤120 MME/day) (81% vs. 10%). Long-acting opioids are useful in managing chronic pain in patients with consistent pain levels; however, opioid-related adverse outcomes, such as accidental overdoses, are twice as likely to occur in those initiating therapy with LA formulations compared with those starting with short-acting (SA) opioids, particularly in the first 2 weeks of use.23 Because of their advanced age and reduced drug clearance, the use of LA opioids in older adults is of particular concern. However, little is known about the safety of LA opioid use in older adults.24
Given the dearth of knowledge regarding the safety of LTOT among older adults with CNCP, there is a need to provide evidence regarding balancing the benefits and risks of LTOT in older adults and in subpopulations who might be at higher risk for adverse outcomes. The specific aims of this study were to evaluate (1) the relationship between opioid dose and the risk of opioid-related adverse events and (2) the relationship between opioid/formulation and the risk of opioid-related adverse events among Medicare-eligible older adults on LTOT.
METHODS
Study Design and Data Source
This study employed a nested case-control design using a Medicare 5% National Sample data for 2012–2016. The database includes inpatient, outpatient, and pharmacy claims from a random 5% of all Medicare beneficiaries in the USA. The data includes individual demographic characteristics, diagnosis codes, procedure codes, and medication fill claims—all linked by an encrypted beneficiary ID. The study was approved by the Institutional Review Board (protocol #18-069) and the data were licensed for use from the Centers for Medicare and Medicaid Services (DUA #RSCH-2018-52319).
Cohort Definition
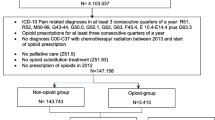
Individuals were considered eligible for cohort entry if they were identified as having a new LTOT use episode between July 1, 2012, and December 31, 2016. A new LTOT use episode was operationalized, based on previous literature,11,25 as the presence of at least three prescription fills for opioid medications totaling 45 cumulative days of supply or more within a 90-day period, immediately preceded by a 6-month period with no history of opioid fills. Individuals were defined to have entered the study cohort on the 91st day after the initiation of the long-term opioid use episode if they met the following inclusion criteria: 65 years or older on the first date of the opioid use; continuously eligible for Medicare parts A, B, and D from 12 months prior to cohort entry until the end of follow-up; have no history of cancer; and have at least two claims for a CNCP condition within a 30-day window in the 12 months before the initiation of the long-term opioid use episode.26,27,28 Please refer to Appendix A (eTable 1) for eligible CNCP conditions used in the study. Individuals entering the study cohort remained in the cohort until the occurrence of an outcome of interest, mortality, first occurrence of cancer, loss of Medicare eligibility, or the end of the study period, whichever was earlier.
Case Definition
This study examined multiple opioid-related adverse events—opioid-induced respiratory depression (OIRD), opioid overdose, mortality, and a composite outcome, which was defined as the first occurrence of any of the previous three events.11,14,18,29 Separate cases and matching controls were defined for each of the events: individuals from the eligible cohort who had a confirmed episode of either OIRD, opioid overdose, or death before the end of the study period were defined as cases. The date of the first occurrence of an event was defined as the index date. OIRD was operationalized, from existing literature, as a listed International Classification of Diseases (ICD) code for prescription opioid-related poisoning along with a Current Procedure Code (CPT) for at least one of the following event occurring within ± 1 day of the opioid-related poisoning: (1) life-threatening respiratory or central nervous system depression; (2) mechanical ventilation; or (3) critical care.14,29 Opioid-related overdose was also operationalized based on existing literature as follows: (1) ICD code for opioid-related poisoning; or (2) ICD code for an opioid-related adverse event plus an ICD code for opioid overdose on the same day of the opioid-related adverse event.11 This study measured all-cause mortality as Medicare claims data do not include information regarding causes of death. All ICD and/or CPT codes (see Appendix eTables 2 and 3) 11,14,29 were identified from Medicare Provider and Analysis Review, Outpatient Standard Analytical file, and Medicare Carrier files, and all primary and non-primary codes were considered. All-cause mortality was identified from Medicare Master Beneficiary Summary File (MBSF).
Control Selection
Controls were defined as individuals from the study cohort who had not been identified to have an opioid-related adverse event as of the index date. One control was selected for each case using incidence-density sampling30 (Fig. 1). This method allows for random sampling from the pool of eligible controls, such that each control subject had an equal or greater time at risk of an adverse event (i.e., time from the 91st day after opioid initiation until adverse event or end of follow-up) than the matched case. This technique allows for controls to serve as a future case and allows for one individual to serve as a control for more than one case. Matching was conducted on age (±1 year) and time of cohort entry (±30 days). Each control was assigned the index date of their matched case. In addition to previously mentioned eligibility criteria, cases and controls were also required to be on LTOT in the 90 days prior to index date.
