Abstract
Background
While the Affordable Care Act’s (ACA) Medicaid expansion has increased insurance coverage, its effects on health outcomes have been mixed. This may be because previous research did not disaggregate mental and physical health or target populations most likely to benefit.
Objective
To examine the association between Medicaid expansion and changes in mental health, physical health, and access to care among low-income childless adults with and without chronic conditions.
Design
We used a difference-in-differences analytical framework to assess differential changes in self-reported health outcomes and access to care. We stratified our analyses by chronic condition status.
Participants
Childless adults, aged 18–64, with incomes below 138% of the federal poverty level in expansion (n = 69,620) and non-expansion states (n = 57,628).
Intervention
Active Medicaid expansion in state of residence.
Main Measures
Self-reported general health; total days in past month with poor health, poor mental health, poor physical health, or health-related activity restrictions; disability; depression; insurance coverage; cost-related barriers; annual check-up; and personal doctor.
Key Results
Medicaid expansion was associated with reductions in poor health days (−1.2 days [95% CI, −1.6,-0.7]) and days limited by poor health (−0.94 days [95% CI, −1.4,-0.43]), but only among adults with chronic conditions. Trends in general health measures appear to be driven by fewer poor mental health days (−1.1 days [95% CI, −1.6,-0.6]). Expansion was also associated with a reduction in depression diagnoses (−3.4 percentage points [95% CI, −6.1,-0.01]) among adults with chronic conditions. Expansion was associated with improvements in access to care for all adults.
Conclusions
Medicaid expansion was associated with substantial improvements in mental health and access to care among low-income adults with chronic conditions. These positive trends are likely to be reversed if Medicaid expansion is repealed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Twenty-six states plus the District of Columbia expanded their Medicaid programs through the Affordable Care Act in 2014, and three additional states (Pennsylvania, Indiana, and Alaska) adopted Medicaid expansion in 2015.1 Individuals with incomes below 138% of the federal poverty level (FPL) became eligible for public health insurance in states that expanded Medicaid, which substantially increased the number of adults with health insurance coverage.2 , 3 Medicaid expansion also improved other access-to-care measures and reduced cost-related barriers to care.4 , 5
While there is clear evidence that Medicaid expansion has increased coverage and access to care, findings with respect to changes in actual health outcomes have been more limited and mixed. A recent analysis of data from Texas, Kentucky, and Arkansas,6 as well as an analysis from a national survey,7 found a positive association between the ACA’s Medicaid expansion and self-reported general health. Conversely, analyses using other nationally representative data sets have not found a significant association between Medicaid expansion and self-reported health outcomes.4 , 5
Analyses of the impact of Medicaid expansion on health outcomes have three important limitations that may contribute to the mixed findings to date. First, although self-reported general health is a valid predictor of functional decline,8 health care utilization,9 and mortality,10 , 11 it is somewhat limited in that it does not capture differences between mental and physical health. This is a key distinction, because Medicaid may have a larger impact on mental health. Quasi-experimental12 and experimental13 analyses of Medicaid expansions prior to the ACA found significant reductions in psychological distress, depression, and mental health-related quality of life, and little or no association with physical health outcomes.
Second, most studies of the ACA’s Medicaid expansion include all non-elderly adults, parents, and childless adults with income below 138% FPL.4 , 5 Low-income parents in expansion and non-expansion states were eligible for Medicaid to varying degrees prior to implementation of the ACA, whereas childless adults had no coverage in the majority of states.14 Recent work has shown that the largest gains in health insurance coverage through the ACA were among childless adults because of their low levels of pre-ACA coverage.2 The inclusion of parents in analyses of the ACA can attenuate the effect size, because many parents were already receiving the “treatment” (i.e., Medicaid) prior to the ACA Medicaid expansion.
Finally, individuals with chronic conditions are most likely to benefit from insurance expansion because they require ongoing treatment and management and are more sensitive to high levels of cost-sharing.15 , 16 Stratifying analyses by chronic condition status can focus on meaningful health improvements among the population most likely to benefit. Moreover, chronic conditions are more prevalent among childless adults than other adults who gained coverage through the Affordable Care Act.17
To address these factors, we utilized a nationally representative data set containing validated measures of both self-reported mental and physical health to assess the relationship between Medicaid expansion and health outcomes among low-income childless adults with and without chronic conditions. We also considered trends in several access-to-care measures.
