Abstract
Background
Many outpatients with functional dyspepsia (FD) do not follow the medication schedule recommendations, which can lead to illness relapse.
Objective
To investigate whether short message service (SMS) reminders improve medication regimen adherence and therapeutic efficacy in outpatients with FD.
Design
Participants with FD were randomly allocated to the control group or intervention group. Patients in the control group received a 4-week medication treatment with no reminders, those in the intervention group received medication treatment plus a daily SMS reminder of dose and medication time.
Participants
Newly diagnosed FD patients from April 2019 to June 2019 were recruited from the GI outpatient clinics at Renji Hospital.
Measurements
The scores for FD symptoms (LDQ) and psychological conditions (PHQ-9 for depression and GAD-7 for anxiety) were assessed before and after the treatment. The medication possession ratio (MPR) was calculated.
Key Results
A total of 352 eligible patients was enrolled in the study. The overall compliance rates of patients in the intervention and control groups were 87.5% and 80.7% in the intention-to-treat (ITT) analysis (P = 0.08) and 94.48% and 86.59% in per-protocol (PP) analysis (P = 0.015), respectively. In the intervention group, the compliance rate of younger patients (age ≤ 40 years) was significantly higher than that of age-matched patients in the control group (ITT: 86.1% vs. 70.5%, P = 0.018). Compared with the control group, the reduction in scores of LDQ (9.33 vs. 8.02, P = 0.017), PHQ-9 (6.97 vs. 5.69, P = 0.004), and GAD-7 (8.70 vs.7.53, P = 0.028) was significantly greater in patients receiving SMS reminders. The MPR of patients positively correlated with the reduction in scores of LDQ, PHQ-9, and GAD-7 in both groups.
Conclusions
SMS reminders can improve treatment compliance and efficacy in patients with FD.
Trial Registration
NCT04052750
Similar content being viewed by others
INTRODUCTION
Functional dyspepsia (FD) is one of the most prevalent functional gastrointestinal disorders (FGIDs). It is characterized by one or more of the following symptoms that are unexplained after a routine clinical evaluation: postprandial fullness, early satiation, epigastric pain, and epigastric burning.1, 2 FD is a common condition seen in the clinical practice of gastroenterologists.3 It poses significant burdens to patients due to consultations, medications, and sickness-related absences from work.4,5,6 Currently, the main treatment options include drug therapy, psychotherapy, and nutritional diet therapy.4,5,6 Although high-quality evidence supporting the use of medication regimens is lacking, pharmacotherapy including acid-suppressive drugs and prokinetics forms one of the pillars of FD treatment.1 Guidelines recommend the use of neuromodulators (such as antidepressants) in FD patients not responding to acid-suppressive drugs and prokinetics.7 The maximum benefit of medications can be achieved only if patients adhere to the prescribed treatment regimen.8 Effective treatment for FD requires patients to take multiple drugs daily for a specific duration (at least 4 weeks), especially for those with severe symptoms.1, 9 However, less than half of outpatients with FD adhere to physician recommendations of the medication schedules given by physicians.10 Non-adherence to prescribed medications could greatly reduce the chance of treatment success, precluding a proper evaluation of therapeutic efficacy. Therefore, we conducted a prospective randomized controlled study to investigate whether short message service (SMS) reminders could improve the treatment compliance rate and therapeutic efficacy in patients with FD.
MATERIALS AND METHODS
Patients and Study Design
This was a prospective, physician-blinded, and randomized study. A total of 352 consecutive patients who were newly diagnosed with FD from April 2019 to June 2019 were recruited from the GI outpatient clinics at Renji Hospital. The inclusion criteria were as follows: 18–65 years old; education level no lower than middle school; met the Rome IV criteria for FD; absence of abnormalities on physical examination, laboratory tests (including a routine blood test, blood glucose, and liver function examination), and abdominal imaging and GI endoscopy; and the absence of Helicobacter pylori infection. Patients were excluded if they were younger than 18 years old or older than 65 years old; were allergic to the treatment medication; had evidence of organic GI disease; had a psychiatric disease or taking psychotropic drugs for indications other than FD; had severe diseases of other systems; were lactating, pregnant, or planning pregnancy; or lacked capacity. The study protocol and informed consent form were approved by the Medical Ethics Committee of Renji Hospital (Approval No. KY2019032), and the study was registered on clinicaltrials.gov (NCT04052750). An informed consent form was obtained from each participant.