Opioid Variables
The key independent variables were dose and formulation of opioids prescribed during LTOT. Both independent variables were measured during the 90 days prior to index date. Opioid dose was defined as the average daily dose of opioids prescribed, measured in MME, and captured using prescription records present in the Medicare prescription drug event file. MME was calculated as per established CMS criteria31 and categorized into three groups: less than 20 MME; 20 to 50 MME; and at least 50 MME. These thresholds were chosen based on CDC guidance and previous research.32 The formulation of opioids was defined as the presence of prescription fills for SA opioids only, LA opioids only, or both SA and LA opioids (combination opioid) during the prior 90 days.33 Opioid formulation was identified using the dosage form code and generic names.
Confounding Variables
Potential confounders included demographic variables, comorbidities, and use of other medications. The demographic variables included in the model, identified from the MBSF, were race, sex, region of residence, and Medicare low-income subsidy (LIS) status. Comorbidities of interest included the presence of multiple CNCP conditions, Parkinson’s disease, renal insufficiency, hepatic insufficiency, mental illnesses, hypnotic medication dependence, substance use disorder, history of overdose, history of respiratory depression, COPD, sleep apnea, or other sleep disorders at any time prior to index date. Comorbidities were identified using ICD codes (Appendix eTable 4) from any Medicare claims files. Medication-related covariates were defined as present if the individual was found to have at least 30 days of supply for medications belonging to any of the following classes during the 90-day hazard period: adjuvant analgesics (such as NSAIDs), anti-convulsants, antidepressants, sedative-hypnotics (non-benzodiazepine receptor agonists, short-acting benzodiazepine receptor agonists, intermediate-acting benzodiazepine receptor agonists and selective melatonin agonists) benzodiazepines, muscle relaxants, or gabapentin. The Deyo-Charlson comorbidity index (CCI) score34 was also calculated based on all available claims prior to the index date.
Statistical Analysis
Data management and analysis were conducted using SAS version 9.4 (Cary, NC). Four different analytic datasets were constructed for each of the four outcomes in the study (OIRD, opioid overdose, mortality, and a composite outcome). For each outcome, individual characteristics of cases and controls were compared using paired samples t-tests, McNemar’s test and Cochran-Mantel-Haenszel test, as appropriate. The relationship between the key independent variables and the outcomes was tested using conditional logistic regression to account for the case-control matching. Both adjusted and unadjusted models were tested where the adjusted models included all the proposed covariates.
RESULTS
Study Cohort
A total of 35,189 Medicare beneficiaries were identified as new LTOT users. Of these beneficiaries 24,342 (69%) were female, 29,321 (83%) were whites, and 15,054 (43%) had a low-income status. The mean age of the cohort was 77 years; within the cohort, we observed 74 OIRD, 133 overdose, and 982 all-cause mortality events during follow-up. The composite outcome of OIRD, opioid overdose, or mortality was experienced by 1122 patients. Detailed patient demographic and clinical characteristics by outcome measures are presented in Table 1. After the selection of matched cases and controls, the median duration of time between cohort entry and the index date for study subjects who experienced an OIRD, overdose, mortality, and the composite outcome was 272.5 days (IQR: 48.5–497.5), 368.5 days (IQR: 136–647), 241 days (IQR: 76–498.5), and 254.5 days (IQR: 77–519), respectively.
Outcomes
Unadjusted Analysis
Table 2 provides unadjusted results of the conditional logistic regression models. We found that opioid use of average MME > 50 (OR = 3.59 [95%CI: 1.01–12.83]) was positively associated with OIRD relative to opioid dosage of <20 MME. The use of combination opioids (OR = 4.52 [95%CI: 1.51–13.47]) was also found to be positively associated with OIRD relative to SA opioids. Opioid dose of average 20–50 MME (OR = 2.60 [95%CI: 1.25–5.41]) and combination opioid formulation (OR = 3.39 [95%CI: 1.59–7.22]) were significantly associated with opioid overdose relative to opioid dosage of <20 MME and SA opioids, respectively. Using opioids with an average dose > 50 MME (OR = 1.60 [95%CI: 1.13–2.27]), use of LA opioid (OR = 1.65 [95%CI: 1.01–2.68]), and use of combination opioid formulation (OR = 3.26 [95%CI: 2.38–4.47]) were significantly associated with all-cause mortality opioid use of 20–50 average MME (OR = 1.46 [95%CI: 1.20–1.78]) and > 50 average MME (OR = 1.83 [95%CI: 1.33–2.50]), and combination opioid formulation (OR = 2.90 [95%CI: 2.19–3.83]) were all significantly associated with the composite outcome compared to opioid dosage of <20 MME and SA opioids, respectively.
