ABSTRACT
OBJECTIVES
To investigate the association between proximal colonic neoplasia and distal lesions as a function of the lesion type. The extent to which health, demographic, and study characteristics moderate this association was also examined.
DATA SOURCES
Google Scholar, Web of Science, Scopus, and PubMed.
STUDY ELIGIBILITY CRITERIA
Studies allowing the calculation of OR of proximal neoplasia
(PN) and proximal advanced neoplasia (PAN) for distal hyperplastic polyps (HP), nonadvanced adenomas (NAA), adenomas (AD), and advanced neoplasia (AN); also, studies for which the proportions of subjects with isolated (i.e., not accompanied by distal lesions) PN (IPN) and PAN (IPAN) over the total number of subjects with PN or PAN could be calculated.
STUDY APPRAISAL AND SYNTHESIS METHODS
Thirty-two studies were included for calculating OR between proximal neoplasia and distal lesions and 40 studies for proportions of IPN and IPAN. Subgroup analyses were conducted for presence of symptoms, prevalence of PN and PAN, age, proportion of males, geographic region, study design, and demarcation point.
RESULTS
The association between distal lesions and proximal neoplasia increased with the severity of the distal lesions. Odds of PN were higher in subjects with HP compared to subjects with a normal distal colon. Odds of PN and PAN were higher in subjects with NAA, AD, and AN than in subjects with a normal distal colon. PAN were more strongly associated with distal lesions in asymptomatic populations, in young populations, and in populations with a low prevalence of PAN. In approximately 60% of the subjects with PN and PAN, these neoplasia were isolated.
LIMITATIONS
The present results may be affected by publication bias and dichotomization in the subgroup analyses. Limitations related to the individual studies include self-selection, lesion misclassification and misses, and technological advances leading to changes in the detection of lesions during the time span of the included studies.
CONCLUSIONS AND IMPLICATIONS OF KEY FINDINGS
All types of distal lesions are predictive of PN. All types of distal neoplasia are predictive of PAN. The association between distal lesions and proximal neoplasia increases with the severity of the distal lesion. The association between distal lesions and proximal advanced neoplasia is stronger in low-risk groups as compared to high-risk groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The use of flexible sigmoidoscopy followed by colonoscopy in colorectal cancer screening programs relies on the assumption that distal lesions are reliable markers of proximal neoplasia. It is widely established that subjects with distal advanced neoplasia (AN) have increased odds of proximal neoplasia (PN) and proximal advanced neoplasia (PAN).1–3
Whether distal hyperplastic polyps (HP) are also markers of PN and PAN is debatable. Formal guidelines generally do not consider HP to be markers of PN or PAN.3–5 Seven of nine colonoscopy studies published to date revealed no significant associations between HP and PN,6–14 and only one of eight colonoscopy studies reported a significant association between HP and PAN.6,10,15–20 Pathology studies, however, suggest that HP could develop into cancer through microsatellite instability and hypermethylation pathways.21–25 The published pathological evidence has been suggested as one of the reasons why physicians tend not to adhere to formal guidelines and refer patients with HP alone for colonoscopy.26 The association between distal nonadvanced adenomas (NAA) and PN and PAN is equivocal as well, and screening recommendations leave the follow-up program for subjects with NAA to the judgment of the clinician.3,27,28
The effectiveness of flexible sigmoidoscopy for screening not only depends on whether distal lesions are markers of PN or PAN, but also on the PN and PAN that are isolated, that is, not accompanied by distal lesions (IPN and IPAN, respectively). It has been suggested that in about half of the subjects, PN do not have distal markers and are thus not identifiable by the sigmoidoscopy outcome alone.16,18,29 It has further been shown that the prevalence of IPN is higher in subjects older than 60 years, those with a family history of colorectal cancer, and those with 10 pack-years of smoking.30
Three previous meta-analyses31–33 have summarized the empirical evidence regarding the association between distal lesions and proximal neoplasia. Subjects with HP had higher odds of PN compared to subjects having a normal distal colon,33 and subjects with NAA were more likely to also have PN than subjects without distal neoplasia.32 Neither HP31,33 nor NAA32 appeared to increase the odds of PAN. These past meta-analyses need to be updated, however. A large number of relevant studies have been published since, offering the opportunity for a more powerful synthesis. Furthermore, the previous meta-analyses did not summarize the effects of demographic factors, such as age, gender, or geographic region, which show differential effects on the prevalence of colonic lesions.34,35 It is possible that the association between distal lesions and proximal neoplasia is also sensitive to these factors. Lastly, the existing meta-analyses did not investigate the extent to which demographic factors moderate the proportions of subjects with IPN and IPAN.
The aim of this meta-analysis was to investigate the relationship between distal lesions and proximal neoplasia as a function of lesion type, to estimate the proportion of subjects with isolated proximal neoplasia in the population, and to examine the extent to which health, demographic, and study characteristics are moderators of the association between distal lesions and proximal neoplasia and of the proportions of subjects with isolated proximal neoplasia.
