Abstract
Patients (85%) with hepatocellular adenoma (HCA) are women taking oral contraceptives. They can be divided into four subgroups according to their genotype/phenotype features. (1) Hepatocyte nuclear factor 1α (HNF1α) biallelic somatic mutations are observed in 35% of the HCA cases. It occurs in almost all cases in women. HNF1α-mutated HCA are most of the time, highly steatotic, with a lack of expression of liver fatty acid binding protein (LFABP) in immunohistochemistry analyses. Adenomatosis is frequently detected in this context. An HNF1α germline mutation is observed in less than 5% of HCA cases and can be associated with MODY 3 diabetes. (2) An activating β-catenin mutation was found in 10% of HCA. These β-catenin activated HCAs are observed in men and women, and specific risk factors, such as male hormone administration or glycogenosis, are associated with their development. Immunohistochemistry studies show that these HCAs overexpress β-catenin (nuclear and cytoplasmic) and glutamine synthetase. This group of tumours has a higher risk of malignant transformation into hepatocellular carcinoma. (3) Inflammatory HCAs are observed in 40% of the cases, and they are most frequent in women but are also found in men. Lesions are characterised by inflammatory infiltrates, dystrophic arteries, sinusoidal dilatation and ductular reaction. They express serum amyloid A and C-reactive protein. In this group, GGT is frequently elevated, with a biological inflammatory syndrome present. Also, there are more overweight patients in this group. An additional 10% of inflammatory HCAs express β-catenin, and are also at risk of malignant transformation. (4) Currently, less than 10% of HCAs are unclassified. It is hoped that in the near future it will be possible with clinical, biological and imaging data to predict in which of the 2 major groups (HNF1α-mutated HCA and inflammatory HCA) the patient belongs and to propose better guidelines in terms of surveillance and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the West, hepatocellular adenoma (HCA) is a rare tumour that usually develops in women following oral contraceptive use for a period of more than 2 years. After the 2005 Bordeaux update on benign hepatocellular nodules [1], we have identified new molecular features associated with HCA, which have modified our understanding [2].
HCAs are associated with molecular features
Hepatocellular adenomas are monoclonal tumours [3, 4] in which several mutations have been identified.
The transcription factor 1 (TCF1) gene
The TCF1 gene encodes the hepatocyte nuclear factor 1α (HNF1α). HNF1α has been identified as a human tumour suppressor gene involved in liver tumourigenesis [5]. Indeed biallelic inactivating mutations of this gene were observed in many HCAs and few hepatocellular carcinomas (HCC). The TCF1 gene maps to chromosome 12q24.2, and encodes the hepatocyte nuclear factor 1α (HNF1α), a transcription factor involved in hepatocyte differentiation. HNF1α controls the expression of liver-specific genes, such as albumin. In mice, loss of HNF1α activity was associated with the development of fatty liver, hepatomegaly, hepatocyte dysplasia and proliferation [6]. In HCA tumours harbouring HNF1α mutations, we observed (a) a repression of gluconeogenesis coordinated with an activation of glycolysis, citrate shuttle and fatty acid synthesis, which may lead to elevated rates of lipogenesis [7] and (b) a silencing of L-FABP, which encodes liver fatty acid binding protein 1, suggesting that impaired fatty acid trafficking may also contribute to the fatty phenotype ([7] and see below).
β-Catenin gene
Chen et al. [8], and later our group, identified a β-catenin-activating mutation in a few HCA cases [9, 10]. We have not observed any HCA cases with both β-catenin mutations and biallelic inactivation of HNF1α, suggesting that these two tumourigenic pathways are mutually exclusive. The β-catenin mutation leads to the activation of the Wnt/β-catenin pathway that plays a key role in liver physiological phenomena, such as lineage specification, differentiation, stem cell renewal, epithelial-mesenchymal transition, zonation, proliferation, cell adhesion and liver regeneration [2]. Mutations of β-catenin are also found in 20–34% of hepatocellular carcinomas, suggesting that β-catenin is the most frequently activated oncogene in HCC [11]. In our series of HCAs, we showed that β-catenin-activated HCAs were more at risk of a malignant transformation than other HCA subtypes [9].