METHODS
Data Source and Study Population
We used data from the 2011–2015 Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative cross-sectional telephone survey of US adults aged 18 and older. The BRFSS is conducted by state health departments in partnership with the Centers for Disease Control and Prevention (CDC) and aims to provide state-level data on health-related risk behaviors and chronic health conditions. Our sample provided 3 years of data prior to implementation of Medicaid expansion and 2 years of follow-up data for most expansion states. The CDC advises against comparing data prior to 2011 with data from 2011 and later because of sampling changes in 2011.18 Cellular respondents were added to the survey in 2011 to improve the representativeness of the sample.19 Adults were randomly selected for interview from households with a landline, and adults with a cellular telephone were randomly selected from a commercially available national database of cellular telephone numbers. BRFSS response rates during our study period were comparable to, and generally higher than, those of other national telephone surveys (landline response rate: 48–53%; cellular response rate: 28–47%).18
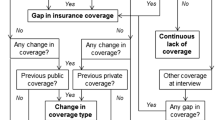
For our analyses, we used BRFSS core questions, which are consistent across states and years. To accommodate our analytical strategy, our study sample consisted of childless adults (herein referred to as adults) age 18–64 with household incomes below 138% FPL, targeting individuals who would qualify for Medicaid coverage if their state chose to expand Medicaid eligibility. Because income in BRFSS is only available in categories (i.e., less than $10,000, $10,000 to less than $15,000, etc.), we divided the midpoint of an individual’s income category by the FPL in the corresponding interview year to calculate income as a percentage of the FPL.7 We accounted for an individual’s household size in our calculation. Our analyses included all 29 states, plus the District of Columbia, that expanded Medicaid in 2014 or 2015 and the 21 states that had not expanded as of December 31, 2015.
We examined trends among adults with one or more chronic conditions and those with no chronic conditions. We identified chronic conditions based on methods used by the CDC to track chronic disease prevalence20 and that have been used to examine the impact of the ACA on health coverage among individuals with chronic conditions.16 An individual was determined to have a chronic condition if they reported ever being told by a health care provider that they had coronary heart disease (heart attack, angina, or coronary heart disease), stroke, asthma, chronic obstructive pulmonary disease, chronic kidney disease, cancer excluding skin cancer, arthritis, or diabetes (not including gestational diabetes or prediabetes). BRFSS respondents were asked about hypertension only in odd years. Therefore, we did not include hypertension in our list of chronic conditions.
Outcome Measures
Our primary health-related outcomes included self-reported general health, days in poor health in the past month, days limited by poor health in the past month, days in poor physical health in the past month, and days in poor mental health in the past month. These validated questions are associated with inpatient and outpatient health care utilization, as well as mortality.21 , 22 Self-reported general health was based on whether an individual reported poor, fair, good, very good, or excellent health, and was analyzed as a five-point scale from 1 (poor) to 5 (excellent). Poor health days (physical health, mental health, total poor health days, and days limited) were count variables ranging from 0 to 30. Poor mental health and physical health days were summed to a maximum of 30 to provide total poor health days.23
We also measured changes in disability. The CDC defines an individual as disabled if they responded “Yes” to either or both questions from the BRFSS two-question disability scale (“Are you limited in any way in any activities because of physical, mental, or emotional problems?” and “Do you now have any health problem that requires you to use special equipment, such as a cane, a wheelchair, a special bed, or a special telephone?”).24
We measured self-reported depression because Medicaid has previously been associated with changes in mental health.12 , 13 Depression was determined by response to the question “Has a doctor or other healthcare provider ever told you that you have a depressive disorder, including depression, major depression, dysthymia, or minor depression?”
Our access-related outcome measures included any current health insurance coverage, any time in the past 12 months when they did not see a doctor due to cost, any routine check-up in the last year, and having a “personal doctor or health care provider.”