METHOD
A literature search was carried out between 11 and 26 November 2010 using Google Scholar, Web of Science, Scopus, and PubMed. Each of the terms “proximal neoplasia”, “advanced proximal neoplasia”, “proximal advanced neoplasia”, “proximal neoplasms”, and “proximal adenoma” was combined with each of the terms “distal”, “hyperplastic”, “adenoma”, “nonadvanced”, “advanced”, “sigmoidoscopy”, and “colonoscopy” in a full-text search.
Exclusion Criteria
The following types of studies were excluded:
-
Studies in which subjects with a positive sigmoidoscopy outcome were referred to colonoscopy. These studies either lacked subjects with a normal distal colon to be used as a reference, or used as a reference subjects whose distal biopsies were found to consist of normal mucosa during histological examination conducted after colonoscopy.
-
Studies focusing on patient groups with colorectal cancer, inflammatory bowel disease, hyperplastic polyposis syndrome, hereditary nonpolyposis syndrome, diverticulosis, or HIV.
-
Studies including only subjects younger than 50 years, as these subjects have lower odds of colorectal lesions as compared to subjects that are 50 years and older, who are the typical target group of screening programs.36,37
-
Studies in which nonneoplastic proximal lesions were aggregated together with neoplastic ones, and studies reporting only proximal cancer.
-
Studies focusing on subjects who underwent polypectomy.
-
Studies with internal inconsistencies inhibiting the calculation of odds ratios.
-
Studies in languages other than English.
Data Extraction
The following data were collected from each study: sample size, presence or absence of symptoms (including a positive fecal occult blood test or barium enema) in more than 50% of the population, mean age, proportion of male subjects, Western (American or European) or Eastern (Asian) population, prospective or retrospective study design, and demarcation point of distal colon (splenic flexure, 60-cm sigmoidoscope length, or rectosigmoid). An e-mail was sent to the corresponding authors of the studies with missing demographic data.
Thirty-two studies met the criteria described in the previous section. Twenty-nine studies classified subjects with respect to their most advanced distal lesion. Of the remaining three studies, one provided the number of all distal lesions per subject and the other two included a group of subjects with mixed hyperplastic and adenomatous polyps. We classified the subjects in these three studies based on their most advanced distal lesion.
Twenty-eight studies reported the number of subjects per type of distal lesion without distinguishing between single and multiple lesions, whereas the remaining four reported subjects with single and multiple lesions separately. It has previously been shown that multiple distal lesions are associated with increased odds of proximal neoplasia compared to single lesions of the same type.38,39 To conform with the methodology followed by the majority of the studies included, however, in these four studies we clustered the subjects with single and multiple lesions together and classified them according to the type of their lesions only.
OR of PN and PAN were calculated for the following distal lesions: hyperplastic polyps (HP), nonadvanced adenomas (NAA), adenomas (AD), and advanced neoplasia (AN). AN were defined as adenomas with a size of 10 mm or greater, adenomas with villous portions, high-grade dysplasias, and adenocarcinomas. Nonhyperplastic lesions were considered as normal findings. OR were calculated as the number of subjects with PN (or PAN) in the group of subjects with distal lesions compared to the number of subjects with PN (or PAN) in the reference group. OR of HP were calculated with the subjects having a normal distal colon as the reference group. OR of NAA, AD, and AN were calculated by using two reference groups: subjects with a normal distal colon, as in Lin et al.,33 and subjects with no distal neoplasia, as in Lewis et al.32 The results were not statistically different. The percentual differences in the summary OR (defined as the absolute difference of the two summary OR divided by the summary OR with the normal-distal-colon group as reference) were: NAA–PN = 5.9%, AD–PN = −1.4%, AN–PN = −3.6%, NAA–PAN = 18.9%, AD–PAN = −0.2%, and AN–PAN = 19.5%. The summary OR presented herein are based on a combination of the two reference groups: the subjects with a normal distal colon were used as the reference group; when this group was not available in a study, the reference group consisted of the subjects with no distal neoplasia instead. OR were not calculated when zero events were observed. OR were meta-analyzed using the random-effects Mantel-Haenszel method.
Absolute risks (AR) of PN and PAN were calculated for subjects with a normal distal colon, HP, NAA, AD, and AN. The absolute risk of PN (or PAN) for subjects with a certain distal-colon condition (i.e., normal, HP, NAA, AD, or AN) was defined as the percentage of subjects with PN (or PAN) and this distal-colon condition out of the total number of subjects with this condition. Proportions of IPN or IPAN were defined as the number of subjects with IPN or IPAN over the total number of subjects with PN or PAN. AR and proportions of IPN and IPAN were meta-analyzed using the DerSimonian-Laird random-effects method.
Subgroup analyses of OR and proportions of IPN and IPAN were conducted according to the presence or absence of symptoms, age younger than 60 years versus 60 years or older, proportion of males lower versus equal to or higher than 0.5, study conducted in Western or Eastern region, prospective or retrospective study design, and splenic flexure or rectosigmoid used as demarcation point. Subgroup analysis of OR was also conducted for PN and PAN prevalence lower versus equal to or higher than the median PN and PAN prevalence. A z-test was used to compare the summary odds ratios between subgroups.40 To investigate the possibility of publication bias the asymmetry of the funnel plots was assessed by Egger’s test.