The inflammatory HCA
In these tumours, with specific pathological characteristics [4, 12], the expression of members of the acute phase inflammatory response, serum amyloid protein (SAA) and C-reactive protein (CRP), was elevated at both the mRNA and protein levels [10]. Some inflammatory HCA also demonstrate β-catenin mutation.
Is there a genetic predisposition to HCA development?
HNF1α germline mutations confer a predisposition to both diabetes (MODY3) [13, 14] and liver adenomatosis. In 1978, Foster described an association between familial adenomas and diabetes [15]. As most individuals with a germline HNF1α mutation do not develop liver tumours [14], the mutations may confer a predisposition to liver adenomatosis, with incomplete penetrance, and suggest that modifier genes may be associated with a toxic exposure factor. More than 50% of women with somatic HNF1α inactivation developed multiple adenomas, suggesting there is a yet unknown genetic predisposition to developing HCA. Recently, we identified CYP1B1 heterozygous germline inactivating mutations in 15% of women that have HNF1α-mutated HCA, suggesting that germline CYP1B1 mutations may also confer predisposition to the development of sporadic HNF1α-mutated HCA [16]. Patients presenting a familial adenomatous coli polyposis with a germline APC mutation frequently developed HCA [17].
We are not any closer to understanding the complexity of HCA formation; however, the careful analysis of molecular and clinical data should lead to new discoveries.
The genotype phenotype classification
In our institution, approximately 120 HCAs have been resected (1984–2007). Currently, the number of HCAs resected range from 5 to 10 cases/year.
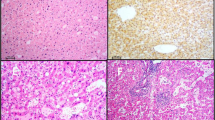
Group 1: Hepatocellular adenomas with mutations of HNF1α
HNF1α mutations are observed in approximately 30–35% of HCA. Biallelic inactivating HNF1α mutations have been identified in tumour tissues: in most cases, both mutations are of somatic origin, whereas in less than 10% of the cases, one mutation is germline and the other is somatic. Correlations with pathological and clinical data have shown that HNF1α mutations are mostly observed in a histologically homogeneous group of tumours, characterised by marked steatosis, no cytological abnormalities, no inflammatory infiltrates and a lack of LFABP expression in the tumour. Patients with germline HNF1α mutations were younger than those with somatic mutations, with or without clinical diabetes, and they frequently had a family history of liver adenomatosis [9, 10].
Group 2: Hepatocellular adenomas with mutations of the β-catenin gene
In our series, about 10% of HCAs demonstrated an activating β-catenin gene mutation. Correlations with corresponding pathological and clinical data have shown that tumours in which β-catenin is mutated are usually characterised by the occurrence of cytological abnormalities and acinar pattern, whereas they are less frequently steatotic and without inflammatory features [9]. Nuclear and cytoplasmic β-catenin staining is often heterogeneous, whereas glutamine synthetase is often more diffusely expressed. HCA with mutated β-catenin are more frequently interpreted as borderline lesions between HCA and HCC, and are more frequently associated with the development of unequivocal HCC than other HCA subtypes [9, 10, 18]. Specific risk factors are often found, such as male hormone administration, glycogenosis and familial polyposis, enhancing the proportion of male patients. However, death linked to HCC was a concern for women in this HCA group.
Group 3: Hepatocellular adenomas with inflammatory features
This group (40–50%) of HCA is characterised by the presence of inflammatory infiltrates, sinusoidal dilatation, dystrophic vessels and ductular reaction [4, 12]. They express inflammatory acute phase proteins such as SAA and CRP [10]. This group, at least partly, corresponds to a newly characterised entity, previously called telangiectatic FNH by Wanless et al. [19], which is a variant of HCA; this variant is often designated as inflammatory and/or telangiectatic HCA depending upon the importance of inflammatory infiltrates and/or sinusoidal dilatation.
Approximately 10% of HCA with inflammatory features also have a mutation in the β-catenin gene (which represents 20% of total of β-catenin-mutated HCA). The risk of HCC does exist, but it appears to be lower in this group than in β-catenin-mutated HCA.
Group 4: Hepatocellular adenomas without HNF1α or β-catenin gene mutations and without the inflammatory protein expression
This group represents less than 5–10% of cases.
Also, some HCA cannot be classified if all or nearly the whole tumour is necrotic and/or haemorrhagic.