Adjusted Analysis
Table 3 presents the adjusted results of the conditional logistic regression models. After adjusting for all control variables, the use of LA opioids (OR = 13.00 [95%CI: 1.30–130.16]) and combination opioids (OR = 6.27 [95% CI: 1.91–20.55]) were found to be significantly associated with opioid overdose compared to SA opioids. We also found that opioid dosage of 20-50 MME and > 50 MME had 61% (OR = 1.61 [95%CI: 1.24 –2.10]) and 99% (OR = 1.99 [95%CI: 1.28–3.10]) higher odds of all-cause mortality, respectively relative to opioid dosage of <20 MME. Combination opioid formulation (OR = 2.75 [95%CI: 1.87–4.04]) was also found to be significantly associated with mortality compared to SA opioids. Regarding the composite outcome, we found that opioid dosage of 20–50 MME had 1.59 times higher odds (OR = 1.59 [95% CI 1.26–2.01]) and > 50 MME had 2.09 times higher odds (OR = 2.09 [95%CI: 1.43–3.04]) of the composite outcome relative to opioid dosage of <20 MME. The use of combination opioids (OR = 2.82 [95%CI: 2.01–3.96]) was also significantly associated with the composite outcome compared to SA opioids. Because the small sample size of the OIRD outcome prohibited multivariable adjustment of the relationship of interest, results of the adjusted model for OIRD were not reported.
DISCUSSION
This nested case-control study examined associations between opioid dose and opioid formulation and the risk of opioid-related adverse events among older adults with CNCP on LTOT using the 5% national sample of Medicare administrative claims data. After adjusting for all control variables, opioid formulation, i.e., the use of LA opioids alone, was a significant risk factor for opioid overdose and use of LA and SA opioids was a significant risk factor for overdose, all-cause mortality and the composite outcome when compared to using SA opioids alone. Additionally, opioid dose of 20–50 MME and > 50 MME were significant risk factors for all-cause mortality and the composite outcome of OIRD, opioid overdose, and all-cause mortality compared to opioid dose < 20 MME. These results are consistent with the findings from previous studies.11,17,29,35 For example, Dunn et al.11 report that overdose risk is higher in patients receiving medically prescribed LTOT at higher doses. Zedler et al.29 reported that patients receiving LA opioids had significantly higher odds of OIRD compared to those not receiving LA opioids. They also report that patients with daily MME >100 had significantly higher odds of OIRD compared to patients with <100 daily MME. The current study adds to the literature of opioid safety, by examining these relationships in older adults receiving LTOT. Improper use of any opioid can cause serious adverse effects including overdose and mortality, and this risk can be significantly higher with the use of extended release or LA opioids. Although LA opioids may be able to provide more consistent and prolonged pain relief,27 their unique pharmacokinetic profiles make them riskier than short-acting opioids.36 Therefore, the CDC recommends that extended release and LA opioids be reserved for patients with severe and continuous pain only.10 In addition, older adults may be at higher risk for opioid overdose, OIRD and other adverse effects when prescribed LA opioids because their reduced renal or hepatic function can lead to decreased drug clearance from the body.10,16,21 On the other hand, SA opioids are generally indicated for the management of acute and breakthrough pain. When LA opioids are used concomitantly with SA opioids, it is possible that the sudden increase in plasma opioid concentrations may increase the risk of opioid-related adverse events,27 as shown in the current study.
This study also finds that compared to opioid dosage of less than 20 MME, higher daily dosage is a significant predictor of all-cause mortality and the composite outcome among older adults with CNCP. Although there is no absolutely safe dose for LTOT, previous research shows that regardless of patient age, the risk of opioid-related adverse outcomes increases with increasing doses.11,14,17 The CDC guideline for prescribing opioids for chronic pain also recommends that clinicians should start patients with the lowest effective opioid dose, great caution has to be exercised when considering increasing opioid dosage to ≥50 MME/day, and opioid dosage of ≥90 MME/day should be generally avoided.10 Therefore, the choice of opioid formulations and dose should be individualized, balancing the patient’s need for continued pain relief and the risk of opioid-related adverse events.27 Finally, this study examined a variety of outcomes—two opioid-related events and all-cause mortality—and found that the effect of the key independent variables was largely consistent with hypotheses and robust to covariate adjustment. Even though we were unable to compute adjusted estimates for OIRD, the adjusted results compared to the unadjusted results for the other outcomes provide reasonable confidence in our findings.
