Abstract
Background
Perioperative hyperglycemia is a known risk factor for postoperative complications after colorectal surgery. The aim of this study was to investigate whether intraoperative blood glucose values are associated with colorectal anastomotic leakage in diabetic and non-diabetic patients undergoing colorectal surgery.
Methods
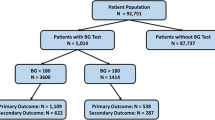
This is an additional analysis of a previously published prospective, observational cohort study (the LekCheck study). Fourteen hospitals in Europe and Australia collected perioperative data. Consecutive adult patients undergoing colorectal surgery with primary anastomosis between 2016 and 2018 were included. From all patients, preoperative diabetic status was known and intraoperative blood glucose was determined just prior to the creation of the anastomosis. The primary outcome was the occurrence of anastomotic leakage within 30 days postoperatively.
Results
Of 1474 patients (mean age 68 years), 224 patients (15%) had diabetes mellitus, 737 patients (50%) had intraoperative hyperglycemia (≥126 mg/dL, ≥7.0 mmol/L), and 129 patients (8.8%) developed anastomotic leakage. Patients with intraoperative hyperglycemia had higher anastomotic leakage rates compared to patients with a normal blood glucose level (12% versus 5%, P<0.001). Anastomotic leakage rate did not significantly differ between diabetic and non-diabetic patients (12% versus 8%, P=0.058). Logistic regression analyses showed that higher blood glucose levels were associated with an increasing leakage risk in non-diabetic patients only.
Conclusion
Incidence and severity of intraoperative hyperglycemia are associated with anastomotic leakage in non-diabetic patients. Whether hyperglycemia is an epiphenomenon, a marker for other risk factors or a potential modifiable risk factor per se for anastomotic leakage requires future research.



Similar content being viewed by others
Abbreviations
- BG:
-
Blood glucose
- CAL:
-
Colorectal anastomotic leakage
- ERAS:
-
Enhanced recovery after surgery
References
Levy N, Dhatariya K. Pre-operative optimisation of the surgical patient with diagnosed and undiagnosed diabetes: a practical review. Anaesthesia 2019;74 Suppl 1:58-66.
Jackson RS, Amdur RL, White JC, Macsata RA. Hyperglycemia is associated with increased risk of morbidity and mortality after colectomy for cancer. J Am Coll Surg 2012;214(1):68-80.
Kiran RP, Turina M, Hammel J, Fazio V. The clinical significance of an elevated postoperative glucose value in nondiabetic patients after colorectal surgery: evidence for the need for tight glucose control? Ann Surg 2013;258(4):599-5.
Huisman DE, Reudink M, van Rooijen SJ, Bootsma BT, van de Brug T, Stens J, et al. LekCheck: A Prospective Study to Identify Perioperative Modifiable Risk Factors for Anastomotic Leakage in Colorectal Surgery. Ann Surg 2020 Jun 4.
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 2015;102(5):462-479.
Gessler B, Eriksson O, Angenete E. Diagnosis, treatment, and consequences of anastomotic leakage in colorectal surgery. Int J Colorectal Dis 2017;32(4):549-556.
Bakker IS, Grossmann I, Henneman D, Havenga K, Wiggers T. Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. Br J Surg 2014;101(4):424-32; discussion 432.
McArdle CS, McMillan DC, Hole DJ. Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 2005;92(9):1150-1154.
Lin X, Li J, Chen W, Wei F, Ying M, Wei W, et al. Diabetes and risk of anastomotic leakage after gastrointestinal surgery. J Surg Res 2015;196(2):294-301.
Cong ZJ, Fu CG, Wang HT, Liu LJ, Zhang W, Wang H. Influencing factors of symptomatic anastomotic leakage after anterior resection of the rectum for cancer. World J Surg 2009;33(6):1292-1297.
Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care 1999;2(1):69-78.
Gianotti L, Sandini M, Romagnoli S, Carli F, Ljungqvist O. Enhanced recovery programs in gastrointestinal surgery: Actions to promote optimal perioperative nutritional and metabolic care. Clin Nutr 2019.
Duggan EW, Carlson K, Umpierrez GE. Perioperative Hyperglycemia Management: An Update. Anesthesiology 2017;126(3):547-560.
Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008;248(2):189-198.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS((R))) Society Recommendations: 2018. World J Surg 2019;43(3):659-695.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37 Suppl 1:81.
World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: a report of a WHO/IDF consultation. 2006:1-50.
Reisinger KW, Poeze M, Hulsewe KW, van Acker BA, van Bijnen AA, Hoofwijk AG, et al. Accurate prediction of anastomotic leakage after colorectal surgery using plasma markers for intestinal damage and inflammation. J Am Coll Surg 2014;219(4):744-751.
Kotagal M, Symons RG, Hirsch IB, Umpierrez GE, Dellinger EP, Farrokhi ET, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg 2015;261(1):97-103.
Margonis GA, Amini N, Sasaki K, Kim Y, Merath K, Buettner S, et al. Perioperative Hyperglycemia and Postoperative Outcomes in Patients Undergoing Resection of Colorectal Liver Metastases. J Gastrointest Surg 2017;21(2):228-237.
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 2013;257(1):8-14.
Davis G, Fayfman M, Reyes-Umpierrez D, Hafeez S, Pasquel FJ, Vellanki P, et al. Stress hyperglycemia in general surgery: Why should we care? J Diabetes Complications 2018;32(3):305-309.
Ljungqvist O. Jonathan E. Rhoads lecture 2011: Insulin resistance and enhanced recovery after surgery. JPEN J Parenter Enteral Nutr 2012;36(4):389-398.
Bansal N. Prediabetes diagnosis and treatment: A review. World J Diabetes 2015;6(2):296-303.
