Abstract
Background
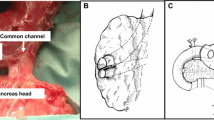
Pancreas-sparing duodenectomy (PSD) offers definitive therapy for duodenal polyposis associated with familial adenomatous polyposis (FAP). We reviewed the long-term complications of PSD and evaluated the incidence of high-grade dysplasia (HGD) and cancer in the remaining upper gastrointestinal tract.
Methods
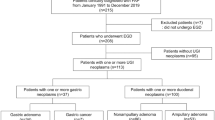
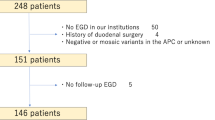
Forty-seven FAP patients with duodenal polyposis undergoing PSD from 1992 to 2019 were reviewed. Long-term was defined as > 30 days from PSD.
Results
All patients were treated with an open technique, and 43 (91.5%) had Spigelman stage III or IV duodenal polyposis. Median follow-up was 107 months (IQR, 26–147). There was no 90-day mortality. Seven patients died at a median of 10.5 years (IQR, 5.4–13.3) after PSD, with one attributed to gastric cancer. Pancreatitis occurred in 10 patients (21.3%), and two required surgical intervention. Seven patients (14.9%) developed an incisional hernia, and all underwent definitive repair. Forty-one patients (87.2%) had postoperative surveillance endoscopy over a median follow-up of 111 months (IQR, 42–138). Three patients (6.4%) developed adenocarcinoma (two gastric, one jejunal), and four (8.5%) had adenomas with HGD (two gastric, two jejunal) with a median of 15 years (IQR, 9–16) from PSD. One patient with gastric adenocarcinoma and all patients with HGD or adenocarcinoma of the jejunum required surgical intervention.
Conclusion
PSD can be performed with a low but definable risk of long-term morbidity. Risk of gastric and jejunal carcinoma rarely occurs and was diagnosed decades after PSD. This demonstrates the need for lifelong endoscopic surveillance and educates us on the risk of carcinoma in the remaining gastrointestinal tract.
Similar content being viewed by others
Abbreviations
- PSD:
-
Pancreas-sparing duodenectomy
- FAP:
-
Familial adenomatous polyposis
- APC:
-
Adenomatous polyposis coli
- BMI:
-
Body mass index
- SSI:
-
Surgical site infection
- OSI:
-
Organ space infection
- HGD:
-
High-grade dysplasia
- LGD:
-
Low-grade dysplasia
References
Bulow S, Bjork J, Christensen IJ, et al. Duodenal adenomatosis in familial adenomatous polyposis. Gut. 2004; 53: 381-86
Offerhaus GJ, Giardello FM, Krush AJ, et al. The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology. 1992; 102(6): 1980-2.
Groves CJ, Saunders BP, Spigelman AD, et al. Duodenal cancer in patients with familial adenomatous polyposis (FAP): results of a 10 year prospective study. Gut. 2002; 50(5): 636-41.
Spigelman AD, Williams CB, Talbot IC, et al. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet. 1989; 2: 783-85.
Johnson MD, Mackey R, Brown N, et al. Outcome based on management for duodenal adenomas: sporadic versus familial disease. J Gastrointest Surg. 2010; 14(2): 229-35.
Mackey R, Walsh RM, Chung R, et al. Pancreas-sparing duodenectomy is effective management for familial adenomatous polyposis. J Gastrointest Surg. 2005; 9(8): 1088-93
Kalady MF, Clary BM, Tyler DS, et al. Pancreas-preserving duodenectomy in the management of duodenal familial adenomatous polyposis. J Gastrointest Surg. 2002: 6(1): 82-7.
Walsh RM, Augustin T, Aleassa EM, et al. Comparison of pancreas-sparing duodenectomy (PSD) and pancreatoduodenectomy (PD) for the management of duodenal polyposis syndromes. Surgery. 2019; 166(4): 496-502.
Chung RS, Church JM, vanStolk R. Pancreas-sparing duodenectomy: indications, surgical technique, and results. Surgery. 1995; 117(3): 254-59.
Augustin T, Moslim MA, Tang A, et al. Tailored surgical treatment of duodenal polyposis in familial adenomatous polyposis syndrome. Surgery. 2018; 163:594-99.
Yoon JY, Mehta N, Burke CA, et al. The Prevalence and Significance of Jejunal and Duodenal Bulb Polyposis After Duodenectomy in Familial Adenomatous Polyposis: Retrospective Cohort Study. Ann Surg. 2019; in press.
Ganschow P, Hackert T, Biegler M, et al. Postoperative outcome and quality of life after surgery for FAP-associated duodenal adenomatosis. Langenbecks Arch Surg. 2018; 403(1): 93-102.
Mankaney G, Leone P, Cruise M, et al. Gastric cancer in FAP: a concerning rise in incidence. Fam Cancer. 2017; 16(3): 371-6.
Fink C, Baumann P, Wente MN, et al. Incisional hernia rate 3 years after midline laparotomy. Br J Surg. 2014; 101(2): 51-4.
Deerenberg EB, Harlaar JJ, Steyerberg EW, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet. 2015; 386(10000): 1254-1260.
Diener MK, Voss S, Jensen K, et al. Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg. 2010; 251(5): 843-56.
Itatsu K, Yokoyama Y, Sugawara G, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014; 101(11): 1439-47.
Al-Sarireh B, Ghaneh P, Gardner-Thorpe J, et al. Complications and follow-up after pancreas-preserving total duodenectomy for duodenal polyps. Br J Surg. 2008; 95(12): 1506-11.
D’Angelica M, Maddineni S, Fong Y, et al. Optimal abdominal incision for partial hepatectomy: increased late complications with Mercedes-type incisions compared to extended right subcostal incisions. World J Surg. 2006; 30(3): 410-18.
Donataccio M, Genco B, Donataccio D. Right subcostal incision in liver transplantation: prospective study of feasibility. Transplant Proc. 2006; 38(4): 1109-10.
Nakayama Y, Konishi M, Gotohda N, et al. Comparison of postoperative early and late complications between pancreas-sparing duodenectomy and pancreatoduodenectomy. Surg Today. 2017; 47(6): 705-11.
Author information
Authors and Affiliations
Contributions
Authors meet all 4 criteria for authorship as described by the International Committee of Medical Journal Editors (ICMJE).
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naples, R., Simon, R., Moslim, M. et al. Long-Term Outcomes of Pancreas-Sparing Duodenectomy for Duodenal Polyposis in Familial Adenomatous Polyposis Syndrome. J Gastrointest Surg 25, 1233–1240 (2021). https://doi.org/10.1007/s11605-020-04621-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04621-7