Randomization and Intervention
Eligible patients were randomly allocated to the intervention group or the control group for 4 weeks. The randomization sequence was prepared by an independent researcher according to the computer-generated random number tables. In order to reduce bias and achieve balance, a permuted-block design (with variable block size) was used in the allocation of participants to study arms. The participants’ basic information and symptoms were recorded before the intervention began. Prescribing physicians were blinded to the study. All patients received standard treatments for FD. Treatment was the discretion of the prescribing physician and included proton-pump inhibitors (PPIs), H2 receptor blockers, and prokinetics as well as antidepressants. Prescribing physicians were blinded to the study. Patients in the intervention group received daily SMS instructions of medication dosage and time about dyspeptic medications prescribed at the outpatient clinic. The control group received only treatment with no reminders. The SMS reminder was sent using an automated system (Red Maple Leaf Media Ltd, Shanghai, China) at the time when medication needed to be taken. The messages included medication dose and time about the drugs prescribed at the outpatient clinic.
Outcome Measures
The primary endpoint of this study was medication adherence to the dyspepsia drugs. The major classes of medications used by the enrolled subjects consisted of the regular first-line therapy, i.e., non-psychiatric medications including PPIs (n = 314, 89.2%), H2 receptor blockers (n = 210, 59.66%), prokinetic agents (n = 117, 33.24%), and psychiatric medications (antidepressants; n = 282, 80.11%). Nearly all the patients received multiple medications. Adherence was evaluated by pill count, using the medication possession ratio (MPR),11 defined as the number of drugs taken by the patient during the follow-up period relative to the amount prescribed. The numerator for MPR was the number of medications taken by patients during the observation period. The MPR denominator was the number of drugs required during the observation period for 100% adherence and was defined as the number of drugs required per day multiplied by the days of the observation period. The start of the observation was defined as the date on which the corresponding medication was first prescribed. The end of the observation was the date of follow-up. If a patient used more than one drug, the MPR was calculated with the sum of all the FD drugs. MPR ≥ 80% was defined as the threshold for which patients were considered adherent to therapy. Poor compliance was defined as taking less than 80% of prescribed dyspepsia drugs. The percentage of compliant patients in each group was calculated by dividing the number of compliant patients (MPR ≥ 80%) by the total numbers of enrolled patients after the 4-week treatment period. The secondary endpoint was the therapeutic efficacy. Dyspeptic symptoms of patients were assessed using Leeds Dyspepsia Questionnaire (LDQ). Psychological symptoms were assessed using Patient Health Questionnaire Depression Scale (PHQ-9) and Generalized Anxiety Disorder Scale (GAD-7). The patients were asked to fill out a corresponding questionnaire before the treatment. A standardized follow-up phone call was performed at the end of the 4-week treatment to evaluate the patient’s condition. Patients’ missing dosages, symptoms, and adverse drug reactions (ADRs) were recorded through the standard self-report questionnaires.
Statistical Analysis
Drug efficacy and treatment compliance were analyzed based on the intent-to-treat (ITT) population, which included all the enrolled subjects, and on a per-protocol (PP) population. Subgroup analyses of patients of different ages were not pre-specified. Our sample size of 176 patients per arm was based on a 10% difference in the SMS reminder group with a significance level of 0.05 (α) and a power of 80% (1 − β) in the two-side test, assuming 10% of withdrawing or loss to follow-up.
SPSS software V.25.0 (IBM Corp., Armonk, NY, USA) was used to perform all statistical analyses. Categorical data were analyzed with chi-square test, or Fisher exact tests if appropriate. Continuous variables were analyzed with Student’s t test. Spearman’s correlation analysis was used to determine the association of medication compliance with symptom improvement or other variables. The participants who were lost to follow-up, withdrew due to adverse reactions, and did not take medicine according to the physician’s advice were excluded in the per-protocol analysis. Each participant who had finished the follow-up phone call at the end of the fourth week was included in the compliance assessment. A P value < 0.05 was considered statistically significant. Normally distributed data were expressed as mean ± SD.
