Abstract
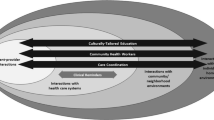
Over the past decade, researchers have shifted their focus from documenting health care disparities to identifying solutions to close the gap in care. Finding Answers: Disparities Research for Change, a national program of the Robert Wood Johnson Foundation, is charged with identifying promising interventions to reduce disparities. Based on our work conducting systematic reviews of the literature, evaluating promising practices, and providing technical assistance to health care organizations, we present a roadmap for reducing racial and ethnic disparities in care. The roadmap outlines a dynamic process in which individual interventions are just one part. It highlights that organizations and providers need to take responsibility for reducing disparities, establish a general infrastructure and culture to improve quality, and integrate targeted disparities interventions into quality improvement efforts. Additionally, we summarize the major lessons learned through the Finding Answers program. We share best practices for implementing disparities interventions and synthesize cross-cutting themes from 12 systematic reviews of the literature. Our research shows that promising interventions frequently are culturally tailored to meet patients’ needs, employ multidisciplinary teams of care providers, and target multiple leverage points along a patient’s pathway of care. Health education that uses interactive techniques to deliver skills training appears to be more effective than traditional didactic approaches. Furthermore, patient navigation and engaging family and community members in the health care process may improve outcomes for minority patients. We anticipate that the roadmap and best practices will be useful for organizations, policymakers, and researchers striving to provide high-quality equitable care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In 2005, the Robert Wood Johnson Foundation (RWJF) created Finding Answers: Disparities Research for Change (www.solvingdisparities.org) as part of its portfolio of initiatives to reduce racial and ethnic disparities in health care.1 RWJF charged Finding Answers with three major functions: administer grants to evaluate interventions to reduce racial and ethnic disparities in care, perform systematic reviews of the literature to determine what works for reducing disparities, and disseminate these findings nationally. Over the past seven years, Finding Answers has funded 33 research projects and performed 12 systematic literature reviews, including the five papers in this symposium.2–6 We are now beginning to leverage this research base to provide technical assistance to organizations that are implementing disparities reduction interventions, such as those participating in RWJF’s Aligning Forces for Quality program.7
This paper summarizes the major lessons learned from the systematic reviews and provides a disparities reduction framework. Building on our prior work,8–10 we present a roadmap for organizations seeking to reduce racial and ethnic disparities in health care. This roadmap may be tailored for use across diverse health care settings, such as private practices, managed care organizations, academic medical centers, public health departments, and federally qualified health centers. Specifically, we outline the following steps:
-
1)
Recognize disparities and commit to reducing them
-
2)
Implement a basic quality improvement structure and process
-
3)
Make equity an integral component of quality improvement efforts
-
4)
Design the intervention(s)
-
5)
Implement, evaluate, and adjust the intervention(s)
-
6)
Sustain the intervention(s)
FINDINGS FROM THE SYSTEMATIC REVIEWS
The five systematic reviews in the present symposium examined interventions to improve minority health and potentially reduce disparities in asthma, HIV, colorectal cancer, prostate cancer, and cervical cancer.2–6 While many valuable ideas to address racial and ethnic health disparities are being pursued outside of the healthcare system, Finding Answers focuses specifically on what can be accomplished once regular access to healthcare services is achieved. Thus, the reviews focused on interventions that occur in or have a sustained linkage to a healthcare delivery setting; programs that were strictly community-based were outside the scope of the project. Additionally, the reviews examined racial and ethnic disparities in care and improvements in minority health, rather than geographic, socioeconomic, or other disparities. For a description of search strategies employed in these reviews, see the technical web appendix which can be accessed online (Electronic Supplementary Material).