Statistical Analysis
We tabulated baseline demographic characteristics of our study population, stratified by chronic condition status. Baseline demographic comparisons included individuals in expansion and non-expansion states prior to January 1, 2014, when most states implemented their Medicaid expansion programs. Significance testing was performed with Pearson’s chi-square test.
Next, we calculated unadjusted differences for each outcome before and after Medicaid expansion between expansion and non-expansion states. We used linear regression models to stratify our analyses by chronic condition status and allowed for different transition times by state as needed.25
In adjusted difference-in-differences analyses, we used multivariable linear regression models to estimate the effect of Medicaid expansion for each of our health-related outcomes among individuals with and without chronic conditions. In adjusted models, our key independent variable was the product of an interaction between indicators for expansion state and the post-expansion time period (equal to 1 for participants in states with Medicaid expansion during the month of their interview and 0 otherwise).5 , 26 The coefficient of this variable represented the differential change in outcomes (from before to after Medicaid expansion) between expansion and non-expansion states. Estimates were adjusted for age, race/ethnicity, sex, education, marital status, and state-year unemployment rate, as well as state-level and quarter-year fixed effects. The underlying time trend, as well as all time-invariant differences between states, are accounted for by fixed effects. We estimated robust standard errors clustered at the state level to account for serial autocorrelation.6 , 27 , 28 Additional information regarding model specification can be found in the online Appendix. We used the same multivariable linear regression models to determine whether Medicaid expansion was associated with measures of health care access among adults with and without chronic conditions.
Difference-in-differences analyses assume that adjusted trends in the control and experimental groups are similar before implementation of a given policy (e.g., Medicaid). Therefore, we examined differences in trends between expansion and non-expansion states in the years prior to implementation of the ACA (2011–2013).
Medicaid enrollees may be more likely to be diagnosed with a chronic condition, due to improved health care access,13 , 28 and such changes in the study population could influence our findings if newly diagnosed individuals tend to be healthier than previously diagnosed individuals. Therefore, we used our difference-in-differences framework to determine whether Medicaid expansion was associated with changes in diagnosis of a chronic condition.
Finally, we conducted sensitivity analyses using our primary multivariable linear regression models to examine all outcomes among elderly adults (65 and older) with and without chronic conditions. If conditions other than the ACA (which targeted individuals aged 18–64) were driving changes in health, we would expect to see similar changes among elderly adults. We additionally conducted difference-in-difference-in-differences analyses to determine whether trends among elderly individuals with chronic conditions were statistically significantly different from trends among non-elderly individuals. All analyses utilized survey weights to allow for national inferences and were conducted using Stata/SE 15.0 (StataCorp LLC, College Station, TX).
RESULTS
Sociodemographic Characteristics
Our sample consisted of 127,248 childless adults surveyed between 2011 and 2015, with incomes ≤138% of the FPL. There were 47,942 adults without a chronic condition and 79,306 adults with at least one chronic condition. Adults with chronic conditions who lived in expansion states were more likely to be younger than 35, Hispanic, and unmarried, have a high school education, and have higher state unemployment than adults with chronic conditions in non-expansion states (Table 1). Adults without chronic conditions who lived in expansion states were more likely to be younger than 25 and Hispanic, have a high school education, and have higher state unemployment than adults without a chronic condition in non-expansion states (Table 1).
Health Outcomes
Tables 2 and 3 present the results for health outcomes among adults without and with chronic conditions, respectively. In both tables, the unadjusted prevalence estimates generally suggest improvements in Medicaid expansion states and smaller improvements or declines in non-expansion states over our study period. The unadjusted differences in these trends were more often significant among those with chronic conditions. The magnitude of unadjusted difference-in-differences estimates was qualitatively larger among adults with chronic conditions.
After adjusting for confounders, we found that Medicaid expansion was not associated with significant changes in any of our measured health outcomes among adults without chronic conditions (Table 2).
