Abstract
Background
Hepatocellular adenoma (HA) is a rare benign liver tumor with increasing incidence affecting young women. In the last years, much has changed in diagnosis, classification, and treatment, due to the identification of different molecular subtypes. With the evolving knowledge, especially on molecular characteristics of the disease, we are far from a consensus of how to deal with such a multifaceted benign disease
Methods
In the last 20 years, we have treated 134 patients with HA with a mean age of 28 years, being 126 women. Fifty patients had a history of abdominal pain and 13 patients had an acute episode of pain due to rupture and bleeding. Until 2009, adenomas larger than 4 cm in diameter were resected, regardless of gender. From 2010 to 2016, only adenomas larger than 5 cm were referred for surgical treatment. Since 2016, resection was indicated in all female patients with non-steatotic adenomas larger than 5 cm and all adenomas in men.
Results and Discussion
One hundred twenty-four patients were submitted to resection, being in 21 major resections. Since 2010, 74% of resections were done laparoscopically. Patients with ruptured adenomas were treated with transarterial embolization. Morbidity rate was 8.1% with no mortality. Authors discuss point-by-point all the aspects and presentations of the disease and the best approach. We proposed a therapeutic guideline based on the best available evidence and in our experience.
Conclusions
Due to the complexity of the disease, the treatment of HA is one the best examples of an individualized approach.


Similar content being viewed by others
References
Bioulac-Sage P, Blanc JF, Rebouissou S, Balabaud C, Zucman-Rossi J. Genotype phenotype classification of hepatocellular adenoma. World J Gastroenterol 2007;13:2649–2654.
Bioulac-Sage P, Laumonier H, Couchy G, Le Bail B, Sa Cunha A, Rullier A, Laurent C, Blanc JF, Cubel G, Trillaud H, Zucman-Rossi J, Balabaud C, Saric J. Hepatocellular adenoma management and phenotypic classification: the Bordeaux experience. Hepatology 2009;50:481–489.
Bioulac-Sage P, Laumonier H, Laurent C, Zucman-Rossi J, Balabaud C. Hepatocellular adenoma: what is new in 2008?. Hepatol Int 2008;2:316–321.
Herman P, Pugliese V, Machado MA, Montagnini AL, Salem MZ, Bacchella T, D'Albuquerque LA, Saad WA, Machado MC, Pinotti HW. Hepatic adenoma and focal nodular hyperplasia: differential diagnosis and treatment. World J Surg 2000;24:372–376.
Rooks JB, Ory HW, Ishak KG, Strauss LT, Greenspan JR, Hill AP, Tyler CW Jr. Epidemiology of hepatocellular adenoma. The role of oral contraceptive use. JAMA 1979;242:644–648.
Laurent A, Dokmak S, Nault JC, Pruvot FR, Fabre JM, Letoublon C, Bachellier P, Capussotti L, Farges O, Mabrut JY, Le Treut YP, Ayav A, Suc B, Soubrane O, Mentha G, Popescu I, Montorsi M, Demartines N, Belghiti J, Torzilli G, Cherqui D, Hardwigsen J; AFC-HCA-2013 Study Group. European experience of 573 liver resections for hepatocellular adenoma: a cross-sectional study by the AFC-HCA-2013 study groupHPB (Oxford). 2016;18(9):748-55.
Klompenhouwer AJ, Bröker MEE, Thomeer MGJ, Gaspersz MP, de Man RA, IJzermans JNM. BJS 2017;104:1695–1703.
Gevers TJG, Marcel Spanier BW, Veendrick PB, Vrolijk JM. Regression of hepatocellular adenoma after bariatric surgery in severe obese patientsLiver Int. 2018;38(12):2134-2136.
Bioulac-Sage P, Balabaud C, Bedossa P, Scoazec JY, Chiche L, Dhillon AP, Ferrell L, Paradis V, Roskams T, Vilgrain V, Wanless IR, Zucman-Rossi J; Laennec and Elves groups. Pathological diagnosis of liver cell adenoma and focal nodular hyperplasia: Bordeaux update. J Hepatol 2007;46:521-527.
Dokmak S, Paradis V, Vilgrain V, Sauvanet A, Farges O, Valla D, Bedossa P, Belghiti J. A single-centre surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology 2009;137:1698–1705.
Cho SW, Marsh W, Steel J, Holloway SE, Heckman JT, Ochoa ER, David A Geller, T Clark Gamblin. Surgical management of hepatocellular adenoma: take it or leave it? Ann Surg Oncol 2008;15:2795–2803.
Deneve JL, Pawlik TM, Cunningham S, Clary B, Reddy S, Scoggins CR, Martin RC, D'Angelica M, Staley CA, Choti MA, Jarnagin WR, Schulick RD, Kooby DA. Liver cell adenoma: a multicentre analysis of risk factors for rupture and malignancy. Ann Surg Oncol 2009;16:640–648.
Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors – from molecular classification to personalized clinical care. Gastroenterology 2013;144: 888–902.
Aseni P, Sansalone CV, Sammartino C, Benedetto FD, Carrafiello G, Giacomoni A, Osio C, Vertemati M, Forti D. Rapid disappearance of hepatic adenoma after contraceptive withdrawal. J Clin Gastroenterol 2001;33:234–236.
Edmondson HA, Reynolds TB, Henderson B. Regression of liver cell adenomas associated with oral contraceptives. Ann Intern Med 1977;86:180–182.
Marks WH, Thompson N, Appleman H. Failure of hepatic adenomas to regress after discontinuance of oral contraceptives. An association with focal nodular hyperplasia and uterine leiomyoma. Ann Surg 1988;208:190–195.
Farges O, Dokmak S. Malignant transformation of liver adenoma: an analysis of the literature. Dig Surg. 2010;27(1):32–38.
Farges O, Ferreira N, Dokmak S, Belghiti J, Bedossa P, Paradis V. Changing trends in malignant transformation of hepatocellular adenoma Gut. 2011;60(1):85-9.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines on the management of benign liver tumours. J Hepatol 2016;65:386–398.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–247.
Bioulac-Sage P, Cubel G, Taouji S, Scoazec JY, Leteurtre E, Paradis V, Sturm N, Nhieu JT, Wendum D, Bancel B, Ramos J, Paraf F, Saint Paul MC, Michalak S, Fabre M, Guettier C, Le Bail B, Zucman-Rossi J, Balabaud C. Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am J Surg Pathol 2012;36:1691–1699.
Miller GC, Campbell CM, Manoharan B, Bryant R, Cavallucci D, O'Rourke N, Clouston AD. Subclassification of hepatocellular adenomas: practical considerations in the implementation of the Bordeaux criteria. Pathology 2018;50(6):593–599.
Nault JC, Paradis V, Cherqui D, Vilgrain V, Zucman-Rossi J. Molecular classification of hepatocellular adenoma in clinical practice. Journal of Hepatology 2017;67:1074–1083.
Zucman-Rossi J, Jeannot E, Nhieu JT, Scoazec JY, Guettier C, Rebouissou S, Bacq Y, Leteurtre E, Paradis V, Michalak S, Wendum D, Chiche L, Fabre M, Mellottee L, Laurent C, Partensky C, Castaing D, Zafrani ES, Laurent-Puig P, Balabaud C, Bioulac-Sage P. Genotype–phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology 2006;43:515–524.
Stoot JH, Coelen RJ, De Jong MC, Dejong CH. Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford) 2010;12:509–522.
Nault JC, Couchy G, Balabaud C, Morcrette G, Caruso S, Blanc JF, Bacq Y, Calderaro J, Paradis V, Ramos J, Scoazec JY, Gnemmi V, Sturm N, Guettier C, Fabre M, Savier E, Chiche L, Labrune P , Zucman-Rossi J. Molecular Classification of Hepatocellular Adenoma Associates With Risk Factors, Bleeding, and Malignant Transformation. Gastroenterology 2017;152:880-894.
van Aalten SM, de Man RA, IJzermans JN, Terkivatan T. Systematic review of haemorrhage and rupture of hepatocellular adenomas. Br J Surg 2012;99:911–916.
Dokmak S, Cauchy F, Belghiti J. Resection, transplantation and local regional therapies for liver adenomas Expert Rev Gastroenterol Hepatol. 2014;8(7):803-10.
Putra J, Ferrell LD, Gouw ASH, Paradis V, Rishi A, Sempoux C, Balabaud C, Thung SN, Bioulac-Sage P. Malignant Transformation of Liver Fatty Acid Binding Protein-Deficient Hepatocellular Adenomas: Histopathologic Spectrum of a Rare Phenomenon. Mod Pathol 2020;33(4):665-675.
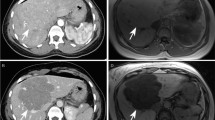
Laumonier H, Bioulac-Sage P, Laurent C, Zucman-Rossi J, Balabaud C,Trillaud H. Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification. Hepatology 2008;48:808–818.
Ronot M, Bahrami S, Calderaro J, Valla DC, Bedossa P, Belghiti J, Vilgrain V, Paradis V. Hepatocellular adenomas: accuracy of magnetic resonance imaging and liver biopsy in subtype classification. Hepatology 2011;53:1182–1191.
van Aalten SM, Thomeer MG, Terkivatan T. Hepatocellular adenomas: correlation of MR imaging findings with pathologic subtype classification. Radiology 2011;261:172–181.
Grazioli L, Olivetti L, Mazza G, Bondioni MP. MR imaging of hepatocellular adenomas and differential diagnosis dilemma. Int J Hepatol 2013:374170.