Each review identified promising practices to improve minority health within the healthcare setting. The asthma paper found that educational interventions were most common, with culturally tailored, skills-based education showing promise.5 Outpatient support, as well as education for inpatient and emergency department patients, were effective. Similarly, the HIV review noted that interactive, skills-based instruction was more likely to be effective than didactic educational approaches for changing sexual health behavior.3 The paper identified a dearth of interventions that target minority men who have sex with men. The colorectal cancer review found that patient education and navigation were the most common interventions and that those with intense patient contact (e.g., in person or by telephone) were the most likely to increase screening rates.4 The colorectal cancer review identified no articles that described interventions to reduce disparities in post-screening follow-up, treatment, survivorship, or end-of-life care. Based on low to moderate evidence, the cervical cancer review reported that navigation combined with either education delivered by lay health educators or telephone support can increase the rate of screening for cervical cancer among minority populations.2 Telephone counseling might also increase the diagnosis and treatment of premalignant lesions of the cervix for minority women. The prostate cancer review focused on the importance of informed decision making for addressing prostate cancer among racial and ethnic minority men.6 Educational programs were the most effective intervention for improving knowledge among screening-eligible minority men. Cognitive behavioral strategies improved quality of life for minority men treated for localized prostate cancer. However, more research is needed about interventions to improve informed decision making and quality of life among minority men with prostate cancer.
CROSS-CUTTING THEMES
We looked across these reviews and Finding Answers’ previous research,11–17 and identified several cross-cutting themes. Our findings showed that promising interventions frequently were multi-factorial, targeting multiple leverage points along a patient’s pathway of care. Culturally-tailored interventions and those that employed a multi-disciplinary team of care providers also tended to be effective. Additionally, we found that education using interactive methods to deliver skills training were more effective than traditional, didactic approaches in which the patient was a passive learner. Patient navigation and interventions that actively involved family and community members in patient care showed promise for improving minority health outcomes. Finally, the majority of interventions targeted changing the knowledge and behavior of patients, generally with some form of education. Interventions directed at providers, microsystems, organizations, communities, and policies were far less common, thus representing an opportunity for future research.
ROADMAP FOR REDUCING DISPARITIES
Table 1 summarizes the major steps health care organizations need to undertake to reduce disparities. Past efforts have focused on Step 1 (e.g. collecting performance data stratified by race, ethnicity, and language) or Step 4 (designing a specific intervention). Our roadmap highlights that these are crucial steps, but will have limited impact unless the other steps are addressed. Effective implementation and long-term sustainability require attention to all six steps.
-
1)
Recognize disparities and commit to reducing them
When health care organizations and providers realize there are disparities in their own practices,18 they become motivated to reduce them.19 Therefore, the Patient Protection and Affordable Care Act of 2010 makes the collection of performance data stratified by race, ethnicity, and language (REL) a priority.20 Similarly RWJF’s Aligning Forces for Quality Program initially focused its disparities efforts on the collection of REL data in different communities. The Institute of Medicine (IOM) recently recommended methods to collect REL data,21 and groups such as the Health Research and Educational Trust (HRET) have developed toolkits to guide organizations in this effort.22
Besides race-stratified performance data, training in health disparity issues (e.g., through cultural competency training) may help providers identify and act on disparities in their own practices. However, while cultural competency training and stratified performance data may increase the readiness of providers and organizations to change their behavior,19 these interventions will need to be accompanied by more intensive approaches to ameliorate disparities. Sequist et al. found that cultural competency training and performance reports of the quality of diabetes care stratified by race and ethnicity increased providers’ awareness of disparities, but did not improve clinical outcomes.23 Therefore, our roadmap for reducing disparities highlights the importance of combining REL data collection with interventions targeted towards specific populations and settings.
-
2)
Implement a basic quality improvement structure and process
Interventions to reduce disparities will not get very far unless there is a basic quality improvement structure and process upon which to build interventions.24,25 Basic elements include a culture where quality is valued, creation of a quality improvement team comprised of all levels of staff, a process for quality improvement, goal setting and metrics, a local team champion, and support from top administrative and clinical leaders. If robust quality improvement structures and processes do not exist, then they must be created and nurtured while disparities interventions are developed.