RESULTS
The literature search yielded 2320 titles (Fig. 1). After excluding 748 duplicates within and among databases, 1572 abstracts were reviewed. Of these, 1324 were excluded based on the criteria described in the method section. The full texts of the remaining 248 publications were reviewed. Thirty-two publications fulfilled the criteria and were included in the meta-analysis (Table 1).
Figure 2 illustrates the sample size and the number of times each of the 32 studies was included in past meta-analyses as a function of the publication year. A significant positive correlation was found between publication year and sample size (r = 0.49, p = 0.005). A shift from prospective towards retrospective studies can also be observed, but without reaching significance (r = 0.28, p = 0.122). Of the eight studies published before 2005 but not included in the most recent meta-analysis,33 six38,41,42,46,49,51 were not taken into consideration probably because they did not provide data on HP, one54 was excluded on the grounds that it did not provide suitable HP data, and one55 was not mentioned. We used the first seven studies38,41,42,46,49,51,54 to estimate the association between AD and PN/PAN.
Table 2 shows the summary estimates of AR and OR for the association between distal lesions and proximal neoplasia. The odds of PN were higher in subjects with HP compared to those having a normal distal colon. Subjects with HP did not show evidence of increased odds of PAN. Note that only 2 of the 9 included studies yielded a significantly positive association between HP and PN. Absolute risks and odds of both PN and PAN were higher in subjects with NAA, AD, and AN than in subjects having a normal distal colon. A positive trend between the association of distal and proximal lesions and the severity of the distal markers can be noticed.
In order to estimate the proportions of IPN and IPAN, a literature search was conducted using the terms “isolated proximal” and “sigmoidoscopy” in Google Scholar, Web of Science, Scopus, and PubMed. A manual review of the references in each newly retrieved and selected article was also performed. Eight additional studies were identified in this way.
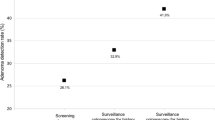
Figure 3 shows the proportions of IPN and IPAN per study. The random-effects summary estimates were 0.61 (95% CI = 0.55–0.67) and 0.58 (95% CI = 0.53–0.63) for IPN and IPAN, respectively. In the population, these proportions correspond to random-effects estimates of 0.09 (95% CI = 0.07–0.11) for IPN and 0.02 (95% CI = 0.01–0.03) for IPAN.
Forest plots with proportions of isolated proximal neoplasia (IPN, left) and isolated proximal advanced neoplasia (IPAN, right) defined as the number of subjects with IPN or IPAN over the total number of subjects with PN or PAN. The error bars are depicted at the 95% CI. The area of the squares corresponds to the weight of each study in the random-effects model. Note that some studies provided data that allowed the calculation of proportions of both IPN and IPAN. The variance of true effect sizes τ2 was 0.118 and 0.035 for IPN and IPAN, respectively.
Table 3 shows the OR after splitting the studies according to the presence of symptoms, prevalence of PN and PAN, age, proportion of males, geographic region, study design, and demarcation point of the distal colon.
Symptoms and prevalence of proximal neoplasia
Symptomatic populations with NAA showed higher odds of PN compared to asymptomatic populations. For PAN, the opposite effect held, with NAA and AN being stronger predictors in asymptomatic populations. Moreover, the association between AN and PAN was stronger in populations with a PAN prevalence lower than the median PAN prevalence of all populations for which PAN prevalence could be calculated.
Age and gender
AN were more strongly associated with PAN in younger populations. No other subgroup differences based on age or gender were found. To gain a better understanding of the moderating role of age, an additional subgroup analysis was conducted for the studies for which OR could be calculated separately for subjects younger than 50 years versus 50 years or older, and found that the OR for AN–PN and NAA–PAN were significantly higher for the subgroups of younger subjects (Table 4).
Geographic region
The NAA–PAN association was stronger in Western regions than in Eastern ones.
Study design
No differences were found between the OR of prospective and retrospective studies.
Demarcation point
The definition of demarcation point did not affect the OR of PN. Note, however, that the number of studies was limited. Odds ratios between NAA/AN and PAN were significantly higher in studies using the splenic flexure as the demarcation point as compared to the odds ratios of the studies using the rectosigmoid as demarcation. Figure 4 illustrates this effect for the association between AN and PAN.
Scatter plot of the odds ratio for the association between distal advanced neoplasia (AN) and proximal advanced neoplasia (PAN) versus the PAN prevalence for studies using the splenic flexure or the rectosigmoid as the demarcation point of the distal colon. The area of the circles represents the sample size of each study. The size of the circles in the legend corresponds to a sample size of 1000.
Subgroup analyses were also conducted for proportions of IPN and IPAN. None of the investigated factors (presence of symptoms, age, proportion of males, geographic region, study design, and demarcation point) was found to be a moderator of these proportions.
To investigate the possibility of publication bias the asymmetry of the funnel plots was assessed by Egger’s test. A slight bias inflating the association between PN and AN was found (intercept (95% CI) = −2.92 (−5.67, −0.17), p = 0.041). Because the PN–AN association is strong and generally accepted, however, we do not consider this finding to be of clinical significance. In all other lesion associations and proportions of IPN and IPAN the funnel plot asymmetry was not significant.