Clinical and biological implications
Somatic HNF1α-mutated HCA occur almost exclusively in women, and the discovery of adenomatosis or multiple adenomas is frequent [10]. Adenomatosis refers to the presence of multiple adenomas on imaging (>10) [20]. Steatotic adenomas (usually present in HNF1α-mutated HCA) are easier to identify by imaging techniques, and this may explain why adenomatosis in our experience appears to be more frequent in group 1 than in group 3. In fact, it is often difficult to assess the true number of adenomas, as small microadenomas are often missed by imaging (if their size is in the mm range). Microadenomas can be seen on the surface of the liver (and have so far been described only in HNF1α group) and on the resected liver. In resected liver cases, immunostaining is very useful for microadenoma identification (LFABP, SAA or CRP). It is not rare to identify other types of nodules, particularly focal nodular hyperplasia (FNH), in patients with multiple adenomas. The differential diagnosis is usually easier for haemangioma, but may be more difficult for FNH. In this context, we found that glutamine synthetase (GS) staining was useful in differentiating FNH from HCA [10].
Identifying β-catenin/GS-positive HCA is of major interest, due to the correlation between β-catenin activation and HCC risk of transformation [2, 8, 18, 21].
This study raised the possibility of using liver biopsies for the identification of the various HCA subtypes. Currently, there is no data relating to the percentage success of this technique (work in progress). It is well known how difficult it is to distinguish between dysplastic HCA exhibiting some cytonuclear abnormalities (corresponding mainly in our study to β-catenin-activated HCA) and well-differentiated HCC on a resected specimen. This is especially significant in β-catenin-activated HCA without overt associated HCC. In our experience, and with the exception of β-catenin HCA occurring in a specific context (glycogenosis, male hormone administration, etc.) independent of sex, all cases of HCC have occurred in women (β-catenin-mutated, either alone or also inflammatory), and all β-catenin-activated HCA without HCC have been found negative for glypican 3 staining (unpublished data). However, only 64% of HCC that developed on normal liver samples were positively stained by glypican 3 [22]; thus, there is a need to identify new markers of malignant transformation in β-catenin-activated HCA and therefore precisely understand the malignant transformation of this type of HCA.
Inflammatory HCA are more often associated with an increased level of GGT, and occurs more frequently in overweight patients [10, 23]. In some cases, signs of chronic anaemia of inflammation may be observed. The link between inflammation and/or anaemia is confirmed by their disappearance after surgical removal of the nodule(s) [24]. It is important to document biological abnormalities (inflammatory and metabolic syndromes) in any suspected cases of inflammatory HCA. The discovery of an inflammatory HCA in men is troublesome, particularly in those who are positive for β-catenin. Even though we have never observed an association with HCC, we cannot ignore that HCC in non-cirrhotic liver occur in a similar setting (due to the combination of metabolic syndrome, excess alcohol consumption, etc.).
Practical attitude
Hepatocellular adenoma is a rare disease occurring in young women and more rarely in men.
The significant correlation between the genotype and phenotype classification has changed our understanding of the disease.
The first interest in this classification was to identify HCA previously classified as telangiectatic FNH [4, 12] and to solve difficulties in diagnosing between HCA and FNH [1].
The second interest has been to offer available tools to classify nodules (and therefore patients), allowing a better understanding of the natural history of each subgroup, including their possible regression after menopause. Also, it sometimes allows us to predict immunopathological diagnosis on liver biopsies of the tumour, like on resected specimens, and soon we hope that imaging data will further enhance our diagnostic criteria (work in progress).
Current data are however too premature to modify, in depth, the classical rules relating to surveillance and treatment [25–28]. For now, these rules remain the same. They can be summarised as follows: stop oral contraceptives, and remove any nodule larger than 4–5 cm to avoid the risk of haemorrhage (frequent) and HCC (rare).
Regarding haemorrhage, HCAs often present radiological evidence of minimal intratumoural bleeding. Those patients may eventually be at a greater risk of major bleeding than those without.
Women with HCA are said to be at greater risk of bleeding during pregnancy. Some authors recommend avoiding pregnancy. However, this risk cannot be estimated at an individual level, and there are cases in which pregnancies have been uneventful. It seems reasonable to look for the presence of intratumoural bleeding in any discovered or known HCA in a pregnant woman, and to recommend a close follow-up using frequent ultrasound imaging.