-
3)
Make equity an integral component of quality improvement efforts
For too long, disparities reduction and quality improvement have been two different worlds. People generally thought about reducing disparities separately from efforts to improve quality, and oftentimes different people in an organization were responsible for implementing disparity and quality initiatives. A major development over the past decade is the increasing recognition that equity is a fundamental component of quality of care. Efforts to reduce disparities need to be mainstreamed into routine quality improvement efforts rather than being marginalized.26 That is, we need to think about the needs of the vulnerable patients we serve as we design interventions to improve care in our organizations, and address those needs as part of every quality improvement initiative. The Institute of Medicine’s Crossing the Quality Chasm report stated that equity was one of six components of quality,27 and the IOM’s 2010 report Future Directions for the National Healthcare Quality and Disparities Reports highlighted equity further by elevating it to a cross-cutting dimension that intersects with all components of quality care.28 Major health care organizations have instituted initiatives that promote the integration of equity into quality efforts including the American Board of Internal Medicine (Disparities module as part of the recertification process), American College of Cardiology (Coalition to Reduce Racial and Ethnic Disparities in Cardiovascular Disease Outcomes [CREDO] initiative),29 American Medical Association (Commission to End Health Care Disparities), American Hospital Association (Race, ethnicity, and language data collection),22 Joint Commission (Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: a Roadmap for Hospitals),30 and National Quality Forum (Healthcare Disparities and Cultural Competency Consensus Standards Development). For many health care organizations and providers, this integration of equity and quality represents a fundamental change from generic quality improvement efforts that improve only the general system of care, to interventions that improve the system of care and are targeted to specific priority populations and settings.
-
4)
Design the intervention(s)
While several themes have emerged regarding successful interventions to reduce health care disparities based on our systematic reviews and grantees, solutions must be individualized to specific contexts, patient populations, and organizational settings.31 For example, solutions for reducing diabetes disparities for African-Americans in Chicago may differ from the answers for African-Americans in the Mississippi Delta. We recommend determining the root causes of disparities in the health care organization or provider’s patient population and designing interventions based on a conceptual model that targets six levels of influence: patient, provider, microsystem, organization, community, and policy (Table 2).8,9 Each level represents a different leverage point that can be addressed to reduce disparities. The relative importance of these levels may vary across diverse organizations and patient populations.
Specific intervention strategies can then be developed to target different levels of influence. Table 3 offers an overview of strategies identified through the review of approximately 400 disparities intervention studies, including the 33 Finding Answers projects and 12 systematic literature reviews. Common intervention strategies include delivering education and training, restructuring the care team, and increasing patient access to testing and screening. About half of the interventions targeted only one of the levels of influence described above; most efforts were directed at patients in the form of education or training. Research evaluating pay-for-performance, on the other hand, was scant and requires further attention, especially given current interest in incentive-based programs. Going forward, Finding Answers aims to categorize each of the approximately 400 studies by level of influence and strategy, and to identify which combinations are promising for disparities reduction.
Organizations can find practical resources and promising intervention strategies on the Finding Answers website (www.solvingdisparities.org) or the Agency for Healthcare Research and Quality (AHRQ) Health Care Innovations Exchange (www.innovations.ahrq.gov). Systematic reviews such as those by Finding Answers and forthcoming ones from the AHRQ Evidence-Based Practice Center Program and the Veterans Administration can inform what types of interventions are most appropriate in different situations. In addition, organizations can learn about successful projects from peers through learning collaboratives,24 site visits, case studies, and webinars.
While there is no silver bullet to reduce disparities, successful interventions reveal important themes. As previously noted, we looked across 12 systematic reviews of the literature and identified promising practices that can inform the design of future disparities interventions.2–6,11–17 These include culturally tailoring programs to meet patients’ needs, patient navigation, and engaging multidisciplinary teams of care providers in intervention delivery. Effective interventions frequently target multiple leverage points along a patient’s pathway of care and actively involve families and community members in the care process. Additionally, successful health education programs often incorporate interactive, skills-based training for minority patients.
-
5)
Implement, evaluate, and adjust the intervention(s)
The National Institutes of Health recently held its fifth annual conference on the science of dissemination and implementation to promote further research in this field, create opportunities for peer-to-peer learning, and showcase available models and tools. One such model is the Consolidated Framework for Implementation Research (CFIR), for which Damschroder et al. reviewed conceptual models of relevant factors in implementing a quality improvement intervention and synthesized existing frameworks into a single overarching model.32 The CFIR covers five domains: intervention characteristics (e.g. relative advantage, adaptability, complexity, cost), outer setting (e.g. patient needs and resources, external policy and incentives), inner setting (e.g. culture, implementation climate, readiness for implementation), characteristics of the individuals involved (e.g. knowledge and beliefs about the intervention, self-efficacy, stage of change), and the process of implementation (e.g. planning, engaging, executing, evaluating). Too often organizations focus on the content of an intervention without planning its implementation in sufficient detail. A model such as CFIR supplies a checklist of factors to consider in implementing an intervention to reduce disparities.