COMMENT
The relationship between distal lesions and proximal neoplasia
This article provided a meta-analysis of the relationship between distal lesions and proximal neoplasia as a function of lesion type. Thirty-two studies were retrieved providing information suitable for calculating odds ratios for PN and PAN. Concerning PAN, 18 studies were included, which, compared to the two studies available in past meta-analyses, resulted in more precise estimates of the summary effects. Forty studies were included for analyzing proportions of IPN and IPAN. The extent to which health, demographic, and study characteristics moderate the association between distal lesions and proximal neoplasia as well as the proportions of IPN and IPAN was also examined.
Subjects with HP showed higher odds of PN compared to subjects having a normal distal colon, whereas they did not show evidence of increased odds of PAN, in line with Lin et al.33 Subjects with NAA showed higher odds of both PN and PAN, supporting and extending Lewis et al.32 who found a significant association between NAA and PN and “potential evidence” (p. 418) but not a significant association between NAA and PAN. Note that Lewis et al.32 focused on “diminutive adenomas”, but the term had multiple definitions and we believe that the term corresponds better to NAA.
Health characteristics
PAN were better predicted in asymptomatic populations, young populations, and populations with a low PAN prevalence; that is, in low-risk groups. This supports past evidence showing that subjects diagnosed at a young age are more likely to have advanced malignancies, possibly due to genetic predispositions.64,65
Demographic characteristics
It is widely established that men have a higher and earlier risk of colonic neoplasia than women.6,10,11,20,35,42–44,52,53,58,66–71 Age and gender are interacting factors, with women younger than 50 years having a lower risk of proximal than distal neoplasia, while males in the same age group have a higher prevalence of distal than proximal neoplasia,16,65,72 women between 50 and 70 years showing an increasing incidence of proximal neoplasia compared to women of younger age,62,65,69 and gender differences diminishing after the age of 70.62 With respect to geographic region, it has been suggested that although Eastern populations have fewer incidences of isolated proximal neoplasia, lesions that are more likely distal,8,38,44,45,73–76 and a 10-year delay in the incidence of colonic neoplasia,43 Western and Eastern populations are becoming increasingly comparable due to the Westernization of the Eastern lifestyle. Note that the existing information concerns prevalences. We found no differences between genders and geographic regions regarding the association between distal lesions and proximal neoplasia.
Study design characteristics
The study of Lin et al.,33 the only meta-analysis investigating the moderating effect of the demarcation point of the distal colon, reported no clinically significant differences in lesion associations between studies using a different demarcation point. We found that studies using the splenic flexure as demarcation yielded significantly higher OR between NAA/AN and PAN compared to studies using the rectosigmoid as demarcation. Note that the majority of the colonoscopy studies used the splenic flexure as the demarcation point, but this does not reflect clinical practice, in which the sigmoidoscope may not reach the area beyond the rectosigmoid in more than 60% of procedures.77,78 The association between NAA/AN and PAN is thus likely weaker in a screening setting than the estimates provided in studies using the splenic flexure as demarcation.
Proportions of IPN and IPAN
The summary estimates of percent proportions of subjects with IPN and IPAN were about 60%, which is higher than the estimates of about 50% provided in past meta-analyses. We found no subgroup differences of demographic factors for proportions of either IPN or IPAN. Note that our analysis concerned the proportion of subjects with IPN and IPAN, and not the population prevalence of IPN and IPAN which is affected by the general prevalence of PN and PAN (i.e., accompanied by distal lesions or not). That is, the increasing population prevalence of IPN with age reported in previous studies30,79 is due, at least in part, to the increasing prevalence of proximal/colonic neoplasia with age, no matter whether the proximal neoplasia are isolated or not.
Study Limitations
Self-selection
A number of biases may have affected the results of the meta-analysis. First, the subjects in the studies were likely to be more health-conscious and aware of preventive medicine than the general population.9,15,37,42,55,80,81 Moreover, most studies were conducted in university hospitals and medical centers in urban areas,19,53 or in private clinics requiring private health insurance42,82 and compensations as high as $500,19 possibly contributing to self-selection bias.
Misclassification and misses
Other sources of bias are lesion misses, false positives, and lesion misclassification. Miss rates of about 26% and 13% of adenomas smaller than 5 mm and between 5 and 10 mm, respectively, have been reported.83,84 Small adenomas may be misclassified as HP,85,86 and adenomatous changes in a portion of HP may not be noticed without histological examination. Moreover, endoscopists usually compare the size of polyps to the width of biopsy forceps, which has been associated with underestimation of polyp size.87,88
Dichotomization
The subgroup analyses relied on dichotomized age, gender, and PN/PAN prevalence groups. This approach may have led to power loss and reduced measurement reliability.89
Technological advances
The included studies spanned more than two decades. Technical advances in colonoscopy, such as high-definition imaging90,91 and optimization of withdrawal techniques92–94 have improved the detection of lesions, particularly of those between 0 and 5 mm.93 The analyses were repeated separately for the studies published before or after 2000 and before or after 2005 and no statistically significant differences in the reported odds ratios and proportions of IPN and IPAN were found.