In contrast, among adults with chronic conditions, we found that Medicaid expansion was associated with a significant improvement in self-reported health (0.07 [95% CI, 0.01 to 0.14]) and a significant reduction in total days in poor health (−1.2 days [95% CI, −1.6 to −0.66]) and days limited by poor health (−0.94 days [95% CI, −1.4 to −0.43]) (Table 3). These improvements appear to be attributable primarily to a reduction in poor mental health days (−1.1 [95% CI, −1.6 to −0.60]). There were no changes in poor physical health days or disability among adults with chronic conditions. Consistent with our finding of an association with fewer poor mental health days, we found that Medicaid expansion was associated with a significant decrease in self-reported depression among adults with chronic conditions (−3.4 percentage points [95% CI, −6.1 to −0.64]).
Health Care Access
We also evaluated several measures of health care access. In adjusted analyses, we found that Medicaid expansion was associated with improvement in all calculated measures of health care access among adults without a chronic condition (Table 4). Medicaid expansion among this group was associated with significant changes in coverage, cost-related barriers to care, check-ups in the last year, and reporting a personal doctor.
For adults with at least one chronic condition, Medicaid was also associated with significant improvement in coverage and cost-related barriers (Table 5). Changes in having a check-up within the last year or reporting a personal doctor among adults with chronic conditions were significant at P < 0.1.
Pre-ACA Time Trends and Sensitivity Analyses
Adjusted linear time trends prior to Medicaid expansion (2011 to 2013) for most outcomes were similar between expansion and non-expansion states. There were minor differences in some access-related pre-ACA time trends, but coefficients were small relative to the effect of Medicaid.
Using the difference-in-differences approach developed for our main outcomes, we found no statistically significant association between Medicaid expansion and diagnosis of a chronic condition; Medicaid expansion was associated with a non-significant decrease in chronic conditions (−0.89 percentage points [95% CI, −2.5 to 0.75]). Notably, chronic condition prevalence among non-elderly childless adults increased in both Medicaid expansion and non-expansion states.
In other sensitivity analyses, we found no substantively similar trends in health outcomes or access-to-care measures among older Americans with or without chronic conditions. In our difference-in-difference-in-differences analysis, trends in mental health outcomes among non-elderly adults with chronic conditions in expansion versus non-expansion states were significantly different from trends among elderly adults with chronic conditions in expansion versus non-expansion states. Additional details can be found in the Appendix, available online.
DISCUSSION
Among a national sample of low-income childless adults, we found that Medicaid expansion was associated with a significant reduction in poor mental health days and self-reported depression, but only among adults with at least one chronic condition. Medicaid expansion was not associated with changes in poor physical health days among adults with or without chronic conditions. To our knowledge, this is the first national study to report positive changes in mental health measures among adults with chronic conditions following implementation of the ACA’s Medicaid expansion provision. These timely results are important to consider in light of continued calls for ACA repeal by President Trump and Republican legislators.29 , 30
Our findings are consistent with studies of state Medicaid expansions prior to Medicaid expansion under the ACA. The Oregon Health Insurance Experiment, which randomized low-income individuals to a Medicaid “lottery,” found that individuals who received Medicaid were significantly less likely to screen positive for depression and were more likely to report higher mental health-related quality of life.13 Individuals who received Medicaid through Oregon’s Health Insurance Experiment had similar physical-health-related quality of life as individuals who did not receive Medicaid. Our results also provide a plausible mechanism for results from an analysis of Medicaid expansion in three states between 1997 and 2007, which indicated that Medicaid expansion was associated with a 7.6% reduction in mortality rates from “external causes” (e.g, suicide and substance use).26 This mortality reduction may be driven by the mental health improvements we found were associated with Medicaid expansion.
Why might mental health improve among adults in Medicaid expansion states? First, we found that Medicaid expansion was associated with a significant reduction in cost-related barriers to care. Financial security through insurance coverage may lead to reduced levels of economic stress and improved mental health.31 , 32 Such financial security could be especially beneficial for individuals who use the health care system on a regular basis (i.e., adults with chronic conditions), and may explain our finding that Medicaid expansion was associated with improved mental health outcomes only among adults with chronic conditions. We also found significant improvements in general access-to-care measures. Improvement in access to care may represent higher rates of mental health treatment. However, although the ACA has improved health insurance coverage for individuals with mental illness, it has had little to no impact on mental health care utilization.33 , 34
Several recent studies also used BRFSS to examine trends in health insurance and health outcomes associated with the ACA Medicaid expansion.7 , 16 , 35 One study, by Courtemanche et al., found no association between Medicaid expansion and the health outcomes we examined.35 However, we isolated the population most likely to benefit from the Medicaid expansion—childless adults with chronic conditions—while others analyzed broader low-income populations.