Through work with our 33 grantees, we have developed a series of best practices for implementing interventions to reduce disparities. These lessons were pulled from detailed qualitative data gathered through the Finding Answers program, and represent perspectives from organization leadership, providers, administrators, and front-line staff. We found common implementation challenges and solutions across health care settings. Table 4 summarizes best practices for disparities reduction efforts, provides the rationale and expected outcomes, and offers recommended strategies for delivering a high-quality equity initiative.
Implementation is an iterative process and organizations are unlikely to get the perfect solution on their first attempt. Thus, evaluation of the intervention and adjustments to the program based on performance data stratified by race, ethnicity, and language are integral parts of the implementation process. Setting realistic goals is essential to accurately assess program effectiveness. Processes of care (e.g. measurement of hemoglobin A1c in patients with diabetes) generally improve more rapidly than patient outcomes (e.g. actual hemoglobin A1c value), and may therefore be better markers of short-term disparities reduction success, while outcomes could be longer-term targets.
-
6)
Sustain the intervention(s)
Health care organizations, administrative leaders, and providers need to proactively plan for the sustainability of the intervention. Sustainability is dependent upon institutionalizing the intervention and creating feasible financial models. Too often interventions are dependent upon the initial champion and first burst of enthusiasm. If that champion leaves the organization or if staff tire after the early stages of implementation, then the disparities initiative is at risk for discontinuation. Institutionalization requires promoting an organizational culture that values equity, creating incentives to continue the effort, whether financial and/or non-financial, and weaving the intervention into the fabric of everyday operations so that it is part of routine care as opposed to a new add-on (e.g. Step 3 in Table 1).
In the long-term, however, interventions must be financially viable. The business case for reducing disparities is evolving and must be viewed from both societal and individual organization/provider perspectives.33–35 From a societal perspective, the business case for reducing disparities centers on direct medical costs, indirect costs, and the creation of a healthy national workforce in an increasingly competitive global economy. Laveist et al. estimate that disparities for minorities cost the United States $229 billion in direct medical expenditures and $1 trillion in indirect costs between 2003 and 2006.36 America’s demographics are becoming progressively more diverse. The United States Census Bureau estimates that by 2050, the Hispanic population will reach 30 %, the black population 13 %, and the Asian population 8 %.37 Thus, from global and national economic perspectives, disparities reduction will become increasingly important if we are to have a healthy workforce that can successfully compete in the international marketplace and support the rapidly growing non-working aging population on the Social Security and Medicare entitlement programs.
From the perspective of the individual health care organization or provider, the immediate incentives are more complex. Integrated care delivery systems have an incentive to reduce disparities to decrease costly emergency department visits and hospitalizations. Large insurers are incentivized to provide high quality care for everyone to be more competitive in marketing their products to employers with increasingly diverse workforces. However, outpatient clinics and providers in the current, predominantly fee-for-service world, especially those serving the uninsured and underinsured, frequently do not have clear incentives to reduce disparities since the money saved from the prevented emergency department visit or hospitalization does not accrue to them.34
Currently, it is difficult to accurately predict the results of health care reform and efforts to contain the Medicare and Medicaid budgets, but several trends indicate that organizations would be wise to integrate disparities reduction into their ongoing quality improvement initiatives. Major national groups such as the Department of Health and Human Services (HHS), Agency for Healthcare Research and Quality, Centers for Disease Control (CDC), Centers for Medicare and Medicaid Services, and Institute of Medicine have consistently stressed the importance of reducing health care disparities and using quality improvement as a major tool to accomplish this goal.28,38–42 The Affordable Care Act emphasizes collection of race, ethnicity, and language data.20 Private demonstration projects, such as the Robert Wood Johnson Foundation Aligning Forces for Quality Program,7 aim for multistakeholder coalitions of providers, payers, health care organizations, and consumers to improve quality and reduce disparities on regional levels. Intense policy attention has been devoted to accountable care organizations,43 the patient-centered medical home,44 and bundled payments.45 These organizational structures and financing mechanisms emphasize coordinated, population based care that may reduce disparities.