Bise S, Frulio N, Hocquelet A, Alberti N, Blanc JF, Laurent C, Laumonier H, Balabaud C, Bioulac-Sage P, Trillaud H. New MRI features improve subtype classification of hepatocellular adenoma. Eur J Radiol 2019; 29(5):2436-2447.
McInnes MD, Hibbert RM, Inácio JR, Schieda N. Focal Nodular Hyperplasia and Hepatocellular Adenoma: Accuracy of Gadoxetic Acid-enhanced MR Imaging-A Systematic Review Radiology 2015;277(2):413-23.
Dokmak S, Belghiti J. Will weight loss become a future treatment of hepatocellular adenoma in obese patients? Liver Int. 2015;35:2228-2232.
Herman P, Coelho FF, Perini MV, Lupinacci RM, D'Albuquerque LAC, Cecconello I. Hepatocellular adenoma: an excellent indication for laparoscopic liver resection. HPB 2012;14:390–395.
Herman P, Krüger J, Lupinacci R, Coelho F, Perini M. Laparoscopic bisegmentectomy 6 and 7 using a Glissonian approach and a half-Pringle maneuverSurg Endosc. 2013 May;27(5):1840-1.
Coelho FF, Kruger JA, Fonseca GM, Araújo RL, Jeismann VB, Perini MV, Lupinacci RM, Cecconello I, Herman P. Laparoscopic liver resection: Experience based guidelines. World J Gastrointest Surg. 2016;27;8(1):5-26.
van Rosmalen BV, Coelen RJS, Bieze M , M. van Delden OM, Verheij J, Dejong CHC, van Gulik TM. Br J Surg 2017;106(10):1362-1371.
Erdogan D, Busch OR, van Delden OM, ten Kate FJ, Gouma DJ, van Gulik TM. Management of spontaneous haemorrhage and rupture of hepatocellular adenomas. A single centre experience. Liver Int 2006;26:433–438.
Huurman VA, Schaapherder AF. Management of ruptured hepatocellular adenoma. Dig Surg 2010;27:56–60.
Darnis B, Rode A, Mohkam K, Ducerf C, Mabrut JY. Management of bleeding liver tumors. J Visc Surg 2014;151:365–375.
Dokmak S, Aussilhou B, Rasoaherinomenjanahary F, Ronot M, Dahdouh R, Ftériche FS, Cauchy F, Paradis V, Belghiti J, Soubrane O. Hemorrhage of hepatocellular adenoma: a complication that can be treated by conservative management without surgery. HPB (Oxford) 2018;20:1198-1205.
Agrawal S, Arnason T, Saini S, Jain S, Belghiti J. Management of hepatocellular adenoma: recent advances. HPB (Oxford) 2015;17:228.
Silva, J P, Klooster B, Tsai S, Christians KK, Clarke CN, Moga H, Gamblin TC. Elective Regional Therapy Treatment for Hepatic Adenoma. Annals of Surgical Oncology 2019;26(1):125-130.
Smolock AR, Cristescu MM, Potretzke TA, Ziemlewicz TJ, Lubner MG, Hinshaw JL, Brace CL, Lee FT Jr. Microwave Ablation for the Treatment of Hepatic Adenomas. J Vasc Interv Radiol. 2016;27(2):244-9.
Chiche L, David A, Adam R, Oliverius MM, Klempnauer J, Vibert E, Colledan M, Lerut J, Mazzafero V, Di-Sandro S, Laurent C, Scuderi V, Suc B, Troisi R, Bachelier P, Dumortier J, Gugenheim J, Mabrut JY, Gonzalez-Pinto I, Pruvot FR, Le-Treut YP, Navarro F, Ortiz-de-Urbina J, Salame E, Spada M, Bioulac-Sage P. Liver Transplantation for Adenomatosis: European Experience. Liver Transplantation 2016;22:516-526 2016.
Cobey FC, Salem RR. A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management. Am J Surg 2004;187:181-191.
Bioulac-Sage P, Taouji S, Possenti L, Balabaud C. Hepatocellular adenoma subtypes: the impact of overweight and obesity. Liver Int 2012;32(8):1217-21.
Gaspersz MP, Klompenhouwer AJ, Broker MEE, Thomeer MGJ, van Aalten SM, Steegers E, Terkivatan T, Koning H, Ijzermans JNM. Growth of hepatocellular adenoma during pregnancy: A prospective study. J Hepatol 2020;72(1):119-124.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Herman, P., Fonseca, G.M., Kruger, J.A.P. et al. Guidelines for the Treatment of Hepatocellular Adenoma in the Era of Molecular Biology: An Experience-Based Surgeons’ Perspective. J Gastrointest Surg 25, 1494–1502 (2021). https://doi.org/10.1007/s11605-020-04724-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04724-1