The discovery of a small (<3 cm) β-catenin-mutated HCA is certainly a strong argument for removing it, especially in men; however, this may not be the universal recommendation, as long as we do not understand all the steps in carcinogenesis, which are probably dependent on the cause. Some causes of disease, such as glycogenosis, are at high risk of malignant transformation, and patients taking male hormones should be monitored extremely carefully once the drug has been stopped.
Table 1 summarises some general and practical aspects relating to HCAs and their differential diagnoses.
The future
Better knowledge of the various subgroups may solve many unanswered questions:
-
Is the bleeding risk the same in all groups and does it occur in nodules smaller than 3–5 cm?
-
Is the β-catenin mutation synonymous with a precancerous stage, possibly reversible if the cause is stopped, or is it a well-differentiated HCC in any case?
-
What is the risk of HCC in cases without β-catenin mutation?
-
Are all HCAs of the same subgroup (in multiple HCA/adenomatosis) exposed to a similar risk of bleeding or HCC transformation?
As HCA is a rare disease, it is important that each centre collects data which include recent information (see flow chart used in our institution). To help clinicians (hepatologists, radiologists, pathologists and surgeons), we are presently building a website, part of which will also be available to patients.
It is likely that new mutations will be discovered, increasing the specificity of the classification. Also, MRI and ultrasound (US) contrast agents will allow researchers to distinguish between the two main subgroups of HCA. Novel drug treatment should become available, and previously proposed radiological investigation therapies may be tested in the future (embolisation, radio frequency) [29, 30].
In the near future, we will be able to propose better guidelines, particularly in patients with adenomatosis that are at risk of haemorrhage (particularly troublesome in pregnant women), and for malignant transformation in two main areas: surveillance and new modalities of treatment.
References
Bioulac-Sage P, Balabaud C, Bedossa P, Scoazec JY, Chiche L, Dhillon AP, et al. Pathological diagnosis of liver cell adenoma and focal nodular hyperplasia: Bordeaux update. J Hepatol 2007;46:521–7.
Rebouissou S, Bioulac-Sage P, Zucman-Rossi J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J Hepatol 2008;48:163–70.
Paradis V, Laurent A, Flejou JF, Vidaud M, Bedossa P. Evidence for the polyclonal nature of focal nodular hyperplasia of the liver by the study of X-chromosome inactivation. Hepatology 1997;26:891–5.
Bioulac-Sage P, Rebouissou S, Sa Cunha A, Jeannot E, Lepreux S, Blanc JF, et al. Clinical, morphologic, and molecular features defining so-called telangiectatic focal nodular hyperplasias of the liver. Gastroenterology 2005;128:1211–8.
Bluteau O, Jeannot E, Bioulac-Sage P, Marques JM, Blanc JF, Bui H, et al. Bi-allelic inactivation of TCF1 in hepatic adenomas. Nat Genet 2002;32:312–5.
Pontoglio M, Barra J, Hadchouel M, Doyen A, Kress C, Bach JP, et al. Hepatocyte nuclear factor 1 inactivation results in hepatic dysfunction, phenylketonuria, and renal Fanconi syndrome. Cell 1996;84:575–85.
Rebouissou S, Imbeaud S, Balabaud C, Boulanger V, Bertrand-Michel J, Terce F, et al. HNF1alpha inactivation promotes lipogenesis in human hepatocellular adenoma independently of SREBP-1 and carbohydrate-response element-binding protein (ChREBP) activation. J Biol Chem 2007;282:14437–46.
Chen YW, Jeng YM, Yeh SH, Chen PJ. P53 gene and Wnt signaling in benign neoplasms: beta-catenin mutations in hepatic adenoma but not in focal nodular hyperplasia. Hepatology 2002;36:927–35.
Zucman-Rossi J, Jeannot E, Nhieu JT, Scoazec JY, Guettier C, Rebouissou S, et al. Genotype–phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology 2006;43:515–24.
Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Jeannot E, et al. Hepatocellular adenomas subtype classification using molecular markers and immunohistochemistry. Hepatology 2007;46:740–8.
de La Coste A, Romagnolo B, Billuart P, Renard CA, Buendia MA, Soubrane O, et al. Somatic mutations of the beta-catenin gene are frequent in mouse and human hepatocellular carcinomas. Proc Natl Acad Sci USA 1998;95:8847–51.