Reducing racial and ethnic disparities in care is the right thing to do for patients, and, from a business perspective, health care organizations put themselves at risk if they do not prepare for policy and reimbursement changes that encourage reduction of disparities. We believe that health care organizations and providers would be imprudent if they did not plan for payment and coverage possibilities such as:
-
1)
Incentives and reimbursements for team-based care. Team-based care is one of the most consistently successful types of disparities interventions,9 but current payment mechanisms often do not create viable business models for sustainability. We believe that it is likely that future policies encouraging efficiency will increasingly reimburse or incentivize team-based care management activities; reimburse or incentivize use of non-physician members of the team, such as community health workers, peer educators and patient navigators; and ensure that downstream savings from care teams, such as averted hospitalizations and emergency department visits, flow back to those that generated the savings.
-
2)
Implementation of pay-for-performance programs for reducing racial and ethnic disparities. Pay-for-performance is likely to become part of efforts to move from paying for volume to paying for quality. It will be important to incorporate safeguards such as pay-for-improvement to avoid cherry picking of easy patients, patient dropping, and harming of poorly resourced organizations caring for predominantly vulnerable populations.16
-
3)
Incentives to create linkages between community and health care system. The new CDC Health Disparities and Inequalities Report and HHS National Strategy for Quality Improvement in Health Care exemplify the rise of combined public health—health care approaches to reduce disparities.39,41,46 Integration of community health workers and other peer-based programming into the health care team shows potential,4,12 and there is evidence that directly involving families, schools, and community-based organizations in health care interventions can improve health outcomes.17
CONCLUSION
As outlined in our roadmap, it is critical to create an organizational culture and infrastructure for improving quality and equity. Organizations must design, implement, and sustain interventions based on the specific causes of disparities and their unique institutional environments and patient needs. To be most effective, all of these elements eventually need to be addressed; 24 however, we do not want to encourage paralysis for those who might perceive a daunting set of obstacles to overcome. Instead, our experience has been that it useful for an organization to start working on disparities by targeting whatever step or action feels right to them and is thus a priority.46 Eventually the other steps will need to be addressed, but reducing disparities is often a dynamic process that evolves over time. While more disparities intervention research is needed, we have learned much over the past 10 years about which approaches are likely to succeed. The time for action is now.
REFERENCES
Schlotthauer AE, Badler A, Cook SC, Perez DJ, Chin MH. Evaluating interventions to reduce health care disparities: an RWJF program. Health Aff. 2008;27:568–73.
Glick SB, Clarke AR, Blanchard A, Whitaker AK. Cervical cancer screening, diagnosis, and treatment interventions for racial and ethnic minorities: a systematic review. J Gen Intern Med. doi:10.1007/s11606-012-2052-2.
Hemmige V, McFadden R, Cook S, Tang H, Schneider J. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. doi:10.1007/s11606-012-2036-2.
Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med. doi:10.1007/s11606-012-2044-2.
Press VG, Pappalardo AA, Conwell WD, Pincavage AT, Prochaska MH, Arora VM. Interventions to improve outcomes for minority adults with asthma: a systematic review. J Gen Intern Med. doi:10.1007/s11606-012-2058-9.
Saleha S, Kotwal AA, Dale W. Interventions to improve decision making and reduce racial and ethnic disparities in the management of prostate cancer: a systematic review. J Gen Intern Med. doi:10.1007/s11606-012-2086-5.
Painter MW, Lavizzo-Mourey R. Aligning Forces for Quality: a program to improve health and health care in communities across the United States. Health Aff (Millwood). 2008;27:1461–3.
Chin MH, Goldmann D. Meaningful disparities reduction through research and translation programs. JAMA. 2011;305:404–5.
Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64:7S–28S.
Chin MH. Improving care and outcomes of the uninsured with chronic disease…Now. Ann Intern Med. 2008;149:206–8.
Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64:29S–100S.
Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64:101S–56S.
Van Voorhees BW, Walters AE, Prochaska M, Quinn MT. Reducing health disparities in depressive disorders outcomes between non-Hispanic whites and ethnic minorities: a call for pragmatic strategies over the life course. Med Care Res Rev. 2007;64:157S–94S.
Masi CM, Blackman DJ, Peek ME. Interventions to enhance breast cancer screening, diagnosis, and treatment among racial and ethnic minority women. Med Care Res Rev. 2007;64:195S–242S.