RESULTS
Subjects
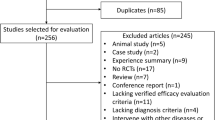
A total of 352 consecutive patients with FD were included and randomly assigned to the control or intervention groups. The flow of screening and recruitment of study subjects is shown in Figure 1. The subjects were all included in the ITT analysis; 327 subjects completed the treatment (164 in the control group and 163 in the intervention group) and were analyzed as the per-protocol group. Groups were well-balanced in terms of demographic and baseline clinical characteristics (Table 1).
Compliance with Medication Treatment
There was no difference in the ITT analysis (n = 176), in the proportion of compliant patients (MPR ≥ 80%) between the intervention and control groups for FD medications (87.5% vs. 80.7%, P = 0.08), though the PP analysis (n = 164) suggested improvement with the intervention (94.5% vs. 86.6%, P = 0.02; Table 2). Subgroup ITT analysis showed that the proportion of compliant patients was higher for non-psychiatric FD drugs compared with the control group (88.0% vs. 78.0%, P = 0.02; Table S1), but not for psychotropic FD drugs (85.7% vs. 77.5%, P = 0.07). Compliance was also significantly higher in patients 40 years and younger between the intervention and control groups (86.1% vs. 70.5%, P = 0.02), though not in older patients (88.7% vs. 88.8%, P = 0.98; Table 2). Patients younger than 40 had higher educational attainment than older patients (P < 0.001; Fig. 2a).
a Education time of patients with different ages (≤ 40 years or 41–65 years) in the control group and intervention group. Data are presented as mean ± SD. ***P < 0.001 (Student’s t test). b The changes in symptom scores after the 4-week treatment in the control group (n = 164) and intervention group (n = 163). *P < 0.05, **P < 0.01 (Student’s t test).
Outcomes of Treatment
The symptom scores decreased significantly compared with baseline in both the control group (n = 164) and the intervention group (n = 163) after a 4-week treatment (P < 0.001; Table 3). Compared with the control group, the change in LDQ scores was greater in the intervention group than in the control group (9.33 vs. 8.02; P = 0.017), indicating a better treatment response of this group. The scores of PHQ-9 (for depression) and GAD-7 (for anxiety) in each group also significantly decreased after a 4-week treatment (P < 0.001 compared with baseline; Table 3). The improvement in these scores in the intervention group was significantly greater than that in the control group (P < 0.05; Fig. 2b).
Relationship Between Medication Compliance and Symptom Improvement
Spearman’s correlation analysis revealed that the MPR of patients positively correlated with the reduction in scores of LDQ (control group: r = − 0.494, P < 0.001; intervention group: r = − 0.246, P = 0.002), PHQ-9 (control group: r = − 0.213, P = 0.006; intervention group: r = − 0.158, P = 0.045), and GAD-7 (control group: r = − 0.496, P < 0.001; intervention group: r = − 0.276, P < 0.001) in both groups (Table 4). We also analyzed the correlations between the baseline characteristics of patients and their MPR. As shown in Table 5, the baseline scores of depression negatively correlated with medication compliance in the control group (control group: r = − 0.195, P < 0.05; intervention group: r = 0.074, P = 0.345). On the contrary, the baseline scores of anxiety positively correlated with medication compliance in the control group (r = 0.213, P < 0.01; intervention group: r = 0.051, P = 0.518).
Adverse Events
The rate of overall ADRs was 1.14% (2/176) in the control group and 1.7% (3/176) in the intervention group (P > 0.99; Table S2). Generally, the incidence of side effects was low, with five participants withdrawing because of intolerable side effects. The majority of these adverse events were of mild or moderate intensity and resolved after the termination of the study. No life-threatening ADRs occurred.
DISCUSSION
Overall, we found that the SMS intervention significantly improved dyspepsia and depressive and anxiety symptoms. Overall, the intervention did not improve adherence (though it increased adherence for non-psychiatric FD drugs) and appeared to be dependent on the participants’ age. Those less than 40 had significant improvement in adherence to medications. Moreover, the intervention improved adherence to non-psychiatric FD medications, such as PPIs, H2 antagonists, and prokinetics, but not to FD antidepressant treatment. Generally, medication adherence was high in both groups, with approximately more than 80% of subjects reporting good adherence, especially in elderly patients.
