ABSTRACT
BACKGROUND
Cancer survivorship care is not adequately addressed in current medical school curricula.
OBJECTIVES
To develop, implement, and evaluate a modular cancer survivorship curriculum that is portable to other educational settings and is designed to provide medical students with a foundation of knowledge, attitudes, and skills related to care for cancer survivors.
PROGRAM DESCRIPTION
An expert consensus panel developed a set of learning objectives related to cancer survivorship to guide the development of educational modules, such as computer-based self-instructional modules, problem-based learning cases, videos, and clinical exercises. Course and clerkship chairs were directly involved in the development and implementation of the modules.
EVALUATION
A cohort study with a historical control group demonstrated that fourth-year medical students increased their knowledge in survivorship issues and their self-reported level of comfort in care activities compared to similar students who did not receive the survivorship curriculum.
CONCLUSIONS
Our framework resulted in a cancer survivorship curriculum that was implemented in a modular manner across the medical curriculum that improved learning and that is potentially portable to other educational settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Thanks to recent advances in cancer screening, treatment, and prevention of recurrent malignancies, most cancer patients today can be expected to survive more than 5 years from the point of diagnosis. The overall 5-year relative survival rate now exceeds 65 percent1. Emerging therapeutic interventions such as personalized genomic therapy2 are likely to improve long-term outcomes for cancer survivors even more. General internists and family practitioners, by far the largest group of providers of survivorship care3, are encountering long-term cancer survivors in increasing numbers. However, they are not necessarily prepared to recognize the unique and life-long needs of these patients related to their previous cancer diagnosis and treatment4.
While medical schools have traditionally focused on the diagnosis and treatment of cancer, and more recently on its prevention5,6, curricula focusing on cancer survivorship are still rare3. Consequently, trainees may feel more prepared to address acute manifestations of oncologic disease than to care for more stable patients with a history of cancer7. Cancer survivors have now joined the group of patients with other chronic diseases who are generally underrepresented in medical school curricula8, and towards whom students’ attitudes decline during training9. A successful educational framework for developing a survivorship curriculum is bound to be complex as it involves multidisciplinary teams of specialists, primary care providers, and, ideally, longitudinal experience with patients.
AIM
In this paper we describe a framework for the development, implementation, evaluation, and dissemination of a curriculum that is portable to other educational settings and is designed to provide medical students with a foundation of knowledge, attitudes, and skills related to cancer survivorship.
PROGRAM DESCRIPTION
During the last 5 years (from 2003 through 2008), the David Geffen School of Medicine at UCLA, the University of California, San Francisco School of Medicine, and the Charles Drew University of Medicine and Science (CDU) have collaboratively developed a 4-year, integrated curriculum in cancer survivorship with support of an NCI R25 grant. Development of this curriculum occurred in several phases: (1) identification of curriculum objectives; (2) development of educational interventions and integration into the existing curriculum; (3) evaluation and dissemination. The curriculum focused on common cancers with increasing survival rates: breast, colorectal, prostate, and gynecological cancers along with childhood cancers such as leukemia.
-
1.
Identification of curriculum objectives
A 15-member multidisciplinary expert consensus panel with representation from the three participating institutions was charged with developing a set of curriculum objectives for the care of patients with cancer as a chronic disease10. Faculty members from various oncology specialties, primary care, and curriculum design specialists met at each of the institutions and created comprehensive lists of knowledge, attitudes, and skills related to survivorship care that medical students should demonstrate upon graduation. Next, using a modified Delphi process, panel members prioritized all items on the collated list, resulting in a final set of 17 objectives. Knowledge objectives pertained to epidemiology of survival, survival rates, psychosocial effects of cancer, and long-term effects of treatment. Skill objectives included, but were not limited to, provide recommendations for secondary prevention of cancer, prescribe appropriate pain medication, give bad news about a second malignancy, and locate current cancer information. The complete list of curriculum objectives has appeared in the Institute of Medicine report, From Cancer Patient to Cancer Survivors: Lost in Translation 3 and elsewhere11.
-
2.