Fisher T, Burnet DL, Huang ES, Chin MH, Cagney KA. Cultural leverage: interventions using culture to reduce racial disparities in health care. Med Care Res Rev. 2007;64:243S–82S.
Chien AT, Chin MH, Davis A, Casalino L. Pay-for-performance, public reporting and racial disparities in health care: how are programs being designed? Med Care Res Rev. 2007;64:283S–304S.
Chin MH, Alexander-Young M, Burnet D. Health care quality improvement approaches to reducing child health disparities. Pediatrics. 2009;124(Suppl 3):S224–36.
Agency for Healthcare Research and Quality. 2010 National Healthcare Disparities Report. AHRQ Publication No. 11–0005. Rockville, M.D.: Agency for Healthcare Research and Quality, 2011. Available at: http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf. Accessed May 23, 2011.
Robert Wood Johnson Foundation. Expecting Success: Excellence in Cardiac Care Results from Robert Wood Johnson Foundation Quality Improvement Collaborative. Published November 19, 2008. Available at: http://www.rwjf.org/files/research/expectingsuccessfinalreport.pdf. Accessed June 27, 2011.
Patient Protection and Affordable Care Act and Health Care and Education Reconciliation Act of 2010.
Institute of Medicine. Race, ethnicity, and language data: standardization for health care quality improvement. Washington, D.C.: The National Academies Press; 2009.
Hasnain-Wynia R, Pierce D, Haque A, Hedges Greising C, Prince V, Reiter J. Health Research and Educational Trust Disparities Toolkit. Available at: http://www.hretdisparities.org. Accessed January 21, 2011.
Sequist TD, Fitzmaurice GM, Marshall R, Shaykevich S, Marston A, Safran DG, Ayanian JZ. Cultural competency training and performance reports to improve diabetes care for black patients: a cluster randomized, controlled trial. Ann Intern Med. 2010;152(1):40–6.
Chin MH. Quality improvement implementation and disparities: the case of the Health Disparities Collaboratives. Med Care. 2010;48:688–75.
Integrating Chronic Care and Business Strategies in the Safety Net. (Prepared by Group Health’s MacColl Institute for Healthcare Innovation, in partnership with RAND and the California Health Care Safety Net Institute, under Contract No./Assignment No: HHSA2902006000171). AHRQ Publication No. 08-0104-EF. Rockville, MD: Agency for Healthcare Research and Quality. September 2008.
Chin MH, Chien AT. Reducing racial and ethnic disparities in health care: an integral part of quality improvement scholarship. Qual Saf Health Care. 2006;15:79–80.
Committee on Quality Health Care in America. Crossing the Quality Chasm: A New Healthcare System for the 21st Century. Washington, D.C.: National Academies Press; 2001.
Ulmer C, Bruno M, Burke S, eds. Future Directions for the National Healthcare Quality and Disparities Reports. Washington, D.C.: National Academies Press; 2010.
Yancy CW, Wang TY, Ventura HO, Piña IL, Vijayaraghavan K, Ferdinand KC, Hall LL. CREDO Advisory Group. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): why credo matters to cardiologists. J Am Coll Cardiol. 2011;57:245–52.
The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: a Roadmap for Hospitals. Oak Brook Terrace, IL: The Joint Commission; 2010.
Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney S, for the SQUIRE Development Group. Publication guidelines for improvement studies in health care: evolution of the SQUIRE Project. Qual Saf Health Care. 2008;17(Suppl 1):i3–9.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
Huang ES, Zhang Q, Brown SES, Drum M, Meltzer DO, Chin MH. The cost-effectiveness of improving diabetes care in U.S. federally-qualified community health centers. Health Serv Res. 2007;42(6 Pt 1):2174–93.
Huang ES, Brown SES, Zhang JX, Kirchhoff AC, Schaefer CT, Casalino LP, Chin MH. The cost consequences of improving diabetes care: the community health center experience. Jt Comm J Qual Safety. 2008;34:138–146.
Beal A. High-quality health care: the essential route to eliminating disparities and achieving health equity. Health Aff. 2011;30:1868–71.
Laveist TA, Gaskin DJ, Richard P. The economic burden of health inequalities in the United States. Joint Center for Political and Economic Studies. 2009. Available at: http://www.thomaslaveist.com/wp-content/downloads/Burden_Of_Health_Disparities_Final__Report.pdf. Accessed May 23, 2011.