Our results are consistent with other studies. Providing patients with some forms of reminder such as SMS reminders on mobile phones helps to enhance antiretroviral adherence.12 A meta-analysis shows that mobile phone SMS messages could double the odds of medication adherence in chronic diseases such as hypertension.13 As growing numbers of individuals use mobile phones around the world, mobile phone–based interventions are appealing.14, 15 Compared with telephone, short messages consume less time and human resources and can be easily integrated into patients’ lives.16 Therefore, a short message reminder may be a more suitable method for promoting compliance in the treatment of FD.
These findings are similar to those of other studies investigating treatment adherence in FD.17 Similar to the findings in a previous study on adherence to proton-pump inhibitors,18 younger participants in the control group displayed lower compliance (reflected as a lower percentage of compliant patients and a lower average age of non-compliant patients) compared with those aged 41–65 years. Interestingly, this population showed a better response to SMS reminders, with an increased percentage of compliant patients (ITT: P = 0.018 vs. control group) than that in the control group. While dyspepsia is not age-related, younger people use mobile phones more frequently,19 and may be more responsive to short message reminding. In addition, older patients are more likely to be taking medications regularly, and may need less reminding. Another explanation may involve the education level; younger patients had higher education. However, whether education level is associated with treatment compliance needs further research. Different from the results obtained in young patients, a high percentage of older patients who are compliant regardless of the arm of the study were observed, indicating that SMS may not be necessary nor useful in older patients with FD.
Patients with FD often exhibit higher levels of anxiety, depression, and other psychological conditions.20 Some researchers have reported that psychotropic drugs such as antidepressants appear to be an effective treatment for FD.21,22,23 We found that SMS reminders did not increase the proportion of compliant patients for psychotropic FD drugs. There are a number of possible reasons for this including side effects24 and stigma.25 Improved communication, including acknowledging and addressing the concerns of FGID patients about pharmacotherapeutic regimens, could potentially improve adherence.26, 27 In our study, adherence to psychotropic drugs did not improve. It may be necessary to look for other strategies to improve adherence to psychotropic agents in FD therapy.
While there was minimal improvement in adherence, there was significant improvement of FD symptoms and comorbid psychological symptoms in both groups, significantly greater in those receiving SMS reminders. The MPR of patients in both groups was positively correlated with symptom improvement. The correlation was stronger in patients in the controls than those in the intervention group. While our intervention did not improve adherence, it may have impacted on patients’ anxiety and depressive symptoms; the SMS messages may have been therapeutically reassuring. Much of the benefit may be from a type of social support and feedback to patients about the disease that may make them feel better.
Our study is not without limitations. First, some patients may need to take medications for FD for more than 4 weeks (often 6–8 weeks) to achieve a clinical effect. Therefore, a longer follow-up period may be needed. Second, an 7% improvement in adherence may be clinically meaningful; our study was underpowered to show this difference to be statistically significant. Third, there was heterogeneity in treatment; this diversity might impact our outcomes, though most of the first-line agents have relatively few adverse effects. Fourth, patients were not blinded in this study. Fifth, compliance was high in both the control and intervention groups. Our intervention could be more effective in a population with lower adherence. Sixth, we focused exclusively on functional dyspepsia; whether this intervention could be more effective in other conditions, such as hypertension (where adherence is generally low), is unknown. Finally, our study was entirely conducted in China and may not be generalizable to other populations.
In conclusion, our study demonstrated that SMS reminders on cell phones could meaningfully improve treatment compliance and had a significant impact on symptom outcomes in patients with FD. Sending SMS reminders on cell phones is economical and easy to do. Daily SMS reminders could be a useful and feasible tool in enhancing treatment compliance of FD patients.
References
Enck P, Azpiroz F, Boeckxstaens G, et al. Functional dyspepsia. Nat Rev Dis Primers. 2017;3:17081.
Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal Disorders. Gastroenterology. 2016;150:1380-92.
Ford AC, Marwaha A, Sood R, et al. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut. 2015;64:1049-57.
Lee OY. Asian motility studies in irritable bowel syndrome. J Neurogastroenterol Motil. 2010;16:120-30.
Dekel R, Drossman DA, Sperber AD. The use of psychotropic drugs in irritable bowel syndrome. Expert Opin Investig Drugs. 2013;22:329-39.
Staudacher HM, Lomer MC, Anderson JL, et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012;142:1510-8.
Moayyedi PM, Lacy BE, Andrews CN, et al. Corrigendum: ACG and CAG Clinical Guideline: Management of Dyspepsia. Am J Gastroenterol. 2017;112:1484.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-97.