CONCLUSION
The present results are important for identifying persons who may need to undergo a colonoscopy. We found that all types of distal lesions are predictive of proximal neoplasia and that PAN are better predicted by distal lesions in low-risk groups. The association between distal lesions and proximal neoplasia increased with the severity of the distal lesion. The fact that more than half of the proximal neoplasia are isolated urges the investigation of other risk factors, including genetic predisposition and environmental risks, which could contribute to predicting proximal neoplasia.
Although a number of screening programs employ colonoscopy, flexible sigmoidoscopy will probably gain territory in view of the results of four large-scale randomized clinical trials of screening flexible sigmoidoscopy performed in Norway (NORCCAP),95 the UK (UKFSST),96 Italy (SCORE),97 and the US (PLCO).98 NORCCAP reported a reduction of 76% for distal colorectal cancer, and in UKFSST the incidence of colorectal cancer was reduced by 33% and the corresponding mortality by 40% (see also99 for a review and meta-analysis). UKFSST found no effect of screening on the incidence of proximal cancer. It remains to be observed whether a reduced incidence of colorectal cancer and corresponding mortality will occur in the other two trials, in which the criteria for colonoscopy referral are closer to those in the present meta-analysis.
REFERENCES
Benson VS, Patnick J, Davies AK, Nadel MR, Smith RA, Atkin WS. Colorectal cancer screening: A comparison of 35 initiatives in 17 countries. Int J Cancer. 2008;122:1357–67.
Winawer SJ, Zauber AG. The advanced adenoma as the primary target of screening. Gastrointest Endosc Clin N Am. 2002;12:1–9.
Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: A consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. CA Cancer J Clin. 2006;56:143–59.
Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58:130–60.
Institute for Clinical Systems Improvement. Health care guideline: Colorectal cancer screening. Thirteenth edition, 2010. Available from: http://www.icsi.org/colorectal_cancer_screening/colorectal_cancer_screening_5.html.
Binda V, Pereira-Lima J, Nunes CA, Falkemberg LT, Azambuja DB, Cruz JV. Is there a role for sigmoidoscopy in symptomatic patients? Analysis of a study correlating distal and proximal colonic neoplasias detected by colonoscopy in a symptomatic population. Arq Gastroenterol. 2007;44:2–7.
Brady PG, Straker RJ, McClave SA, Nord HJ, Pinkas M, Robinson BE. Are hyperplastic rectosigmoid polyps associated with an increased risk of proximal colonic neoplasms? Gastrointest Endosc. 1993;39:481–5.
Foutch PG, DiSario JA, Pardy K, Mai HD, Manne RK. The sentinel hyperplastic polyp: A marker for synchronous neoplasia in the proximal colon. Am J Gastroenterol. 1991;86:1482–5.
Lieberman DA, Smith FW. Screening for colon malignancy with colonoscopy. Am J Gastroenterol. 1991;86:946–51.
Lin OS, Schembre DB, McCormick SE, et al. Risk of proximal colorectal neoplasia among asymptomatic patients with distal hyperplastic polyps. Am J Med. 2005;118:1113–9.
Pennazio M, Arrigoni A, Risio M, Spandre M, Rossini FP. Small rectosigmoid polyps as markers of proximal neoplasms. Dis Colon Rectum. 1993;36:1121–5.
Provenzale D, Martin ZZ, Holland KL, Sandler RS. Colon adenomas in patients with hyperplastic polyps. J Clin Gastroenterol. 1988;10:46–9.
Provenzale D, Garrett JW, Condon SE, Sandler RS. Risk for colon adenomas in patients with rectosigmoid hyperplastic polyps. Ann Intern Med. 1990;113:760–3.
Rex DK, Smith JJ, Ulbright TM, Lehman GA. Distal colonic hyperplastic polyps do not predict proximal adenomas in asymptomatic average-risk subjects. Gastroenterology. 1992;102:317–9.
Byeon JS, Yang SK, Kim TI, et al. Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc. 2007;65:1015–22.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Using risk for advanced proximal colonic neoplasia to tailor endoscopic screening for colorectal cancer. Ann Intern Med. 2003;139:959–65.
Leung WK, Ho KY, Kim W, et al. Colorectal neoplasia in Asia: a multicenter colonoscopy survey in symptomatic patients. Gastrointest Endosc. 2006;64:751–9.
Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162–8.
Liou JM, Lin JT, Huang SP, et al. Screening for colorectal cancer in average-risk Chinese population using a mixed strategy with sigmoidoscopy and colonoscopy. Dis Colon Rectum. 2007;50:630–40.
Liu HH, Wu MC, Peng Y, Wu MS. Prevalence of advanced colonic polyps in asymptomatic Chinese. World J Gastroenterol. 2005;11:4731–4.
Jass JR, Iino H, Ruszkiewicz A, et al. Neoplastic progression occurs through mutator pathways in hyperplastic polyposis of the colorectum. Gut. 2000;47:43–9.
Hawkins NJ, Ward RL. Sporadic colorectal cancers with microsatellite instability and their possible origin in hyperplastic polyps and serrated adenomas. J Natl Cancer Inst. 2001;93:1307–13.