Our study has important limitations. First, we were limited to 2 years of post-ACA data, although we used the most current data available. Medicaid expansion may have a larger impact on health once an individual has had coverage for several years, but our short-term results are critical to informing current policy debates surrounding Medicaid expansion. Second, we cannot infer causality from observational data. Confounding is likely reduced, however, with our use of a difference-in-differences analytical strategy with state- and quarter-year-level fixed effects. Finally, our measure of depression was intended to measure self-reported lifetime prevalence of depression and was not based on diagnostic criteria. Nonetheless, we detected changes similar to studies that used depression measures based on diagnostic criteria.13
Conclusions
In this national study of low-income childless adults, we found that Medicaid expansion was associated with significant improvements in self-reported mental health outcomes among adults with chronic conditions. Medicaid among this population was also associated with improved insurance coverage, fewer cost-related barriers, and improved access to care. Analysis of the ACA’s impact to date provides a benchmark for policymakers to estimate the effect of repealing the law. If Medicaid expansion is, in fact, repealed by the current administration, future research should examine whether improvements in health are reversed among low-income populations who lose coverage.
References
Status of state action on the Medicaid expansion decision. The Henry J. Kaiser Family Foundation. http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0. Published October 14, 2016. Accessed December 29, 2016.
McMorrow S, Kenney GM, Long SK, Gates JA. The ACA Medicaid Expansion Led to Widespread Reductions in Uninsurance among Poor, Childless Adults. Washington, D.C.: Urban Institute; 2017. http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf436464. Accessed April 12, 2017.
Health Policy Brief: Uninsurance Rates and the Affordable Care Act. Health Aff (Millwood). May 2016. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=157. Accessed December 29, 2016.
Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947–56. https://doi.org/10.1056/NEJMsa1612890.
Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366–74. https://doi.org/10.1001/jama.2015.8421.
Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–9. https://doi.org/10.1001/jamainternmed.2016.4419.
Simon K, Soni A, Cawley J. The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions. J Policy Anal Manage. 2017;36(2):390–417. https://doi.org/10.1002/pam.21972.
Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50B(6):S344–53. https://doi.org/10.1093/geronb/50B.6.S344.
Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50(5):517-528. https://doi.org/10.1016/S0895-4356(97)00045-0.
DeSalvo KB, Muntner P. Discordance between physician and patient self-rated health and all-cause mortality. Ochsner J. 2011;11(3):232–40.
Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. https://doi.org/10.2307/2955359.
McMorrow S, Kenney GM, Long SK, Goin DE. Medicaid expansions from 1997 to 2009 increased coverage and improved access and mental health outcomes for low-income parents. Health Serv Res. 2016;51(4):1347–67. https://doi.org/10.1111/1475-6773.12432.
Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment — effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368:1713–22. https://doi.org/10.1056/NEJMsa1212321.
Medicaid eligibility for adults as of January 1, 2014. The Henry J. Kaiser Family Foundation. http://kff.org/medicaid/fact-sheet/medicaid-eligibility-for-adults-as-of-january-1-2014/. Published October 1, 2013. Accessed April 28, 2017.
Galbraith AA, Ross-Degnan D, Soumerai SB, Rosenthal MB, Gay C, Lieu TA. Nearly half of families in high-deductible health plans whose members have chronic conditions face substantial financial burden. Health Aff (Millwood). 2011;30(2):322–31. https://doi.org/10.1377/hlthaff.2010.0584.
Torres H, Poorman E, Tadepalli U, et al. Coverage and Access for Americans With Chronic Disease Under the Affordable Care Act: A Quasi-Experimental Study. Ann Intern Med. 2017;166(7):472. https://doi.org/10.7326/M16-1256.
Karaca-Mandic P, Jena AB, Ross JS. Health and Health Care Use Among Individuals at Risk to Lose Health Insurance With Repeal of the Affordable Care Act. JAMA Intern Med. 2017;177(4):590–3. https://doi.org/10.1001/jamainternmed.2016.9541.