Development and implementation of educational interventions
Curriculum objectives guided the development of educational interventions addressing specific cancers12. A modular approach was taken as opposed to developing a new course or clerkship. That is, smaller stand-alone units that supported a limited number of objectives were created to allow integration into existing courses and clerkships. The resulting set of approximately 30 educational modules used a variety of educational strategies (see Table 1 for a complete overview). The following is a representative sample:
-
(1)
The case of Mrs. Hernandez: a video problem-based learning (PBL) case
This video-based PBL case features Mrs. Hernandez, a 56-year-old immigrant from Mexico, who presents to an urgent care physician with chest pain and cough. She is initially diagnosed with pneumonia. Her symptoms progress, and she is subsequently diagnosed with stage IIIA adenocarcinoma of the lung, which is treated with chemotherapy and radiotherapy. The case ends with a 6-month follow-up visit when the patient is in remission, and the physician must discuss her concerns about recurrence of her cancer and her health beliefs. Students learn to describe the pathophysiology of lung cancer, the relationship between staging and prognosis, and the factors affecting the patient’s quality of life after treatment.
-
(2)
Surviving endometrial cancer: a computer-based self-study module
In this module, students encounter a 64-year-old woman who visits her primary care physician after being treated for Stage 2A endometrial cancer. Over the subsequent 20 months, she returns to the physician several times for a variety of complaints, including hair loss, swollen feet, weight loss, and concerns about recurrence of the cancer. At her 1-year checkup with the oncologist, she is diagnosed with a para-aortic lymph node indicative of a localized relapse. With each visit, the student is required to make diagnostic, treatment, and counseling decisions.
-
(3)
The human side of survivorship: panel and theater presentation of cancer survivors
First-year medical students have an opportunity to see the human side of survivorship issues through a 90-min panel presentation. The panel occurs during a week in which the students analyze skin biopsies from patients with malignant melanoma. Three or four cancer survivors tell their stories, starting with how they were diagnosed and treated. They then discuss the impact of cancer and treatment on their relationships, jobs, and self-perception. They describe how they coped with interacting with multidisciplinary teams, their use of complementary or alternative medicine, and any insurance issues they encountered. Students have reviewed this panel presentation very positively and are grateful for this glimpse into the cancer experience. In addition, students have a chance to see a one-woman show on the experience of being a cancer survivor (Jonna’s Body13). Dramatic story telling and humor create emotional links for students to the survivorship experience.
-
(4)
Cancer survivorship write-up exercise
In this exercise, students identify a cancer survivor among the patients for whom they are caring during their inpatient internal medicine clerkship. The patient may or may not have been hospitalized because of a cancer-related problem. Guided by a template, they conduct and then write up a detailed cancer history of the patient, including details of cancer treatment and follow-up. In addition to the usual history and physical examination findings, students are prompted to address quality of life issues, pain control, advance directives, and secondary screening. This write-up exercise is designed to prompt students to identify cancer survivors during their clerkship, increase their awareness of survivorship issues, and to conduct a detailed cancer history.
Having a pre-clerkship curriculum that includes PBL, innovative laboratory sessions, and a longitudinal “Doctoring” course facilitated the insertion of the modules. PBL survivor cases could be offered to course chairs to replace existing cases with similar learning goals but lacking a survivor focus. The “Doctoring” course chairs helped develop and implement the majority of skill-based modules in their course including the panel of cancer survivors, behavior change counseling, and advanced directives. The same implementation strategy worked for the clerkships as well. By involving clerkship chairs and site directors at UCSF, CDU, and UCLA in curriculum development, knowledge-oriented modules could be inserted in clerkships in internal medicine, surgery, and obstetrics/gynecology. A limitation to this approach is the need to negotiate for the needed curricular time for the integration of these new materials.