Böhm SK. Hyperplastic polyps of the colorectum—Do they possess a malignant potential? The molecular classification of colorectal cancer and the serrated pathway. Gastrointest Oncol. 2002;4:97–117.
Boland CR, Montgomery CK, Kim YS. A cancer associated mucin alteration in benign colonic polyps. Gastroenterology. 1982;82:664–72.
O'Brien MJ, O'Keane JC, Zauber A, Gottlieb LS, Winawer SJ. Precursors of colorectal carcinoma. Biopsy and biologic markers. Cancer. 1992;70:1317–27.
Mysliwiec PA, Brown ML, Klabunde CN, Ransohoff DF. Are physicians doing too much colonoscopy? A national survey of colorectal surveillance after polypectomy. Ann Intern Med. 2004;141:264–71.
Farraye FA, Wallace M. Clinical significance of small polyps found during screening with flexible sigmoidoscopy. Gastrointest Endosc Clin N Am. 2002;12:41–51.
Levin TR, Palitz A, Grossman S, et al. Predicting advanced proximal colonic neoplasia with screening sigmoidoscopy. JAMA. 1999;281:1611–7.
Gondal G, Grotmol T, Hofstad B, Bretthauer M, Eide TJ, Hoff G. Grading of distal colorectal adenomas as predictors for proximal colonic neoplasia and choice of endoscope in population screening: experience from the Norwegian Colorectal Cancer Prevention study (NORCCAP). Gut. 2003;52:398–403.
Anderson JC, Alpern Z, Messina CR, et al. Predictors of proximal neoplasia in patients without distal adenomatous pathology. Am J Gastroenterol. 2004;99:472–7.
Dave S, Hui S, Kroenke K, Imperiale TF. Is the distal hyperplastic polyp a marker for proximal neoplasia? A systematic review. J Gen Inten Med. 2003;18:128–37.
Lewis JD, Ng K, Hung KE, Bilker WB, Berlin JA, Brensinger C, Rustgi AK. Detection of proximal adenomatous polyps with screening sigmoidoscopy. A systematic review and meta-analysis of screening colonoscopy. Arch Intern Med. 2003;163:413–20.
Lin OS, Gerson LB, Soon MS, Schembre DB, Kozarek RA. Risk of proximal colon neoplasia with distal hyperplastic polyps. A meta-analysis. Arch Intern Med. 2005;165:382–90.
Lieberman D. Race, gender, and colorectal cancer screening. Am J Gastroenterol. 2005;100:2756–8.
Nelson RL, Persky V, Turyk M. Carcinoma in situ of the colorectum: SEER trends by race, gender, and total colorectal cancer. J Surg Oncol. 1999;71:123–9.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Results of screening colonoscopy among persons 40 to 49 years of age. N Engl J Med. 2002;346:1781–5.
Strul H, Kariv R, Leshno M, et al. The prevalence rate and anatomic location of colorectal adenoma and cancer detected by colonoscopy in average-risk individuals aged 40–80 years. Am J Gastroenterol. 2006;101:255–62.
Hammer K, Hammer J, Oesterreicher C, Pötzi R. Advanced distal colonic lesions as predictors of advanced lesions in the proximal colon. Medicine. 2000;79:127–34.
O'Brien K, Sweeney BF Jr, Conger N, Fischer JR, Lang KA. Prevalence of proximal adenomas after an adenoma is found on flexible sigmoidoscopy. Cancer Detect Prev. 2003;27:259–65.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. UK: West Sussex, John Wiley & Sons, Ltd.; 2009.
Ang YS, Macaleenan N, Mahmud N, Keeling PWN, Kelleher DP, Weir DG. The yield of colonoscopy in average-risk patients with non-specific colonic symptoms. Eur J Gastroenterol Hepatol. 2002;14:1073–7.
Betés Ibáñez M, Muñoz-Navas MA, Duque JM, et al. Diagnostic value of distal colonic polyps for prediction of advanced proximal neoplasia in an average-risk population undergoing screening colonoscopy. Gastrointest Endosc. 2004;59:634–41.
Choe JW, Chang HS, Yang SK, et al. Screening colonoscopy in asymptomatic average-risk Koreans: Analysis in relation to age and sex. J Gastroenterol Hepatol. 2007;22:1003–8.
Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, Sohn JH. Risk of advanced proximal adenoma and cancer according to rectosigmoid findings in the Korean population. Dig Dis Sci. 2006;51:2206–12.
Erarslan E, Turkay C, Isik A, Uz B, Kaya A, Bavbek N. Prevalence of proximal neoplasms among asymptomatic patients according to distal colorectal findings. Dig Dis Sci. 2009;54:1312–6.
Ikeda Y, Mori M, Miyazaki M, Yoshizumi T, Maehara Y, Sugimachi K. Significance of small distal adenoma for detection of proximal neoplasms in the colorectum. Gastrointest Endosc. 2000;52:358–61.
Johnson DA, Gurney MS, Volpe RJ, et al. A prospective study of the prevalence of colonic neoplasms in asymptomatic patients with an age-related risk. Am J Gastroenterol. 1990;85:969–74.