Behavioral Risk Factor Surveillance System: 2015 Summary Data Quality Report. Atlanta, GA: Centers for Disease Control and Prevention; 2015.
Behavioral Risk Factor Surveillance System - Improving Survey Methodology. Public Health Surveillance and Informatics Program Office. Centers for Disease Control and Prevention; 2012. https://www.cdc.gov/brfss/factsheets/pdf/DBS_BRFSS_survey.pdf. Accessed August 9, 2017.
Ward BW, Black LI. State and Regional Prevalence of Diagnosed Multiple Chronic Conditions Among Adults Aged ≥18 Years — United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(29):735–8. 10.15585/mmwr.mm6529a3.
Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures – Population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1:37. https://doi.org/10.1186/1477-7525-1-37.
Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin Exp Res. 2002;14(6):499–508.
Health-Related Quality of Life (HRQOL) - Methods and Measures. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/hrqol/methods.htm#3. Published May 27, 2016. Accessed April 28, 2017.
Stevens AC, Courtney-Long EA, Okoro CA, Carroll DD. Comparison of 2 disability measures, Behavioral Risk Factor Surveillance System, 2013. Prev Chronic Dis. 2016;13:160080. https://doi.org/10.5888/pcd13.160080.
Meyer BD. Natural and Quasi-Experiments in Economics. J Bus Econ Stat. 1995;13(2):151–61. https://doi.org/10.1080/07350015.1995.10524589.
Sommers BD, Baicker K, Epstein AM. Mortality and Access to Care among Adults after State Medicaid Expansions. N Engl J Med. 2012;367(11):1025–34. https://doi.org/10.1056/NEJMsa1202099.
Bertrand M, Duflo E, Mullainathan S. How Much Should We Trust Differences-In-Differences Estimates? Q J Econ. 2004;119(1):249–75. https://doi.org/10.1162/003355304772839588.
Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions - a quasi-experimental study. Ann Intern Med. 2016. https://doi.org/10.7326/M15-2234.
Oberlander J. The end of Obamacare. N Engl J Med. November 2016. https://doi.org/10.1056/NEJMp1614438.
Jost T. House passes AHCA: how it happened, what it would do, and its uncertain Senate future. Health Aff (Millwood). May 2017. http://healthaffairs.org/blog/2017/05/04/house-passes-ahca-how-it-happened-what-it-would-do-and-its-uncertain-senate-future/. Accessed May 8, 2017.
Kronick R, Bindman AB. Protecting Finances and Improving Access to Care with Medicaid. N Engl J Med. 2013;368(18):1744–45. https://doi.org/10.1056/NEJMe1302107.
Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: a systematic review and meta-analysis. Clin Psychol Rev. 2013;33(8):1148–62. https://doi.org/10.1016/j.cpr.2013.08.009.
Creedon TB, Cook BL. Access to mental health care increased but not for substance use, while disparities remain. Health Aff (Millwood). 2016;35(6):1017–21. https://doi.org/10.1377/hlthaff.2016.0098.
Saloner B. An update on “insurance coverage and treatment use under the Affordable Care Act among adults with mental and substance use disorders.” Psychiatr Serv. 2017;68(3):310–1. https://doi.org/10.1176/appi.ps.201600566.
Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health. NBER Working Paper 23269, National Bureau of Economic Research; 2017. https://doi.org/10.3386/w23269.
Funding
This research was funded with support from the Robert Wood Johnson Clinical Scholars Program and the Ann Arbor VA Healthcare System.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Additional information
Prior Presentations
An earlier version of this manuscript was presented at the Society of General Internal Medicine Annual Conference in Washington, DC, on April 21, 2017.
Electronic supplementary material
ESM 1
(DOCX 100 kb)
Rights and permissions
About this article
Cite this article
Winkelman, T.N., Chang, V.W. Medicaid Expansion, Mental Health, and Access to Care among Childless Adults with and without Chronic Conditions. J GEN INTERN MED 33, 376–383 (2018). https://doi.org/10.1007/s11606-017-4217-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-017-4217-5