United States Census Bureau, Population Division. Table 6. Percent of the Projected Population by Race and Hispanic Origin for the United States: 2010 to 2050 (NP2008-T6). Release Date: August 14, 2008. Available at: http://www.census.gov/population/www/projections/summarytables.html. Accessed May 25, 2011.
Department of Health and Human Services. A Nation Free of Disparities in Health and Health Care: HHS Action Plan to Reduce Racial and Ethnic Health Disparities. 2011. Available at: http://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf. Accessed May 23, 2011.
Department of Health and Human Services. Report to Congress: National Strategy for Quality Improvement in Health Care. 2011. Available at: http://www.healthcare.gov/center/reports/quality03212011a.html. Accessed June 17, 2011.
Agency for Healthcare Research and Quality. 2010 National Healthcare Quality Report. AHRQ Publication No. 11–0004. Rockville, M.D.: Agency for Healthcare Research and Quality. 2011. Available at: http://www.ahrq.gov/qual/nhqr10/nhqr10.pdf. Accessed May 23, 2011.
Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report – United States, 2011. Morbidity and Mortality Weekly Report 2011; 60 Suppl:1–113.
Centers for Medicare and Medicaid Services. Discover the health disparities program. Available at: http://www.cmspulse.org/cms.html. Accessed June 17, 2011.
Fisher ES, McClellan MB, Safran DG. Building the path to accountable care. N Engl J Med. 2011;365:2445–7.
Birnberg JM, Drum ML, Huang ES, Casalino LP, Lewis S, Vable AM, Tang H, Quinn MT, Burnet DL, Summerfelt T, Chin MH. Development of a Safety Net Medical Home Scale in Health Centers. J Gen Intern Med. 2011;26:1418–25.
Hackbarth G, Reischauer R, Mutti A. Collective accountability for medical care–toward bundled Medicare payments. N Engl J Med. 2008;359:3–5.
Peek ME, Wilkes AE, Roberson T, Goddu A, Nocon R, Tang H, Quinn M, Bordenave K, Huang ES, Chin MH. Early lessons from an initiative on Chicago's South Side to reduce disparities in diabetes care and outcomes. Health Aff. 2012;31:177–86.
Acknowledgements
Contributors
We would like to thank Melissa R. Partin, PhD, who served as the JGIM Deputy Editor for the six manuscripts in this Special Symposium: Interventions to Reduce Racial and Ethnic Disparities in Health Care. Dr. Partin provided valuable advice and feedback throughout this project. Marshall H. Chin, MD, MPH, and Amanda R. Clarke, MPH, served as the Robert Wood Johnson Foundation Finding Answers: Disparities Research for Change Systematic Review Leadership Team that oversaw the teams writing the articles in this symposium.
Funding Source
Support for this publication was provided by the Robert Wood Johnson Foundation Finding Answers: Disparities Research for Change Program. The Robert Wood Johnson Foundation had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, approval, or decision to submit the manuscript for publication.
Prior Presentations
Presented in part at the Society of General Internal Medicine Midwest Regional Meeting, September 23, 2010, Chicago, Illinois; the Society of General Internal Medicine Annual Meeting, May 5, 2011, Phoenix, Arizona; the American Public Health Association Annual Meeting, November 1, 2011, Washington, D.C.; and the Institute for Healthcare Improvement Annual National Forum, December 4, 2011, Orlando, Florida.
Conflict of Interest
The authors report no conflicts of interest with this work. Dr. Chin was also supported by a National Institute of Diabetes and Digestive and Kidney Diseases Midcareer Investigator Award in Patient-Oriented Research (K24 DK071933), Diabetes Research and Training Center (P60 DK20595), and Chicago Center for Diabetes Translation Research (P30 DK092949).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary materials
Below is the link to the electronic supplementary material.
ESM 1
(DOC 46 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chin, M.H., Clarke, A.R., Nocon, R.S. et al. A Roadmap and Best Practices for Organizations to Reduce Racial and Ethnic Disparities in Health Care. J GEN INTERN MED 27, 992–1000 (2012). https://doi.org/10.1007/s11606-012-2082-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2082-9