Kadakia SC, Wrobleski CS, Kadakia AS, Meier NJ. Prevalence of proximal colonic polyps in average-risk asymptomatic patients with negative fecal occult blood tests and flexible sigmoidoscopy. Gastrointest Endosc. 1996;44:112–7.
Khan A, Shrier I, Gordon PH. Do distal adenomas mandate total colonoscopy? Surg Endosc. 2003;17:886–90.
Nicholson FB, Korman MG, Stern AI, Hansky J. Distribution of colorectal adenomas: implications for bowel cancer screening. Med J Aust. 2000;172:428–30.
Odelowo OO, Hoque M, Begum R, Islam KK, Smoot DT. Colonoscopy for colorectal cancer screening in African Americans. J Assoc Acad Minor Phys. 2002;13:66–8.
Okamoto M, Kawabe T, Yamaji Y, et al. Rectosigmoid findings are not associated with proximal colon cancer: Analysis of 6 196 consecutive cases undergoing total colonoscopy. World J Gastroenterol. 2005;11:2249–54.
Park HW, Byeon JS, Yang SK, et al. Colorectal neoplasm in asymptomatic average-risk Koreans: The KASID prospective multicenter colonoscopy survey. Gut Liver. 2009;3:35–40.
Sciallero S, Costantini M, Bertinelli E, et al. Distal hyperplastic polyps do not predict proximal adenomas: results from a multicentric study of colorectal adenomas. Gastrointest Endosc. 1997;46:124–30.
Thiis-Evensen E, Hoff GS, Sauar J, Majak BM, Vatn MH. Flexible sigmoidoscopy or colonoscopy as a screening modality for colorectal adenomas in older age groups? Findings in a cohort of the normal population aged 63–72 years. Gut. 1999;45:834–9.
Al-Enezi SA, Alsurayei SA, Ismail AE, Aly NYA, Ismail WA, Abou-Bakr AA. Adenomatous colorectal polyps in patients referred for colonoscopy in a regional hospital in Kuwait. Saudi J Gastroenterol. 2010;16:188–93.
Castiglione G, Ciatto S, Mazzotta A, Grazzini G. Sensitivity of screening sigmoidoscopy for proximal colorectal tumours. Lancet. 1995;354:729–7.
Chiu HM, Wang HP, Lee YC, et al. A prospective study of the frequency and the topographical distribution of colon neoplasia in asymptomatic average-risk Chinese adults as determined by colonoscopic screening. Gastrointest Endosc. 2005;61:547–53.
Gryska RV, Cohen AM. Screening asymptomatic patients at high risk for colon cancer with full colonoscopy. Dis Colon Rectum. 1987;30:18–20.
Kim DH, Lee SY, Choi KS, et al. The usefulness of colonoscopy as a screening test for detecting colorectal polyps. Hepato-Gastroenterology. 2007;54:2240–2.
Lieberman DA, Smith FW. Frequency of isolated proximal colonic polyps among patients referred for colonoscopy. Arch Intern Med. 1988;148:473–5.
Schoenfeld P, Cash B, Flood A, et al. Colonoscopic screening of average-risk women for colorectal neoplasia. N Engl J Med. 2005;352:2061–8.
Soon M-W, Soon A, Lin T-Y, Lin OS. Distribution of colon neoplasia in Chinese patients: implications for endoscopic screening strategies. Eur J Gastroenterol Hepatol. 2008;20:642–7.
Negri E, Braga C, La Vecchia C, et al. Family history of cancer and risk of colorectal cancer in Italy. Br J Cancer. 1998;77:174–9.
Slattery ML, Friedman GD, Potter JD, Edwards S, Caan BJ, Samowitz W. A description of age, sex, and site distributions of colon carcinoma in three geographic areas. Cancer. 1996;78:1666–70.
Rex DK, Lehman GA, Ulbright TM, et al. Colonic neoplasia in asymptomatic persons with negative fecal occult blood tests: Influence of age, gender, and family history. Am J Gastroenterol. 1993;88:825–31.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000;343:169–74.
McCashland TM, Brand R, Lyden E, De Garmo P. Gender differences in colorectal polyps and tumors. Am J Gastroenterol. 2001;96:882–6.
Australian Institute of Health and Welfare and the Australasian Association of Cancer Registries. Cancer in Australia 1991-1994 (with projections to 1999). Canberra: AIHW, 1998.
Brenner H, Hoffmeister M, Stegmaier C, Brenner G, Altenhofen L, Haug U. Risk of progression of advanced adenomas to colorectal cancer by age and sex: estimates based on 840 149 screening colonoscopies. Gut. 2007;56:1585–9.
Nguyen SP, Bent S, Chen YH, Terdiman JP. Gender as a risk factor for advanced neoplasia and colorectal cancer: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7:676–81.
Chao A, Gilliland FD, Hunt WC, Bulterys M, Becker TM, Key CR. Increasing incidence of colon and rectal cancer among Hispanics and American Indians in New Mexico (United States), 1969–94. Cancer Causes Control. 1998;9:137–44.