Paradis V, Benzekri A, Dargere D, Bieche I, Laurendeau I, Vilgrain V, et al. Telangiectatic focal nodular hyperplasia: a variant of hepatocellular adenoma. Gastroenterology 2004;126:1323–9.
Yamagata K, Oda N, Kaisaki PJ, Menzel S, Furuta H, Vaxillaire M, et al. Mutations in the hepatocyte nuclear factor-1alpha gene in maturity-onset diabetes of the young (MODY3). Nature 1996;384:455–8.
Bacq Y, Jacquemin E, Balabaud C, Jeannot E, Scotto B, Branchereau S, et al. Familial liver adenomatosis associated with hepatocyte nuclear factor 1alpha inactivation. Gastroenterology 2003;125:1470–5.
Foster JH, Berman MM. The malignant transformation of liver cell adenomas. Arch Surg 1994;129:712–7.
Jeannot E, Poussin K, Chiche L, Bacq Y, Sturm N, Scoazec JY, et al. Association of CYP1B1 germ line mutations with hepatocyte nuclear factor 1alpha-mutated hepatocellular adenoma. Cancer Res 2007;67:2611–6.
Jeannot E, Wendum D, Paye F, Mourra N, de Toma C, Fléjou JF, et al. Hepatocellular adenoma displaying a HNF1alpha inactivation in a patient with familial adenomatous polyposis coli. J Hepatol 2006;45:883–6.
Chen PJ. Genetic mutation in hepatic adenoma: seeing is believing. J Hepatol 2006;45:767–9.
Wanless IR, Albrecht S, Bilbao J, Frei JV, Heathcote EJ, Roberts EA, et al. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Mod Pathol 1989;2:456–62.
Flejou JF, Barge J, Menu Y, Degott C, Bismuth H, Potet F, et al. Liver adenomatosis. An entity distinct from liver adenoma? Gastroenterology 1985;89:1132–8.
Monga SP. Hepatic adenomas: presumed innocent until proven to be beta-catenin mutated. Hepatology 2006;43:401–4.
Wang XY, Degos F, Dubois S, Tessiore S, Allegretta M, Guttmann RD, et al. Glypican-3 expression in hepatocellular tumors: diagnostic value for preneoplastic lesions and hepatocellular carcinomas. Hum Pathol 2006;37:1435–41.
Paradis V, Champault A, Ronot M, Deschamps L, Valla DC, Vidaud D, et al. Telangiectatic adenoma: an entity associated with increased body mass index and inflammation. Hepatology 2007;46:140–6.
Sa Cunha A, Blanc JF, Lazaro E, Mellottee L, Le Bail B, Zucman-Rossi J, et al. Inflammatory syndrome with liver adenomatosis: the beneficial effects of surgical management. Gut 2007;56:307–9.
van der Windt DJ, Kok NF, Hussain SM, Zondervan PE, Alwayn IP, de Man RA, et al. Case-orientated approach to the management of hepatocellular adenoma. Br J Surg 2006;93:1495–502.
Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol 2005;39:401–12.
Gibbs JF, Litwin AM, Kahlenberg MS. Contemporary management of benign liver tumors. Surg Clin North Am 2004;84:463–80.
Chiche L, Dao T, Salame E, Galais MP, Bouvard N, Schmutz G, et al. Liver adenomatosis: reappraisal, diagnosis, and surgical management: eight new cases and review of the literature. Ann Surg 2000;231:74–81.
Kim YI, Chung JW, Park JH. Feasibility of transcatheter arterial chemoembolization for hepatic adenoma. J Vasc Interv Radiol 2007;18:862–7.
Rocourt DV, Shiels WE, Hammond S, Besner GE. Contemporary management of benign hepatic adenoma using percutaneous radiofrequency ablation. J Pediatr Surg 2006;41:1149–52.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is dedicated to a leading French hepatologist, JP Benhamou, who continues to maintain a great interest in hepatocellular adenoma.
An erratum to this article can be found at http://dx.doi.org/10.1007/s12072-008-9089-7
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bioulac-Sage, P., Laumonier, H., Laurent, C. et al. Hepatocellular adenoma: what is new in 2008. Hepatol Int 2, 316–321 (2008). https://doi.org/10.1007/s12072-008-9075-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-008-9075-0