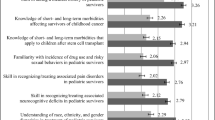
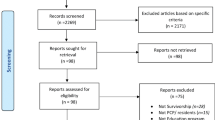
PROGRAM EVALUATION
Students evaluated the usefulness of each curricular module and provided suggestions for improvement. In addition, we used a cohort study with a historical control group to assess the effect of the curriculum on students’ knowledge of and experience with cancer survivorship. In 2004, we developed an instrument to measure students’ fund of knowledge on survivorship issues (25 multiple choice questions) and their self-rated comfort levels in survivorship care (nine items rated on a five-point Likert scale)14. This survey instrument is available online. Questionnaire items covered the five cancer types addressed in the curriculum and yielded acceptable reliability levels (Chronbach’s alpha = 0.67). We determined discriminant validity with a group of oncology fellows, who performed significantly better than medical students. In addition, we asked students to estimate how many times during medical school they had observed someone else caring for survivors, received direct instruction or practiced specific skills related to cancer survivors. Prior to implementing the new curriculum, we administered the instrument to a historical control group in 200515,16 and in subsequent years as the curriculum was phased in.
The historical control group consisted of 211 fourth-year medical students at the three participating programs (Class of 2006). These students had not experienced a dedicated cancer survivorship curriculum. The intervention group consisted of 195 students in the Class of 2007 who had been exposed to a different combination of modules at each institution, 10 modules at UCSF, 19 at UCLA, and 20 at CDU.
The control group demonstrated the serious shortcomings of the educational status quo7. They lacked knowledge in key survivorship issues, such as long-term consequences of cancer treatments. Furthermore, while all students reported some contact with cancer survivors during their clerkships, less then half received direct instruction or were afforded the opportunity to practice critical components of survivorship care.
Educational outcomes gradually improved as the cancer survivorship modules were introduced into the curriculum17. Compared to the historical controls, the intervention groups at UCLA and CDU improved their scores on average by about 43% (p < 0.001). Students at UCSF, where fewer modules were implemented, did not demonstrate such a knowledge gain. Students at all institutions, however, reported to be more comfortable in several care activities (p < 0.05), including working in a specialty team and identifying patients with high cancer recurrence risks. Students also reported having encountered more cancer survivors compared to the control group. Whereas in previous years cancer survivors may have rarely been identified as such, the emphasis of the new curriculum on taking a cancer history may have raised the awareness among medical students of cancer survivors presenting in clinics and on ward rotations.
DISSEMINATION
Most of the educational modules of our cancer survivorship curriculum are stand-alone and, thus, can be easily shared with other institutions. Many of them have been showcased at the annual meeting of the American Association for Cancer Education18 and at the Innovations in Medical Education Exhibits during the annual meeting of the Association of American Medical Colleges19. We also created a dedicated website20 where many of the materials can be downloaded or requested free of charge.
DISCUSSION
Appropriate training of future physicians is needed, regardless of specialty, to address the unique needs of the rapidly increasing population of cancer survivors. New models of delivering survivorship care are still being proposed21, and consequently, training across the continuum will need to be adapted continuously. Our modular approach facilitated the implementation and integration of our interventions across the 4 years of medical school at diverse institutions, provided maximum flexibility to incorporate emerging treatment options, and yielded portable products that were easily disseminated to other institutions. The development of curriculum objectives by an expert consensus panel drove the development of specific interventions. Having faculty members who could champion these objectives with their colleagues who serve as course and clerkship chairs was an essential component for success.
The gradual introduction of our curriculum was associated with an improvement in knowledge and comfort levels related to survivorship care and raised students’ awareness of survivors. Our evaluation strategy, however, lacked objective evaluation of students’ skills either by patients or trained observers. Thus, the effect of our curriculum on actual survivorship care (beyond knowledge, attitudes, and experience) was not determined.
In sum, our framework resulted in a cancer survivorship curriculum that was flexibly implemented at multiple sites using a modular approach and strategic involvement of curricular leaders. Students demonstrated improved learning and more survivorship experience over controls. The resulting modules are adaptable for a variety of health profession students and can be integrated into existing courses and clerkships with appropriate negotiation.
References
Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK (eds). SEER Cancer Statistics Review, 1975–2005, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2005/. [Assessed on April 2, 2009]
Garman KS, Nevins JR, Potti A. Genomic strategies for personalized cancer therapy. Hum Mol Genet. 2007; 16Spec No. 2: R226–32.