This study has several limitations. First, as in all analyses using insurance claims databases, we had restricted capacity to adjust for the severity of diseases including substance use disorders, physical illnesses, and psychiatric illnesses, which may possibly place patients at increased risk of opioid-related adverse events regardless of the opioid regimen. Second, our reported opioid-related adverse event rates may be an underestimate of the actual event rates as some opioid-related adverse events may go unreported if patients die without seeking medical attention or receive medical attention that is not reimbursed by Medicare. As we do not have a priori reason to believe that the ascertainment of outcomes would be biased with respect to opioid dose or formulation, the relative risks that we report are not likely to be affected by this limitation. Third, administrative claims data do not capture all known predictors, such as behavioral and social characteristics, family history and genotype, opioids obtained from other sources, illicit substance use, and other details regarding opioid indications (e.g., analgesia vs medication-assisted treatment of opioid use disorder) or nonopioid medication. Although we adjusted for all potential confounders, the possibility of residual confounding cannot be excluded. Fourth, due to the low event rates for outcomes of OIRD and opioid overdose, the estimates for these outcomes should be interpreted with caution. Finally, this study only evaluated the impact of LTOT as operationalized through the 90-day window. However, the risk of adverse outcomes is probably also influenced by short-term changes in dose and formulation or by the total duration of LTOT. Future studies should investigate the impact of these factors.
CONCLUSION
We observed increased risk for opioid-related adverse events in older adults receiving LTOT at higher doses, and those using LA and the combination of LA and SA opioids relative to those using only SA opioids. Because of inadequate evidence regarding benefits and risks, LTOT should be prescribed to older adults with caution, and a plan of close monitoring and periodic reassessing of the benefits and risks of opioid therapy should be in place.
References
Papaleontiou M, Henderson CR, Turner BJ, et al. Outcomes associated with opioid use in the treatment of chronic non-cancer pain among older adults: a systematic review and meta-Analysis. J Am Geriatr Soc. 2010;58(7):1353-1369. doi:https://doi.org/10.1111/j.1532-5415.2010.02920.x
Stompór M, Grodzicki T, Stompór T, Wordliczek J, Dubiel M, Kurowska I. Prevalence of chronic pain, particularly with neuropathic component, and its effect on overall functioning of elderly patients. Med Sci Monit. 2019;25:2695-2701. doi:https://doi.org/10.12659/MSM.911260
Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17(3):417-431, v. doi:https://doi.org/10.1016/s0749-0690(05)70078-1
Soldato M, Liperoti R, Landi F, et al. Non malignant daily pain and risk of disability among older adults in home care in Europe. Pain. 2007;129(3):304-310. doi:https://doi.org/10.1016/j.pain.2006.10.016
Gianni W, Ceci M, Bustacchini S, et al. Opioids for the treatment of chronic non-cancer pain in older people. Drugs Aging. 2009;26(1):63-73. doi:https://doi.org/10.2165/11534670-000000000-00000
Fine PG. Long-term consequences of chronic pain: mounting evidence for pain as a neurological disease and parallels with other chronic disease states. Pain Med. 2011;12(7):996-1004. doi:https://doi.org/10.1111/j.1526-4637.2011.01187.x
Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457-467. doi:https://doi.org/10.2147/JPR.S105892
Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69(2):197-207. doi:https://doi.org/10.1037/a0035794
Reid MC, Eccleston C, Pillemer K. Management of chronic pain in older adults. BMJ. 2015;350:h532. doi:https://doi.org/10.1136/bmj.h532
CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65. doi:https://doi.org/10.15585/mmwr.rr6501e1er
Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85-92. doi:https://doi.org/10.7326/0003-4819-152-2-201001190-00006
Musich S, Wang SS, Slindee L, Kraemer S, Yeh CS. Prevalence and characteristics associated with high dose opioid users among older adults. Geriatric Nursing. 2019;40(1):31-36. doi:https://doi.org/10.1016/j.gerinurse.2018.06.001
Solomon DH. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170(22):1968. doi:https://doi.org/10.1001/archinternmed.2010.391
Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911-1929. doi:https://doi.org/10.1111/pme.12480
Nadpara PA, Joyce AR, Murrelle EL, et al. Risk factors for serious prescription opioid-induced respiratory depression or overdose: comparison of commercially insured and veterans health affairs populations. Pain Med. 2018;19(1):79-96. doi:https://doi.org/10.1093/pm/pnx038
Ginsburg M, Silver S, Berman H. Prescribing opioids to older adults: a guide to choosing and switching among them. Geriatrics and Aging. 2009;12(1):5.