Moayyedi P, Delaney BC, Vakil N, et al. The efficacy of proton pump inhibitors in nonulcer dyspepsia: a systematic review and economic analysis. Gastroenterology. 2004;127:1329-37.
Cassell B, Gyawali CP, Kushnir VM, et al. Beliefs about GI medications and adherence to pharmacotherapy in functional GI disorder outpatients. Am J Gastroenterol. 2015;110:1382-7.
Peterson AM, Nau DP, Cramer JA, et al. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10:3-12.
Reid MJ, Dhar SI, Cary M, et al. Opinions and attitudes of participants in a randomized controlled trial examining the efficacy of SMS reminders to enhance antiretroviral adherence: a cross-sectional survey. J Acquir Immune Defic Syndr. 2014;65:e86-8.
Thakkar J, Kurup R, Laba TL, et al. Mobile Telephone Text Messaging for Medication Adherence in Chronic Disease: A Meta-analysis. JAMA Intern Med. 2016;176:340-9.
Vervloet M, Linn AJ, van Weert JC, et al. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19:696-704.
Castaldelli-Maia JM, Scomparini LB, Andrade AG, et al. Perceptions of and attitudes toward antidepressants: stigma attached to their use--a review. J Nerv Ment Dis. 2011;199:866-71.
Lee YJ, Kim ES, Choi JH, et al. Impact of reinforced education by telephone and short message service on the quality of bowel preparation: a randomized controlled study. Endoscopy. 2015;47:1018-27.
Krol N, Muris JW, Schattenberg G, et al. Use of prescribed and non-prescribed medication for dyspepsia. Scand J Prim Health Care. 2004;22:163-7.
Van Soest EM, Siersema PD, Dieleman JP, et al. Persistence and adherence to proton pump inhibitors in daily clinical practice. Aliment Pharmacol Ther. 2006;24:377-85.
Zhou R, Wu C, Rau P-LP, et al. Young driving learners’ intention to use a handheld or hands-free mobile phone when driving. Transport Res F: Traffic Psychol Behav. 2009;12:208-217.
Aro P, Talley NJ, Ronkainen J, et al. Anxiety is associated with uninvestigated and functional dyspepsia (Rome III criteria) in a Swedish population-based study. Gastroenterology. 2009;137:94-100.
Tan VP, Cheung TK, Wong WM, et al. Treatment of functional dyspepsia with sertraline: a double-blind randomized placebo-controlled pilot study. World J Gastroenterol. 2012;18:6127-33.
Jackson JL, O’Malley PG, Tomkins G, et al. Treatment of functional gastrointestinal disorders with antidepressant medications: a meta-analysis. Am J Med. 2000;108:65-72.
Ford AC, Luthra P, Tack J, et al. Efficacy of psychotropic drugs in functional dyspepsia: systematic review and meta-analysis. Gut. 2017;66:411-420.
Fortney JC, Pyne JM, Edlund MJ, et al. Reasons for antidepressant nonadherence among veterans treated in primary care clinics. J Clin Psychiatry. 2011;72:827-34.
Zhong BL, Chen HH, Zhang JF, et al. Prevalence, correlates and recognition of depression among inpatients of general hospitals in Wuhan, China. Gen Hosp Psychiatry. 2010;32:268-75.
Sirey JA, Bruce ML, Alexopoulos GS, et al. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52:1615-20.
Sirey JA, Banerjee S, Marino P, et al. Adherence to Depression Treatment in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74:1129-1135.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Grant Numbers: 81970473, 81670484, 81470812, 81970472, 81500412, and 81270463).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol and informed consent form were approved by the Medical Ethics Committee of Renji Hospital (Approval No. KY2019032). An informed consent form was obtained from each participant.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bo Wang and Qing-Qing Luo contributed equally to this work.
Electronic Supplementary Material
ESM 1
(DOCX 14 kb).
Rights and permissions
About this article
Cite this article
Wang, B., Luo, QQ., Li, Q. et al. Daily Short Message Service Reminders Increase Treatment Compliance and Efficacy in Outpatients with Functional Dyspepsia: a Prospective Randomized Controlled Trial. J GEN INTERN MED 35, 2925–2931 (2020). https://doi.org/10.1007/s11606-020-06088-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-06088-3