Institute of Medicine. From Cancer Patient to Cancer Survivor: Lost in Translation, Survivorship Report. Washington, DC, National Academy Press, 2006.
Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: A new challenge in delivering quality care. J Clin Oncol. 2006; 2432: 5101–4.
Hauer KE, Wilkerson L, Teherani A. The relationship between medical students’ knowledge, confidence, experience, and skills related to colorectal cancer screening. J Cancer Educ. 2008; 234: 209–13.
Lee M, Wilkerson L, Harrity S, Hodgson CS. Differences in cancer prevention knowledge and experience among medical students at three institutions over time. J Cancer Educ. 2006; 214: 223–9.
Uijtdehaage S, Hauer KE, et al. Preparedness for caring of cancer survivors: a multi-institutional study of medical students and oncology fellows. J Cancer Educ. 2009; 241: 28–32.
Pham HH, Simonson L, Elnicki DM, Fried LP, Goroll AH, Bass EB. Training US medical students to care for the chronically ill. Acad Med. 2004; 791: 32–40.
Arenson CA, Rattner S, Borden C, Collins L, Fields SK, Gavin E, Veloski JJ. Cross-sectional assessment of medical and nursing students’ attitudes toward chronic illness at matriculation and graduation. Acad Med. 2008; 8310 Suppl: S93–6.
Stuber M, Guiton G, Wilkerson L. Cancer as a chronic illness: Competencies for a curriculum for medical students. J Cancer Educ. 2003; 183 Suppl: 23.
Ferrell BR, Winn R. Medical and nursing education and training opportunities to improve survivorship care. J Clin Oncol. 2006; 2432: 5142–8.
Stuber M, Wilkerson L, Go VL. Integration of cancer survivorship coursework into first year medical school curriculum. J Cancer Educ. 2004; 193, Suppl: 35.
Jonna Tomases. Jonna’s body, please hold. http://www.jonnasbody.com. [Accessed on April 2, 2009]
Wilkerson L, Go VL, Stuber M, Uijtdehaage S. Developing instruments to measure knowledge and experience related to cancer survivorship. J Cancer Educ. 2005; 203, Suppl: 16.
Uijtdehaage S, Hauer K, Wilkerson L, Stuber M, Go VL, Rajagopalan S. Cancer survivorship: What do medical students know? J Cancer Educ. 2006; 212, Suppl: 37.
Uijtdehaage S, Wilkerson L, Stuber M, Go VL, Hauer K, Rajagopalan S. Cancer survivorship: What do medical students experience? J Cancer Educ. 2006; 212, Suppl: 17.
Uijtdehaage S, Hauer K, Rajagopalan S, Wilkerson L. Improving knowledge of and experience with cancer survivors: Effects of a dedicated curriculum. J Cancer Educ. 2007; 224, Suppl: 72.
American Association for Cancer Education. www.aaceonline.com. [Accessed on April 2, 2009]
Association of American Medical Colleges. Innovations In Medical Education Exhibits. http://www.aamc.org/members/gea/. [Assessed on April 2, 2009].
David Geffen School of Medicine, UCLA. UCLA Cancer Survivorship. http://www.medsch.ucla.edu/cancersurvivorship/. [Accessed on April 2, 2009].
Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006; 2432: 5117–24.
Acknowledgements
This research study was made possible by a grant from the National Cancer Institute, R25 CA096975, 2002–2007, (PI: LuAnn Wilkerson). The authors wish to acknowledge the contributions of Patricia Ganz, MD, to the initiation of this project.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the Electronic supplementary material.
ESM 1
(PDF 168 KB)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Uijtdehaage, S., Hauer, K.E., Stuber, M. et al. A Framework for Developing, Implementing, and Evaluating a Cancer Survivorship Curriculum for Medical Students. J GEN INTERN MED 24 (Suppl 2), 491–494 (2009). https://doi.org/10.1007/s11606-009-1024-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1024-7