Bohnert ASB, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321. doi:https://doi.org/10.1001/jama.2011.370
Gomes T, Mamdani MM, Paterson JM, Dhalla IA, Juurlink DN. Trends in high-dose opioid prescribing in Canada. Can Fam Physician. 2014;60(9):826-832.
Els C, Jackson TD, Kunyk D, et al. Adverse events associated with medium- and long-term use of opioids for chronic non-cancer pain: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;(10). doi:https://doi.org/10.1002/14651858.CD012509.pub2
Guerriero F. Guidance on opioids prescribing for the management of persistent non-cancer pain in older adults. World J Clin Cases. 2017;5(3):73-81. doi:https://doi.org/10.12998/wjcc.v5.i3.73
American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons, Reprinted with permission from The American Geriatrics Society. Original article appears in J Am Geriatr Soc 2009; 57: 1331–1346. “Pharmacological management of persistent pain in older persons.” Pain Med. 2009;10(6):1062-1083. doi:https://doi.org/10.1111/j.1526-4637.2009.00699.x
Ray JB. Implications of the extended-release/long-acting opioid REMS for managed care. Am J Manag Care. 2015;21(9):12.
Schieber LZ, Guy GP, Seth P, et al. Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006-2017. JAMA Netw Open. 2019;2(3):e190665. doi:https://doi.org/10.1001/jamanetworkopen.2019.0665
Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of long-acting opioids and mortality in patients with chronic noncancer pain. JAMA. 2016;315(22):2415-2423. doi:https://doi.org/10.1001/jama.2016.7789
Ramachandran S, Salkar M, Bentley JP, Eriator I, Yang Y. Pattern of use and geographic variation in long-term prescription opioid use among older adults in the United States: a study of Medicare administrative claims data [in press]. Pain Physician.
Reid MC, Bennett DA, Chen WG, et al. Improving the pharmacologic management of pain in older adults: identifying the research gaps and methods to address them. Pain Med. 2011;12(9):1336-1357. doi:https://doi.org/10.1111/j.1526-4637.2011.01211.x
Argoff CE, Silvershein DI. A comparison of long- and short-acting opioids for the treatment of chronic noncancer pain: tailoring therapy to meet patient needs. Mayo Clin Proc. 2009;84(7). Accessed September 1, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2704132/.
Sullivan MD, Edlund MJ, Fan M-Y, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000-2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440-449. doi:https://doi.org/10.1016/j.pain.2008.04.027
Zedler BK, Saunders WB, Joyce AR, Vick CC, Murrelle EL. Validation of a screening risk index for serious prescription opioid-induced respiratory depression or overdose in a US commercial health plan claims database. Pain Med. 2018;19(1):68-78. doi:https://doi.org/10.1093/pm/pnx009
Richardson DB. An incidence density sampling program for nested case-control analyses. Occup Environ Med. 2004;61(12):e59-e59. doi:https://doi.org/10.1136/oem.2004.014472
Centers for Medicare and Medicaid Services. Opioid oral morphine milligram equivalent (MME) conversion factors. [online]. Published online August 2017. Accessed October 10, 2020. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf
Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Calculating total daily dose of opioids for safer dosage. Accessed October 10, 2020. https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf
Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use — United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265-269. doi:https://doi.org/10.15585/mmwr.mm6610a1
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Clin Epidemiol. 1987;40(5):373-383.
Miller M, Barber CW, Leatherman S, et al. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175(4):608-615. doi:https://doi.org/10.1001/jamainternmed.2014.8071
Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363(21):1981-1985. doi:https://doi.org/10.1056/NEJMp1011512
Funding
This work was supported by the National Institute on Drug Abuse R15DA046036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors of this manuscript have no conflict of interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 30.7 kb)
Rights and permissions
About this article
Cite this article
Salkar, M., Ramachandran, S., Bentley, J.P. et al. Do Formulation and Dose of Long-Term Opioid Therapy Contribute to Risk of Adverse Events among Older Adults?. J GEN INTERN MED 37, 367–374 (2022). https://doi.org/10.1007/s11606-021-06792-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06792-8