Qing SH, Rao KY, Jiang HY, Wexner SD. Racial differences in the anatomical distribution of colorectal cancer: a study of differences between American and Chinese patients. World J Gastroenterol. 2003;9:721–5.
Francois F, Park J, Bini EJ. Colon pathology detected after a positive screening flexible sigmoidoscopy: a prospective study in an ethnically diverse cohort. Am J Gastroenterol. 2006;101:823–30.
Theuer CP, Taylor TH, Brewster WR, Campbell BS, Becerra JC, Anton-Culver H. The topography of colorectal cancer varies by race/ethnicity and affects the utility of flexible sigmoidoscopy. Am Surg. 2001;67:1157–61.
Soon MS, Kozarek RA, Ayub K, Soon A, Lin TY, Lin OS. Screening colonoscopy in Chinese and Western patients: A comparative study. Am J Gastroenterol. 2005;100:2749–55.
Painter J, Saunders DB, Bell GD, Williams CB, Pitt R, Bladen J. Depth of insertion at flexible sigmoidoscopy: implications for colorectal cancer screening and instrument design. Endoscopy. 1999;31:227–31.
Kronborg O. Colon polyps and cancer. Endoscopy. 2000;32:124–30.
Boursi B, Halak A, Umansky M, Galzan L, Guzner-Gur H, Arber N. Colonoscopic screening of an average-risk population for colorectal neoplasia. Endoscopy. 2009;41:516–21.
Keren D, Rainis T, Goldstein O, Stermer E, Lavy A. Significant colonic neoplasia prevalence and ASGE recommendations. Is it time for a change? J Clin Gastroenterol. 2008;42:886–91.
Farrands PA, Hardcastle JD, Chamberlain J, Moss S. Factors affecting compliance with screening for colorectal cancer. Community Med. 1984;6:12–9.
Chao A, Connell CJ, Cokkinides V, Jacobs EJ, Calle EE, Thun MJ. Underuse of screening sigmoidoscopy and colonoscopy in a large cohort of US adults. Am J Public Health. 2004;94:1775–81.
Van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, Van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006;101:343–50.
Rex DK, Cutler CS, Lemmel GT, et al. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997;112:24–8.
Norfleet RG, Ryan ME, Wyman JB. Adenomatous and hyperplastic polyps cannot be reliably distinguished by their appearance through the fiberoptic sigmoidoscope. Dig Dis Sci. 1988;33:1175–7.
Neale AV, Demers RY, Budev H, Scott RO. Physician accuracy in diagnosing colorectal polyps. Dis Colon Rectum. 1987;30:247–50.
Schoen RE, Gerber LD, Margulies C. The pathologic measurement of polyp size is preferable to the endoscopic estimate. Gastrointest Endosc. 1997;46:492–6.
Gopalswamy N, Shenoy VN, Choudhry U, et al. Is in vivo measurement of size of polyps during colonoscopy accurate? Gastrointest Endosc. 1997;46:497–502.
MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7:19–40.
Tribonias G, Theodoropoulou A, Konstantinidis K, et al. Comparison of standard versus high-definition, wide-angle colonoscopy for polyp detection: a randomized controlled trial. Colorectal Dis. 2010;12:e260–6.
Rex D. Detection of neoplasia at colonoscopy: what next? Endoscopy. 2008;40:333–5.
Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355:2533–41.
East JE, Stavrindis M, Thomas-Gibson S, Guenther T, Tekkis PP, Saunders BP. A comparative study of standard vs. high definition colonoscopy for adenoma and hyperplastic polyp detection with optimized withdrawal technique. Aliment Pharmacol Ther. 2008;28:768–76.
Rex DK. Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc. 2000;51:33–6.
Hoff G, Grotmol T, Skovlund E, Bretthauer M. Risk of colorectal cancer seven years after flexible sigmoidoscopy screening: randomised controlled trial. BMJ. 2009;338:b1846.
Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–33.
Segnan N, Senore C, Andreoni B, et al. Baseline findings of the Italian multicentre randomised controlled trial of “once-only sigmoidoscopy”—SCORE. J Natl Cancer Inst. 2002;94:1763–72.
Weissfeld JL, Schoen RE, Pinsky PF, et al. Flexible sigmoidoscopy in the PLCO cancer screening trial: results from the baseline screening examination of a randomized trial. J Natl Cancer Inst. 2005;97:989–97.
Bretthauer M. Colorectal cancer screening. J Intern Med. 2011;270:87–98.
ACKNOWLEDGMENTS
The research of Dimitra Dodou and Joost de Winter is supported by the Dutch Technology Foundation (STW), applied science division of the Netherlands Organisation for Scientific Research (NWO) and the Technology Program of the Ministry of Economic Affairs. Preliminary results of this work were presented at a poster session during the 3rd Dutch Biomedical Engineering Conference, Egmond aan Zee, The Netherlands, January 20–21, 2011.
Conflict of Interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dodou, D., de Winter, J.C.F. The Relationship Between Distal and Proximal Colonic Neoplasia: A Meta-Analysis. J GEN INTERN MED 27, 361–370 (2012). https://doi.org/10.1007/s11606-011-1919-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1919-y