Bloomgarden ZT. Approaches to treatment of pre-diabetes and obesity and promising new approaches to type 2 diabetes. Diabetes Care 2008;31(7):1461-1466.
Sorensen BM, Houben AJ, Berendschot TT, Schouten JS, Kroon AA, van der Kallen, C. J., et al. Prediabetes and Type 2 Diabetes Are Associated With Generalized Microvascular Dysfunction: The Maastricht Study. Circulation 2016;134(18):1339-1352.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998;15(7):539-553.
Lohsiriwat V, Pongsanguansuk W, Lertakyamanee N, Lohsiriwat D. Impact of metabolic syndrome on the short-term outcomes of colorectal cancer surgery. Dis Colon Rectum 2010;53(2):186-191.
Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J. Haemoglobin A1c as a predictor of postoperative hyperglycaemia and complications after major colorectal surgery. Br J Surg 2009;96(11):1358-1364.
Goodenough CJ, Liang MK, Nguyen MT, Nguyen DH, Holihan JL, Alawadi ZM, et al. Preoperative Glycosylated Hemoglobin and Postoperative Glucose Together Predict Major Complications after Abdominal Surgery. J Am Coll Surg 2015;221(4):854-61.e1.
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001;345(19):1359-1367.
NICE-SUGAR Study Investigators for the Australian and New Zealand Intensive Care Society Clinical Trials Group and the Canadian Critical Care Trials Group, Finfer S, Chittock D, Li Y, Foster D, Dhingra V, et al. Intensive versus conventional glucose control in critically ill patients with traumatic brain injury: long-term follow-up of a subgroup of patients from the NICE-SUGAR study. Intensive Care Med 2015;41(6):1037-1047.
Kao LS, Meeks D, Moyer VA, Lally KP. Peri-operative glycaemic control regimens for preventing surgical site infections in adults. Cochrane Database Syst Rev 2009;(3):CD006806.
Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology 2015;123(6):1455-1472.
Duncan AE. Hyperglycemia and perioperative glucose management. Curr Pharm Des 2012;18(38):6195-6203.
Knaak C, Wollersheim T, Mörgeli R, Spies C, Vorderwülbecke G, Windmann V, et al. Risk Factors of Intraoperative Dysglycemia in Elderly Surgical Patients. Int J Med Sci 2019;16(5):665-674.
Le HT, Harris NS, Estilong AJ, Olson A, Rice MJ. Blood glucose measurement in the intensive care unit: what is the best method? J Diabetes Sci Technol 2013;7(2):489-499.
Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth 2013;110(2):191-200.
Acknowledgements
The authors thank Dr. M.R. Scheltinga, surgeon at Máxima Medical Center, Veldhoven, the Netherlands, for critically reviewing the manuscript and Dr. J. Dieleman, epidemiologist also at Máxima Medical Center, for her assistance with the statistical analyses. This project was supported by the Taskforce Anastomotic Leakage, the Netherlands.
Collaborators
The LekCheck study group
W. Bleeker (Wilhelmina Ziekenhuis, Assen, The Netherlands), B.T. Bootsma (VU Medical Center Amsterdam, Amsterdam, The Netherlands), F. Daams (VU Medical Center Amsterdam, The Netherlands), C.V. Feo (Ospedale del Delta, Lagosanto, Ferrara, Italy), M.J. van Hoogstraten (Bernhoven, Uden, The Netherlands), D.E. Huisman (VU Medical Center Amsterdam, The Netherlands), A. Jongen (Maastricht University Medical Center, The Netherlands), N. Komen (Antwerp University Hospital, Antwerp, Belgium), H. M. Kroon (Royal Adelaide Hospital, Adelaide, Australia), E.A.A.G.L. Lagae (ZorgSaam, Terneuzen, The Netherlands), M. Reudink (Máxima Medical Center, Veldhoven, The Netherlands), S.J. van Rooijen (Maastricht University, Maastricht, The Netherlands), R.M.H. Roumen (Máxima Medical Center, Veldhoven, The Netherlands), T. Sammour (Royal Adelaide Hospital, Adelaide, Australia), G.D. Slooter (Máxima Medical Center, Veldhoven, The Netherlands), D.J.A. Sonneveld (Dijklander Ziekenhuis, Hoorn, The Netherlands), L.P.S. Stassen (Maastricht University Medical Center, The Netherlands), A.K. Talsma (Deventer Ziekenhuis, Deventer, The Netherlands), S. Targa (Antwerp University Hospital, Antwerp, Belgium), S.C. Veltkamp (Amstelland Ziekenhuis, Amstelveen, The Netherlands), E.G.G. Verdaasdonk (Jeroen Bosch Ziekenhuis, Den Bosch, The Netherlands), T.S. de Vries Reilingh (Elkerliek Ziekenhuis, Helmond, The Netherlands), B. van Wely MD (Bernhoven, Uden, The Netherlands), J.A. Wegdam (Elkerliek Ziekenhuis, Helmond, The Netherlands).
Author information
Authors and Affiliations
Consortia
Contributions
DH, SR, AL, HK, RR, FD, and GD made substantial contributions to conception and study design. MR, DH, and SR made substantial contributions to the acquisition and/or analysis of data. MR and DH interpreted the data. MR and DH primarily drafted the manuscript. AL, SR, HK, RR, FD, and GD critically revised it for important intellectual content. All authors gave final approval for this version to be published. Finally, all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Reudink, M., Huisman, D.E., van Rooijen, S.J. et al. Association Between Intraoperative Blood Glucose and Anastomotic Leakage in Colorectal Surgery. J Gastrointest Surg 25, 2619–2627 (2021). https://doi.org/10.1007/s11605-021-04933-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-04933-2